Abstract
Aplastic anaemia is a rare and serious disease characterised by severe immunosuppression due to prolonged neutropenia and the use of immunosuppressants such as corticosteroids, cyclosporine and antithymocyte globulin. Candida species are pathogens of low virulence colonising the skin and the digestive tract of many healthy individuals. Nonetheless, the incidence of invasive candidal infection is increasing. The widespread use of central intravascular catheters, invasive procedures, broad-spectrum antibiotics and immunosuppresion predisposes patients to these infections. Eye, skin, cardiac, liver, spleen and brain infection are the most common sites of invasive candidiasis. Bone and joint infections are less frequent and Candida hip septic arthritis is extremely rare. We present here a patient treated for aplastic anaemia, who developed fungal arthritis of the hip and systemic candidaemia.
Background
This case is interesting for three reasons: diagnostic difficulty and differential diagnosis with serum sickness; the issue of antifungal prophylaxis in patients treated for idiopathic aplastic anaemia; the urgency of diagnosis and its impact on treatment and survival.
Case presentation
A 55-year-old man was admitted for pancytopenia (Hb=7.6 G/dL, Plt=15 G/L, PNN=0.3×109 G/L). No blastic infiltration was observed on bone marrow examination. Medullar bone biopsy showed medullar hypoplasia. A diagnosis of aplastic anaemia was established; according to Camitta's criteria, the patient had severe aplastic anaemia.1 Before administration of the immunosupressors, he developed a high fever that was treated with piperacilline-tazobactam and levofloxacin. No bacteria, viruses or fungi were identified in blood and urine cultures. An intravenous central catheter was inserted.
After 5 days of antibiotic treatment with no fever, immunosuppressive treatment was started with antithymocyte globulin (ATG) 3.5 mg/kg, days 1–5, cyclosporine 4 mg/kg days 5–90 and methylprednisolone 2 mg/kg days 1–5, followed by tapering of corticosteroid therapy according to the guidelines of the French Society of Bone Marrow Transplantation (SFGM).
Outcome and follow-up
Fifteen days after initiation of ATG, the patient complained of pain in the right hip with an increase of C reactive protein (CRP) to 80 mg/L. He had no fever. Serum sickness was suspected as a complication of ATG treatment. Corticosteroid therapy was increased with no change in the complete blood count.
After 22 days, the patient developed fever and CRP increased to 160 mg/L. Intravenous antibiotics were switched to ceftazidime and vancomycin. The hip pain required high doses of morphine and other pain killers. An ultrasound examination of the right hip revealed a joint effusion of 1.5 cm. Septic arthritis was diagnosed. However, no drainage of joint fluid was performed because of thrombocytopenia (15 G/L).
On day 25, the blood cultures grew Candida albicans. CRP, a measure of inflammation, increased to 643 mg/L and fibrinogen was 13 g/L. Caspofungin was started and the patient was transferred to medical intensive care.
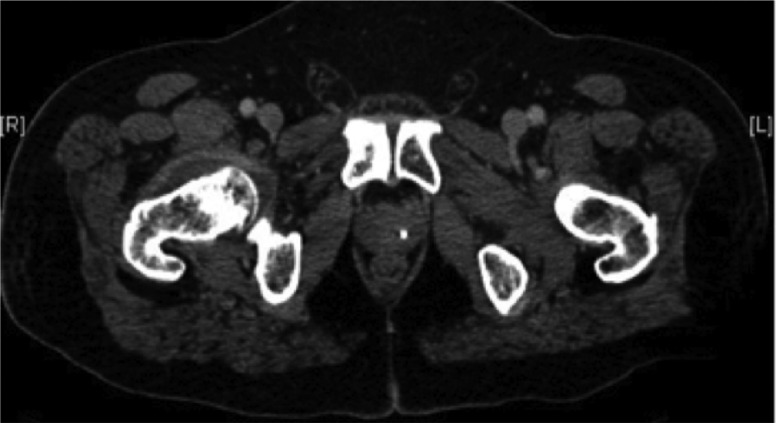
Two days later, a CT scan showed right hip effusion (figure 1). Synovial fluid aspiration was performed after platelet transfusion. C albicans was confirmed in the joint fluid. Amphotericin B was added to caspofungin. A subsequent CT of the abdomen and cytolysis showed hepatosplenic candidiasis.
Figure 1.
Transversal incidence of tomodensitometry which shows liquid effusion in right hip.
Shortly after, the patient presented with multiorgan failure: haematological, neurological (confusion), pulmonary (necessitating mechanical ventilation and oral intubation), hepatic and renal (acute renal failure necessitating dialysis). He died 37 days after initiation of ATG treatment and was still pancytopenic.
