Abstract
Anterior cruciate ligament (ACL) is the primary stabilizer of the knee. An impairment of any of the dynamic or static stability providing factors can lead to overload on the other factors and ultimately to deterioration of knee stability. This can result in anterior tibial translation and rupture of the ACL. The purpose of this study was to examine the influence of tibial slope on ACL injury risk on soccer players. A total of 64 elite soccer players and 45 sedentary controls were included in this longitudinal and controlled study. The angle between the tibial mid-diaphysis line and the line between the anterior and posterior edges of the medial tibial plateau was measured as the tibial slope via lateral radiographs. Individual player exposure, and injuries sustained by the participants were prospectively recorded. Eleven ACL injuries were documented during the study period. Tibial slope was not different between soccer players and sedentary controls. Tibial slope in the dominant and non-dominant legs was greater for the injured players compared to the uninjured players. The difference reached a significant level only for the dominant legs (p < 0.001). While the tibial slopes of the dominant and non-dominant legs were not different on uninjured players (p > 0.05), a higher tibial slope was observed in dominant legs of injured players (p < 0.05). Higher tibial slope on injured soccer players compared to the uninjured ones supports the idea that the tibial slope degree might be an important risk factor for ACL injury.
Key points.
Dominant legs’ tibial slopes of the injured players were significantly higher compared to the uninjured players (p < 0.001).
Higher tibial slope was determined in dominant legs compared to the non-dominant side, for the injured players (p = 0.042). Different tibial slope measures in dominant and non-dominant legs might be the result of different loading and/or adaptation patterns in soccer.
Key words: Tibial slope, knee, ACL injury, soccer, dominant leg, exercise
Introduction
Anterior cruciate ligament (ACL) injuries occur due to deterioration of tibiofemoral joint stability, which is provided by static and dynamic stabilizers. Static stability is supplied by ligaments, menisci, joint capsule and bony geometry. The dynamic stability is an integrated function of the neuromuscular system. The largest proportion of ACL injuries occur during sport activities involving deceleration, twisting, cutting or jumping. ACL injuries can occur as a result of excessive valgus stress, forced external rotation of the femur on a fixed tibia (with the knee in full extension), or forced hyperextension (Childs, 2002; Griffin et al., 2000; Hootman et al., 2007). An ACL injury leads to interruption in athletic career, and in some cases former athletic performance cannot be reached even following successful reconstruction. Therefore, evidence-based preventive interventions should be provided as at least advanced treatment approaches.
Assessment of ACL injury risk factors is the first step of preventive measures. Although the etiology of ACL injuries is still uncertain, many risk factors have been proposed (Hughes and Watkins, 2006). In addition to the individual biomechanical, anatomical and hormonal factors, environmental factors may also increase the risk of injury (Griffin et al., 2006; Hashemi et al., 2010; Hughes and Watkins, 2006; Schultz et al., 2010).
The tibial slope, which is defined as the angle between the line perpendicular to the tibial axis, and the posterior inclination of the tibial plateau, is proposed to play a role in static stability; and greater tibial slope is claimed to be one of the ACL injury risk factors in recent years (Griffin et al., 2006; Hashemi et al., 2010; Stijak et al., 2008). Increased tibial slope has been shown to lead to a larger anterior tibial translation via stress to the knee joint, and consequently inducing stretching and rupture of the ACL (Dejour and Bonnin, 1994; Griffin et al., 2006). Shelburne et al. used a musculoskeletal computer model of the lower limb to determine changes in anterior tibial translation, tibial shear force, and cruciate ligament forces that result from a change in posterior tibial slope. Tibial shear force and anterior tibial translation force increased as tibial slope was increased (Shelburne et al., 2011). Shao et al. anticipated, based on the results from their biomechanical model, that an increase in the tibial slope would increase the resulting anterior tibial translation and ligament forces in both healthy and ACL-deficient knees (Shao et al., 2011)
The aim of this study was to examine the influence of tibial slope on ACL injury risk on soccer players.
Methods
In this longitudinal and controlled study a total of 64 healthy male soccer players from the Turkish second and third division teams, and a control group consisting of 45 sedentary people were involved. None of the subjects in the control group had participated in regular sports activity. Physical characteristics of subjects are detailed in Table 1. Subjects with a history of previous knee ligament injury or abnormal findings during knee examination were excluded from the study.
