Abstract
Cross-sectional studies suggest that cognitive deficits contribute to psychosocial impairment among individuals with mood disorders. However, studies examining whether cognition prospectively predicts psychosocial outcome are few, have employed short follow-up periods, and have not demonstrated incremental validity (i.e., that cognition predicts future functioning even when controlling for baseline functioning). In a sample of 51 individuals with unipolar depression or bipolar disorder, we investigated whether attention/processing speed (APS) performance predicted social functioning 18 years later. Baseline APS predicted 18-year social functioning even after controlling for baseline social functioning and depressive symptoms, demonstrating incremental validity. Individuals with high baseline APS had stable social functioning over 18 years, while functioning deteriorated among those with low APS. This finding helps clarify the temporal order of cognitive and psychosocial deficits associated with mood disorders, and suggests the clinical utility of cognitive measures in identifying those at risk for deterioration in social functioning.
Keywords: Depression, Bipolar Disorder, Neuropsychology, Social Functioning
Depression is the fourth leading worldwide cause of disease burden (Üstün et al., 2004). Among other difficulties, individuals with depression have poor interpersonal functioning (Joiner and Timmons, 2009; Segrin, 1990). However, the specific mechanisms through which depression impairs social functioning have not been fully elucidated.
One pathway through which depression may impair social functioning is neurocognition. Cognitive impairment is a feature of both unipolar and bipolar depression, and many depressed individuals experience deficits in cognition even during symptom remission (Austin et al., 2001; Bhardwaj et al., 2010; Kurtz and Gerraty, 2009). Cognitive deficits predict functional impairment in several disorders, most notably schizophrenia (Hseih et al., 2011; Milev et al., 2005).
Several recent studies of individuals with bipolar disorder have reported cross-sectional associations of executive functioning, verbal memory, and attention/processing speed (APS) with psychosocial functioning (Burdick et al., 2010; Godard et al., 2011; Martino et al., 2011; Solé et al., 2012). A smaller number of studies of unipolar depression have also reported that cognition in several domains, including APS, predicts concurrent psychosocial functioning (Fennig et al., 2002; Jaeger et al., 2006). Finally, among individuals with geriatric unipolar depression, executive dysfunction has been linked to impairment in instrumental activities of daily living (e.g., preparing meals, taking medicine; Cahn-Weiner et al., 2000; Kiosses and Alexopoulos, 2005; Kiosses et al., 2000, 2001).
A limitation of this literature is that most studies have employed cross-sectional designs. A prospective study linking cognitive impairment to future functional outcome would help clarify the temporal relationships among depression, cognition, and functioning. Moreover, a finding that cognition prospectively predicts functional outcome would have important clinical implications, for instance suggesting that preventative interventions should target individuals with poor cognition before psychosocial functioning deteriorates. One prospective study of unipolar depression found that deficits in motor skills, visual memory, and perceptual reasoning during hospitalization predicted functioning six months later (Jaeger et al., 2006). However, these measures were also correlated with functioning at baseline, and the study did not examine whether baseline cognitive ability predicted later functioning over and above baseline functioning. Therefore, although this finding does support a stable association between cognition and functioning, it does not establish whether cognitive measures have incremental validity as predictors of functioning. Demonstrating incremental validity is important because if cognition does not predict future functioning over and above current functioning, it would have limited clinical utility. A longer follow-up period may be needed to show that cognition incrementally predicts future functioning.
The primary aim of the present study was therefore to investigate whether a critical cognitive domain, APS, predicted social functioning 18 years later among individuals with unipolar and bipolar depression. APS has previously been linked to concurrent social functioning in a subset of this sample (Burdick et al., 2010). We hypothesized that baseline APS would show incremental validity in predicting social functioning 18 years later over and above baseline functioning and depressive symptoms.