Discussion
Serum sickness is a complication of ATG treatment. It consists of a hypersensitivity reaction with formation of immune complexes (antigen-antibodies), an excess of antigens. Immune complexes are deposited in the joints. Our patient presented two major criteria of serum sickness: persistent arthralgia and symptoms occurring more than 7 days after initial administration of ATG.2 However, joint aspiration and hence diagnosis was delayed because of thrombocytopenia. Platelet transfusion above 50 G/L would have helped secure the diagnosis and antifungal treatment could have been started. Early antifungal therapy (<48 h after candidaemia) offers a higher probability of survival compared to patients with delayed treatment.3
Candida species is the fourth most common bloodstream infection and is the leading cause of invasive fungal infection among hospitalised patients.4 Acute disseminated candidiasis remains as a life-threatening disease.3 5––7 Owing to low incidence of non-specific symptoms, a long delay between exposure to risk factors and/or candidaemia and the onset of symptoms, candida arthritis is a problematic diagnosis. Invasive candidiasis is rare in the general population (approximately 8 episodes/100 000 person-years),8 but they are a dreaded complication in intensive care units, where they represent 10–15% of nosocomial infections. Mortality rates are 40–60%.3 Candida can have 200 species.3 C albicans, is ubiquitous and usually colonises the oropharynx, gastrointestinal tract, vagina and skin. The ability of these yeasts to become pathogenic is rather due to the immune status of the host than to any virulence factor of the yeast. Thus, Candida is responsible for invasive infections in solid organ or bone marrow transplants, patients receiving cancer chemotherapy or other immunosuppression, and is nowadays more and more frequently seen in intensive care units.3 Risk factors for candidaemia include recent surgery, intravenous nutrition, antibiotic use, corticosteroid therapy, chemotherapy, haematological malignancy, diabetes, central venous catheter4 and neutropenia.3
This case shows that although fungal arthritis is exceptional, it should be envisaged as a differential diagnosis of serum sickness (complication of ATG treatment). However no official recommendations exist regarding the therapeutic management of patients with idiopathic aplastic anaemia. Indeed, although prophylactic antifungal therapy was not recommended,4 9 it should have been considered.
Learning points.
The incidence of invasive fungal infections is increasing.
Several risk factors have been found to be associated with these infections, including the prolonged use of broad-spectrum antibiotics, chemotherapy, intravenous nutrition with fluids containing high glucose concentrations, neutropenia and central venous catheterisation.
The most important factors for the successful treatment of fungal arthritis and candidaemia are early diagnosis and prompt treatment.
Acknowledgments
The authors thank Dc Jean-Richard EVEILLARD and Dc Adrian TEMPESCUL for their daily help.
Footnotes
Contributors: RLC was involved in writing the manuscript. GG was the main physician who was involved in taking care of the patient. J-CI and J-MT were involved in reviewing the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Yoon HH, Huh SJ, Lee JH, et al. Should we still use Camitta's criteria for severe aplastic anemia? Korean J Hematol 2012;2013:126–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lundquist AL, Chari RS, Wood JH, et al. Serum sickness following rabbit antithymocyte-globulin induction in a liver transplant recipient: case report and literature review. Liver Transpl 2007;2013:647–50 [DOI] [PubMed] [Google Scholar]
- 3.Taieb F, Méchaï F, Lefort A, et al. Management of candidemia and invasive candidiasis. Rev Med Interne 2011;2013:173–80 [DOI] [PubMed] [Google Scholar]
- 4.Leenders NH, Oosterheert JJ, Ekkelenkamp MB, et al. Candidemic complications in patients with intravascular catheters colonized with Candida species: an indication for preemptive antifungal therapy? Int J Infect Dis 2011;2013:e453–8 [DOI] [PubMed] [Google Scholar]
- 5.Dewar CL, Sigler L. Fungal arthritis of the knee caused by Mycoleptodiscus indicus. Clin Rheumatol 2010;2013:1061–5 [DOI] [PubMed] [Google Scholar]
- 6.Swanson H, Hughes PA, Messer SA, et al. Candida albicans arthritis one year after successful treatment of fungemia in a healthy infant. J Pediatr 1996;2013:688–94 [DOI] [PubMed] [Google Scholar]
- 7.Bariola JR, Saccente M. Candida lusitaniae septic arthritis : case report and review of the litterature. Diagn Microbiol Infect Dis 2008;2013:61–3 [DOI] [PubMed] [Google Scholar]
- 8.Frentiu E, Petitfrere M, May T, et al. Two cases of spondylodiscitis due to Candida sp. Med Mal Infect 2007;2013:275–80 [DOI] [PubMed] [Google Scholar]
- 9.Marsh JC, Ball SE, Cavenagh J, et al. British Committee for Standards in Haematology Guidelines for the diagnosis and management of aplastic anaemia. Br J Haematol 2009;2013:43–70 [DOI] [PubMed] [Google Scholar]