Table 1.
Subjects’ characteristics. Data are means (± SD).
| Soccer players (n = 64) |
Control group (n = 45) |
|
|---|---|---|
| Age (years) | 22.7 (3.5) | 23.8 (2.0)* |
| Height (m) | 1.80 (.06) | 1.79 (.07) |
| Body weight (kg) | 74.0 (6.8) | 74.5 (9.4) |
| BMI (kg·m-2) | 22.9 (1.3) | 23.1 (1.6) |
BMI: body mass index.
* p < 0.05
The subjects were informed about testing procedures, possible risks and discomfort that might ensue, and gave their written informed consent to participate in accordance with the Helsinki Declaration (WMADH, 2000).
In the present study, lower limb dominance refers to the leg that is used for mobility, while the non-dominant limb contributes to support. Leg dominance is also defined as the preferred kicking leg from childhood, and as the preferred leg while putting on trousers.
Tibial slope measurement
In order to establish the tibial slope, lateral knee radiographs of the subjects were obtained upon the exact superposition of the femoral condyles. At least one, and in maximum three radiographs were taken for each knee. The proximal tibial anatomic axis (PTAA), which demonstrates the best correlation with the tibial shaft anatomic axis, was used as the reference (Çullu et al., 1999). PTAA was assessed with the help of two median points (midpoints between the anterior and posterior tibial cortex) marked at 5 cm distal to the tibial tuberosity, and 15 cm distal to the joint line. The angle between the tibial mid-diaphysis line, and the line between the anterior and posterior edges of the medial tibial plateau was measured as the tibial slope through manual goniometric measurements (Figure 1). Reliability, repeatability and reproducibility of this measurement was studied and found to be the best among different techniques (Çullu et al., 1999).
Figure 1.
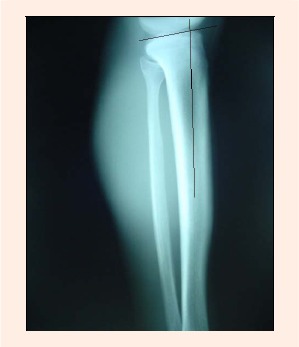
Tibial slope measurement by using the proximal tibial anatomic axis.
Follow up
Individual player exposure, and injuries sustained were prospectively recorded during the two and a half year of study period. One player exposure is defined as 1 player in 1 practice or game. The data was collected by phone calls, and/or meeting the participants and team doctors every three months. The information obtained for each injury included: date of injury, date of return to full participation, injury circumstances, injury type and location, diagnosis, injury mechanism, and treatment plans. Confidentiality of all player data was ensured.
Injury rate was defined as (total injury number/ total exposure number) x 1000.
ACL injury rate was defined as (total ACL injury number/total exposure number) x 1000 (Mihata et al., 2006).
Statistical analysis
Data was analyzed with the SPSS v15.0 programme. Subject characteristics of the groups were compared by using the unpaired t-test. Differences between dominant and non-dominant leg data in each group, and those between the data of soccer players and sedentary people were researched by using t-tests, too. Due to the non-similarity of the differences between dominant and non-dominant legs within and between the groups, an unpaired t-test was applied to compare injured and uninjured players in the assessment of tibial slope. The “Odds Ratio” was calculated as the ratio of values above and below arithmetic means for the parameters. For all analyses, a p-value less than 0.05 was considered to be statistically significant.
Results
The average ages of the soccer and control groups were 22.7 ± 3.5 and 23.8 ± 2.0 yrs, respectively. Despite choosing the subjects of both groups from the same age range of 20-30 years, there was a statistically significant difference for this parameter (Table 1). This difference seems unlikely to influence the study outcomes.
ACL injury incidence and characteristics
Overall 37598 exposures were recorded during the study period. Total injury and ACL injury rates of the soccer players are given in Table 2. Eight of the ACL injuries occurred during match play (five in the first, and three in the second halves), and three during training.
Table 2.