Methods
Participants
The sample consisted of 51 individuals with non-psychotic unipolar depression or non-psychotic bipolar disorder drawn from the Chicago Follow-Up Study (CFUS), a longitudinal research program based at the University of Illinois College of Medicine (Burdick et al., 2006; Harrow et al., 2004). Participants were recruited from inpatient hospital psychiatric units and initially diagnosed by Research Diagnostic Criteria (Spitzer et al., 1978) for an acute depressive or manic episode using the Schedule for Affective Disorders and Schizophrenia (SADS; Endicott and Spitzer, 1978). Participants were reassessed six times (i.e., F1 – F6). The sample consists of 51 participants with data on symptoms, cognition, and functioning available at both F1 and F6. Participants with history of psychosis or more than two current manic symptoms at F1 or F6 were excluded.
The baseline for the present report was F1, which occurred two years after index hospitalization. F1 was used as the baseline because previous analyses of this dataset have indicated that cognitive performance improved markedly from index hospitalization to F1 and then remained stable for twenty years (Bonner-Jackson et al., 2010). This suggests that acute illness or other factors interfered with test performance during the hospitalization assessment, and the F1 assessment therefore provides a better estimate of participants’ abilities.
We examined functional outcome at F6, 18 years after the F1 baseline assessment. F6 is the most recent follow-up from which a sufficient number of participants had functioning data. Forty-nine individuals provided data at F1 but not at F6. These individuals did not differ from the present sample on baseline depression, APS, or social functioning.
Measures
Clinical status
Depressive symptoms were assessed at baseline and follow-up using the composite depressed mood and behavior score (subscale 12) from the Katz Adjustment Scales (KAS; Katz and Lyerly, 1963), a 55-item self-report instrument that was the precursor to the Symptom Checklist-90 (SCL-90). Manic and psychotic symptoms were also rated at each time point using the SADS.
Cognition
Attention/processing speed (APS) was measured at each time point using Digit Symbol, a subtest from the Wechsler Adult Intelligence Scale–Revised (WAIS-R; Wechsler, 1981). The WAIS-R Information subtest was used as an estimate of intellectual functioning.
Functional outcome
We assessed functional outcome using a standardized clinician-rated measures of social functioning (Strauss and Carpenter, 1972). The social functioning scale assessed the frequency and context of social interactions in the month preceding assessment on a five-point scale, ranging from “none” to “chance encounters with others” to “regularly planned meetings several times a month.”*
Data Analysis
We examined whether baseline functioning, depressive symptoms, or APS predicted social functioning or employment status at 18-year follow-up. We conducted a hierarchical linear regression in which follow-up social functioning was regressed on baseline social functioning in the first block, baseline depressive symptoms in the second block, and baseline Digit Symbol in the third block. Years of education was included as a covariate in all models.
Results
Sample characteristics at baseline and 18 years later are presented in Table 1. Unipolar and bipolar participants did not differ on depressive symptoms, APS, or social functioning at baseline or follow-up (all ps > .2).
Table 1.
Sample Characteristics
| Baseline | Follow-Up | |
|---|---|---|
| Demographics | ||
| Age at Assessment (SD) | 25.1 (3.5) | 43.5 (3.8) |
| Female | 58.8% | |
| Caucasian | 78.4% | |
| Years of Education (SD) | 14.0 (2.3) | |
| Clinical Variables | ||
| KAS Current Depressiona (SD) | 16.0 (5.4) | 14.7 (5.2) |
| Unipolar | 82.4% | 72.5% |
| Social Functioningb | 3.6 (0.8) | 3.3 (1.1) |
| Employed Full-Timeb | 72.5% | 80.4% |
| Current Medication | ||
| Antidepressant | 11.8% | 43.0% |
| Lithium | 5.9% | 9.8% |
| Antipsychotic | 11.8% | 9.8% |
| Any Psychotropic | 37.3% | 64.7% |
| Premorbid Intellectual Function | ||
| WAIS-Rc Information, Scaled (SD) | 12.1 (2.9) | 12.4 (2.5) |
KAS Current Depression = Katz Adjustment Scales, subscale 12 (depressed mood and behavior)
According to Strauss-Carpenter Outcome Scales
WAIS-R = Wechsler Adult Intelligence Scale - Revised.
Unsurprisingly, baseline social functioning predicted follow-up social functioning, R2 = .27, F(2, 48) = 8.87, p < .001. Baseline depressive symptoms did not predict follow-up social functioning, ΔR2 < .01, F < 1. However, as hypothesized, baseline APS accounted for 12% of unique variance in social functioning at follow-up, ΔR2 = .12, F(1, 46) = 8.63, p < .01. This effect remained significant even after covarying for gender, baseline or follow-up polarity, age or medication use. The effect also remained significant when not controlling for years of education. Baseline intellectual functioning and polarity at baseline or follow-up did not predict follow-up functioning, and polarity did not moderate the effect of APS on functioning (all ps > .5).
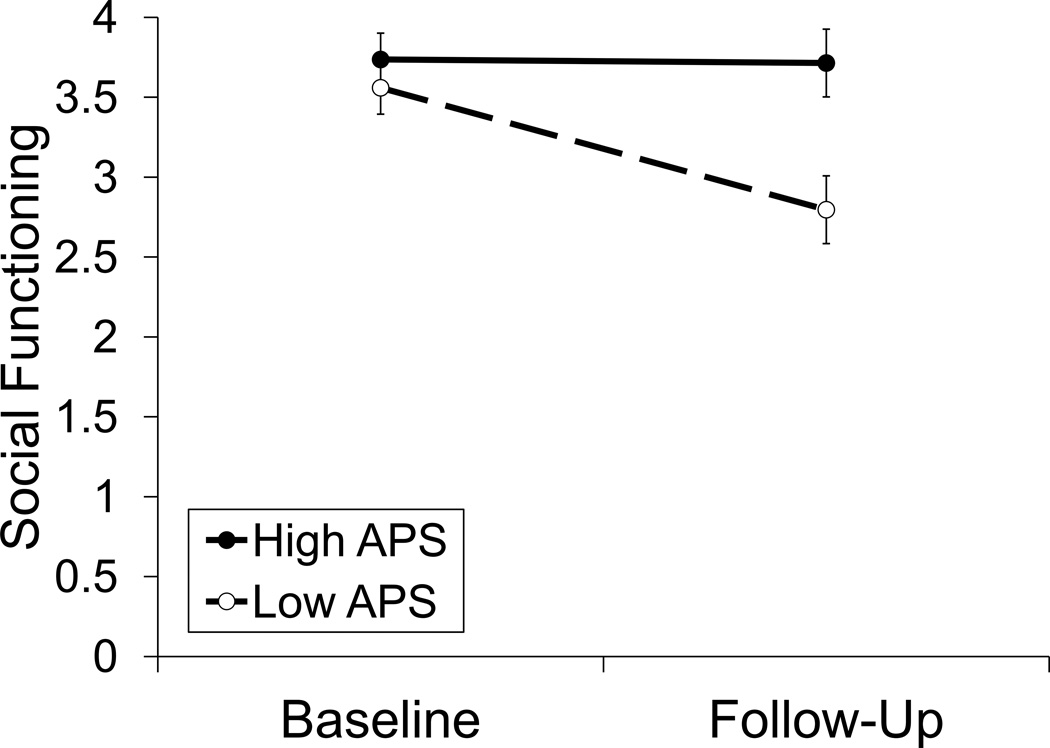
To better understand this result, we plotted simple slopes of social functioning over time at high (+1 SD) and low (−1 SD) levels of baseline APS (Figure 1). The slopes in Figure 1 do not represent groups, but rather the relative effect of time on social functioning at different levels of APS. The slopes for this figure were derived from two analyses; each analysis included a conditional moderator where 0 represented either 1 SD above or below the mean on APS. Each of these slopes was modeled in the entire sample (Aiken & West, 1991). These analyses revealed that individuals with high APS ability showed stable social functioning (effect of time, F < 1), while the social functioning of individuals with low APS decreased over time [effect of time, F(1, 48) = 14.12, p < .001].
Figure 1.
Eighteen-year trajectories of social functioning among individuals with high and low attention/processing speed (APS) performance at baseline. Error bars represent standard errors.