Total injury and ACL injury rates of the soccer player.
| Soccer players (n = 64) |
|
|---|---|
| Player exposuresa | 37598 |
| Total injury number | 442 |
| ACL injuries (percentage of total injuries) | 11 (%2.48) |
| Total injury rateb | 11.7 |
| ACL injury rateb | .29 |
a One player exposure is defined as 1 athlete in 1 practice or game.
b Rate expressed as per 1000 athlete exposures
All of the ACL injuries happened through non-contact mechanisms including landing in (n = 2), sudden deceleration (n = 1), and forced external rotation of the femur on a fixed tibia (n = 8), while the knee positioned in full or nearly full extension. In one player, both dominat and non-dominat legs sustained an ACL injury. The rest of ACL injuries were observed on the dominant side. None of the injured players declared previous injury. Seven players ended their soccer careers at the end of the second year of the study period.
Tibial slope
The tibial slope to both dominant and non-dominant legs was not different comparing soccer players and sedentary controls (p = 0.355), (Table 3).
Table 3.
Tibial slopes (°) of soccer players, of soccer players with or w/o ACL injury, and of controls according to leg dominance. Data are means (± SD).
| Dominant leg | Non-dominant leg | |
|---|---|---|
| Soccer players (n = 64) | 9.59 (2.80) | 9.58 (2.70) |
| Control group (n = 45) | 9.42 (2.81) | 8.81 (2.92) |
| Soccer players with ACL injury (n = 10) | 12.90 (2.73) | 11.25 (3.52) * |
| Soccer players w/o ACL injury (n = 54) | 8.98 (2.39) † | 9.27 (2.43) |
* p < 0.05 compared with dominant leg
† p < 0.001 compared with soccer players with ACL injury
Dominant legs’ tibial slopes of the injured players were significantly higher compared to the uninjured players (p < 0.001). However, this difference did not reach significance for the non-dominant leg (p = 0.117), (Table 3).
The tibial slopes of the dominant and non-dominant legs were not different on uninjured players (p = 0.413), (Table 3). In contrast, higher tibial slope was determined in dominant legs compared to the non-dominant side, for the injured players (p = 0.042), (Table 3). Players with tibial slope over the group mean had 5.62 times increased ACL injury risk according to the “Odds Ratio” (Table 4).
Table 4.
The effect of higher tibial slope angles on ACL injury.
| ACL injury | Total | |||
|---|---|---|---|---|
| Yes | No | |||
| Tibial | 9.58 and above | 9 | 52 | 61 |
| slope | 9.57 and below | 2 | 65 | 67 |
| Total | 11 | 117 | 128 | |
Discussion
The tibial slope is claimed to be one of the ACL injury risk factors in recent years. Limitation of static stability with increased tibial slope, and impairment of functional stability may cause ACL injury.
About 75% of ACL injuries occur with non-contact mechanisms (Arendt and Dick, 1995). Sudden deceleration, landing-in and changing direction with fixed foot, while the knee is in more extended position, are stated as possible mechanisms in ACL injuries (Kirkendall and Garret, 2000; McLean et al., 2004, 2010; Olsen et al., 2004; Yu and Garret, 2007). In the present study, all of the ACL injuries occurred with non-contact mechanisms including landing (n = 2), sudden deceleration (n = 1), and forced external rotation of the femur on a fixed tibia (n = 8), while the knee positioned in full or nearly full extension.
The ACL injury rate was 0.29/1000 in this study, this is somewhat higher in comparison to the ACL injury rates reported in the literature. From the injury surveillance system of Collegiate Athletic Association concerning collegiate soccer players, ACL injury rates were reported as 0.13/1000 (Arendt and Dick, 1995), 0.11/1000 (Agel et al., 2005), and 0.12/1000 (Mihata et al., 2006).
Eight ACL injuries happened during the match and three of them during the training. Similarly, 2-4 times higher match injuries compared with training ones were reported in previous studies (Dvorak et al., 2000; Hawkins and Fuller, 1999; Hawkins et al., 2001).
During the match, five ACL injuries occurred in the first halves and three in the second halves. Hawkins et al., 2001 reported more injuries in second halves compared to the first halves. Local muscle tiredness is known as one of the factors leading to an ACL injury. Electromechanical delay and increased anterior translation of tibia due to muscle tiredness may raise ACL injury risk (Chappell et al., 2005; Wojtys et al., 1996).