Discussion
Growing evidence suggests that cognitive and functional impairments in mood disorders are related, but the temporal relationship among these variables has not been established. We demonstrated that attention/processing speed performance at an early post-hospitalization follow-up predicted social functioning 18 years later. This was true even when controlling for baseline social functioning, demonstrating incremental validity for APS as a predictor of future course of social functioning. Specifically, social functioning deteriorated over time among those with poor APS but remained stable among high-APS individuals.
Poor APS may therefore be a risk factor for depression-related social deficits. Depressed individuals engage in a constellation of behaviors associated with poor social functioning. Deficits in APS may be relevant to several of these, including deficits in verbal communication skills (e.g., speaking more slowly, more softly, and with less prosody; Joiner and Timmons, 2009), as well as nonverbal skills (e.g., less gesturing, eye contact, and use of facial expression to communicate positive emotions; Segrin, 2001).
Furthermore, APS strongly influences performance in higher-order cognitive domains (Salthouse, 1996), and as such is a fundamental component of the cognitive system (Kail and Salthouse, 1994). Consistent with this, differences in APS have been shown to account for most other cognitive deficits observed in mood disorders (Antila et al., 2011). Therefore, some effects of APS on social functioning may be mediated by other cognitive domains. For instance, impairments in cognitive flexibility might be involved in perseverative social behaviors like excessive reassurance-seeking (Coyne, 1976; Joiner and Timmons, 2009) and negative feedback seeking (Swann et al., 1992).
APS’ ability to predict future social functioning independently of current functioning points to the potential clinical utility of cognitive measures. Specifically, low-APS individuals with mood disorders may be good candidates for early intervention to prevent problems in social functioning. Because social support is itself a robust predictor of depression (Grav et al., 2012) these interventions might result not only in better interpersonal functioning, but also in a more favorable overall course of illness. Indeed, interventions that promote social contact also reduce depressive symptoms (Forsman et al., 2011). The current results also suggest that efforts to treat cognitive impairment may be effective for improving social function. Consistent with this, cognitive remediation has been found to improve social functioning in schizophrenia (Twamley et al., 2003).
The present study had several limitations. First, because only one cognitive ability was assessed, we were unable to determine whether the results reflect a specific effect of APS on social functioning or a broader effect of generalized cognitive impairment. Nonetheless, the data indicate that the finding was not due to differences in intellectual ability. Second, although social functioning is an important aspect of psychosocial outcome, we did not assess other areas (e.g., recreational functioning) or more fine-grained aspects of social functioning (e.g., functioning in romantic relationships vs. friendships vs. with family members). Third, a large proportion of individuals who provided baseline data did not complete the follow-up assessment. However, individuals who did versus did not complete follow-up did not differ on depressive symptoms, APS, or social functioning at baseline, suggesting that dropout did not affect the present results. Finally, the use of an inpatient-recruited sample may reduce the generalizability of the results to less severe samples. A strength of the study is that it included a much longer follow-up period than other studies on this subject.
Conclusions
Using data from a longitudinal study, we found that attention/processing speed performance early in the course of illness predicted social functioning 18 years later. Individuals with low APS ability are at increased risk for declining social functioning. These findings are relevant for understanding the progression of functional impairment in mood disorders as well as for better targeting of preventative interventions.
Footnotes
We did not include the Strauss-Carpenter’s re-hospitalization or work functioning scales in analyses because both were highly skewed, due to few re-hospitalizations (n=5) and lack of variability in work functioning (most participants employed).
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Antila M, Kieseppä T, Partonen T, Lönnqvist J, Tuulio-Henriksson A. The effect of processing speed on cognitive functioning in patients with familial bipolar I disorder and their unaffected relatives. Psychopathology. 2011;44:40–45. doi: 10.1159/000317577. [DOI] [PubMed] [Google Scholar]
- Austin MP, Mitchell P, Goodwin GM. Cognitive deficits in depression: possible implications for functional neuropathology. Br J Psychiatry. 2001;178:200–206. doi: 10.1192/bjp.178.3.200. [DOI] [PubMed] [Google Scholar]
- Baune BT, Miller R, McAfoose J, Johnson M, Quirk F, Mitchell D. The role of cognitive impairment in general functioning in major depression. Psychiatry Res. 2011;176:183–189. doi: 10.1016/j.psychres.2008.12.001. [DOI] [PubMed] [Google Scholar]
- Bhardwaj A, Wilkinson P, Srivastava C, Sharma M. Cognitive deficits in euthymic patients with recurrent depression. J Nerv Ment Dis. 2010;198:513–515. doi: 10.1097/NMD.0b013e3181e4c5ba. [DOI] [PubMed] [Google Scholar]
- Bonner-Jackson A, Grossman LS, Harrow M, Rosen C. Neurocognition in schizophrenia: a 20-year multi-follow-up of the course of processing speed and stored knowledge. Compr Psychiatry. 2010;51:471–479. doi: 10.1016/j.comppsych.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdick KE, Goldberg JF, Harrow M. Neurocognitive dysfunction and psychosocial outcome in patients with bipolar I disorder at 15-year follow-up. Acta Psychiatr Scand. 2010;122:499–506. doi: 10.1111/j.1600-0447.2010.01590.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdick KE, Goldberg JF, Harrow M, Faull RN, Malhotra AK. Neurocognition as a stable endophenotype in bipolar disorder and schizophrenia. J Nerv Ment Dis. 2006;194:255–260. doi: 10.1097/01.nmd.0000207360.70337.7e. [DOI] [PubMed] [Google Scholar]
- Cahn-Weiner DA, Malloy PF, Boyle PA, Marran M, Salloway S. Prediction of functional status from neuropsychological tests in community-dwelling elderly individuals. Clin Neuropsychol. 2000;14:187–195. doi: 10.1076/1385-4046(200005)14:2;1-Z;FT187. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: the Schedule for Affective Disorders and Schizophrenia. Arch Gen Psychiatry. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Fennig S, Mottes A, Ricter-Levin G, Treves I, Levkovitz Y. Everyday memory and laboratory memory tests: general function predictors in schizophrenia and remitted depression. J Nerv Ment Dis. 2002;190:677–682. doi: 10.1097/00005053-200210000-00004. [DOI] [PubMed] [Google Scholar]
- Forsman AK, Nordmyr J, Wahlbeck K. Psychosocial interventions for the promotion of mental health and the prevention of depression among older adults. Health Promot Int. 2011;26(Suppl 1):85–107. doi: 10.1093/heapro/dar074. [DOI] [PubMed] [Google Scholar]
- Godard J, Grondin S, Baruch P, Lafleur MF. Psychosocial and neurocognitive profiles in depressed patients with major depressive disorder and bipolar disorder. Psychiatry Res. 2011;190:244–252. doi: 10.1016/j.psychres.2011.06.014. [DOI] [PubMed] [Google Scholar]
- Grav S, Hellzèn O, Romild U, Stordal E. Association between social support and depression in the general population: the HUNT study, a cross-sectional survey. J Clin Nurs. 2012;21:111–120. doi: 10.1111/j.1365-2702.2011.03868.x. [DOI] [PubMed] [Google Scholar]
- Harrow M, Jobe TH, Herbener ES, Goldberg JF, Kaplan KJ. Thought disorder in schizophrenia: Working memory and impaired context. J Nerv Ment Dis. 2004;192:3–11. doi: 10.1097/01.nmd.0000105994.78952.b6. [DOI] [PubMed] [Google Scholar]
- Hsieh PC, Huang HY, Wang HC, Liu YC, Bai YM, Chen KC, Yang YK. Intercorrelations between the Personal and Social Performance Scale, cognitive function, and ADLs. J Nerv Ment Dis. 2011;199:513–515. doi: 10.1097/NMD.0b013e318221447e. [DOI] [PubMed] [Google Scholar]
- Jaeger J, Berns S, Uzelac S, Davis-Conway S. Neurocognitive deficits and disability in major depressive disorder. Psychiatry Res. 2006;145:39–48. doi: 10.1016/j.psychres.2005.11.011. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Timmons KA. Depression in its interpersonal context. In: Gotlib IH, Hammen CL, editors. Handbook of Depression. 2nd ed. New York, NY: Guilford Press; 2009. pp. 322–339. [Google Scholar]
- Kail R, Salthouse TA. Processing speed as a mental capacity. Acta Psychol (Amst) 1994;86:199–225. doi: 10.1016/0001-6918(94)90003-5. [DOI] [PubMed] [Google Scholar]
- Katz MM, Lyerly SB. Methods for measuring adjustment and social behavior in the community: I. rationale, description, discriminative validity and scale development. Psychol Rep. 1963;13:503–535. [Google Scholar]
- Kiosses DN, Alexopoulos GS. IADL functions, cognitive deficits, and severity of depression: a preliminary study. Am J Geriatr Psychiatry. 2005;13:244–249. doi: 10.1176/appi.ajgp.13.3.244. [DOI] [PubMed] [Google Scholar]
- Kiosses DN, Alexopoulos GS, Murphy C. Symptoms of striatofrontal dysfunction contribute to disability in geriatric depression. Int J Geriatr Psychiatry. 2000;15:992–999. doi: 10.1002/1099-1166(200011)15:11<992::aid-gps248>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Kiosses DN, Klimstra S, Murphy C, Alexopoulos GS. Executive dysfunction and disability in elderly patients with major depression. Am J Geriatr Psychiatry. 2001;9:269–274. [PubMed] [Google Scholar]
- Kurtz MM, Gerraty RT. A meta-analytic investigation of neurocognitive deficits in bipolar illness: profile and effects of clinical state. Neuropsychology. 2009;23:551–562. doi: 10.1037/a0016277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino DJ, Igoa A, Marengo E, Scápola M, Strejilevich SA. Neurocognitive impairments and their relationship with psychosocial functioning in euthymic bipolar II disorder. J Nerv Ment Dis. 2011;199:459–464. doi: 10.1097/NMD.0b013e3182214190. [DOI] [PubMed] [Google Scholar]
- Milev P, Ho B, Arndt S, Andreasen NC. Predictive values of neurocognition and negative symptoms on functional outcome in schizophrenia: a longitudinal first-episode study with 7-year follow-up. Am J Psychiatry. 2005;162:495–506. doi: 10.1176/appi.ajp.162.3.495. [DOI] [PubMed] [Google Scholar]
- Salthouse T. The processing-speed theory of adult age differences in cognition. Psychol Rev. 1996;103:403–428. doi: 10.1037/0033-295x.103.3.403. [DOI] [PubMed] [Google Scholar]
- Segrin C. A meta-analytic review of social skill deficits in depression. Commun Monogr. 1990;57:292–308. [Google Scholar]
- Solé B, Bonnin CM, Torrent C, Balanzá-Martínez V, Tabarés-Seisdedos R, Popovic D, Martínez-Arán A, Vieta E. Neurocognitive impairment and psychosocial functioning in bipolar II disorder. Acta Psychiatr Scand. 2012;125:309–317. doi: 10.1111/j.1600-0447.2011.01759.x. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research Diagnostic Criteria: rationale and reliability. Arch Gen Psychiatry. 1978;35:773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- Strauss JS, Carpenter WT. The prediction of outcome in schizophrenia: characteristics of outcome. Arch Gen Psychiatry. 1972;27:739–746. doi: 10.1001/archpsyc.1972.01750300011002. [DOI] [PubMed] [Google Scholar]
- Swann WB, Wenzlaff RM, Krull DS, Pelham BW. Allure of negative feedback: self-verification strivings among depressed persons. J Abnorm Psychol. 1992;101:293–305. doi: 10.1037/0021-843x.101.2.293. [DOI] [PubMed] [Google Scholar]
- Twamley E, Jeste D, Belack A. Review of cognitive training in schizophrenia. Schizophr Bull. 2003;29:359–382. doi: 10.1093/oxfordjournals.schbul.a007011. [DOI] [PubMed] [Google Scholar]
- Ustün TB, Ayuso-Mateos JL, Chatterji S, Mathers C, Murray CJ. Global burden of depressive disorders in the year 2000. Br J Psychiatry. 2004;184:386–392. doi: 10.1192/bjp.184.5.386. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale - Revised. New York, NY: Psychological Corporation; 1981. [Google Scholar]