Although many measurement techniques have been proposed for tibial slope, an accepted universal standard still does not exist. Six different measurement techniques were described by investigators. Generally, there has been a consensus on medial tibial plateau as a sagittal plane reference. However, there are still different opinions about reference vertical anatomic line. In order to establish the posterior tibial slope, the angle between tibial anatomic axis and the line between the anterior and posterior edges of the medial tibial plateau is measured through lateral knee radiographs obtained upon the exact superposition of the femoral condyles. Çullu et al., 1999 demonstrated that PTAA best correlates with the tibial shaft anatomic axis. Therefore, PTAA was used in the measurement of the tibial slope in the present study.
We hypothesized, that greater tibial slope leads to increased ACL injury risk. Eleven ACL injuries occurred in ten soccer players, throughout the study. In one player, both dominant and non-dominant legs sustained an ACL injury. In nine players ACL injury happened on the dominant side. The tibial slope in dominant legs was significantly higher on injured players compared to the uninjured ones. However, this difference was out of statistical significance for the non-dominant leg. Nevertheless, higher tibial slope was observed in the dominant legs compared to the non-dominant side, in the injured players. There is still no study investigating the effect of leg dominancy on tibial slope in the current literature. Determining different tibial slope measures in dominant and non-dominant legs might be the result of different loading and/or adaptation patterns in soccer.
Measurements based on lateral radiographs yielded 10 ± 3° tibial slopes (Dejour and Bonnin, 1994). However, in this study, the tibial slope was found to be about 13° in the injured players. Players with tibial slope over the mean group value had 5.62 times increased ACL injury risk according to the “Odds Ratio” analysis. Presence of higher tibial slope in dominant legs for the injured players may point to the leg dominancy effect.
Biomechanical studies reported that higher tibial slope results in a greater anterior tibial translation (Boden et al., 2009; Dejour and Bonnin, 1994; Giffin et al., 2004). Increased tibial translation stresses the ACL structure via raised dynamic load, and consequently may cause a rupture. McLean et al., 2011 found the posterior tibial slope significantly correlated with both, peak anterior tibial acceleration and peak anteromedial bundle strain.
In the current literature seven studies compared the tibial slope in patients to noncontact ACL injury and a control group (Brandon et al., 2006; Hashemi et al., 2010; Hudek et al., 2011; Meister et al., 1998; Stijak et al., 2008; Terauchi et al., 2011; Todd et al., 2010). Terauchi et al., 2011 reported in their cross-sectional study that large posterior tibial slope is correlated with noncontact ACL injury in woman. Todd et al., 2010 found in their case-control study that subjects in the noncontact ACL group had significantly greater slope angles (9.39° ± 2.58°) than did control subjects (8.50° ± 2.67°). Hashemi et al., 2010 reported significantly increased tibial slope in injured cases compared to uninjured cases. Stijak et al., 2008 measured the tibial slope via both medial and lateral tibial plateaus in ACL ruptured cases, and in patients complaining of patellofemoral pain with no gonarthrosis. They reported higher tibial slope degrees via the lateral tibial plateau approach in ACL ruptured patients. Brandon et al., 2006 found higher tibial slopes in ACL ruptured patients, and stated that higher tibial slope increases the risk of ACL injury.
Whereas in two of these studies, comparing the tibial slope value in patients with noncontact ACL injury and a control group consisting of patients with patellofemoral pain syndrome, no difference was reported (Hudek et al., 2011; Meister et al., 1998). However, it was shown that arthritis may affect the correct measurements of tibial slope in patients who have patellofemoral pain syndrome (Hernigou et al., 1987).
As the present longitudinal study covers the data of uninjured soccer players at the begin of the study, the observation of higher tibial slope values on the players sustaining ACL injury during the study period compared to the once remaining uninjured in the same time period, may give a more realistic picture of the effect of tibial slope on ACL injury risk.
Conclusion
Higher tibial slopes in injured soccer players compared to the uninjured players may indicate a relationship between the tibial slope and ACL injury risk. However, further longitudinal studies including larger sample size are still needed to be made to clarify the absolute risk of ACL injury, including other major factors of dynamic and static stability. Preventive measures are becoming more important particularly in sports of high risk such as soccer. On players who display higher tibial slopes, additional exercises targeting enhancement of neuromuscular stability should be advised.
Biographies
Seçkin Şenişik
Employment
Ege University School of Medicine, Sports Medicine Department, Izmir, Turkey
Degree
MD
Research interests
Sports traumatology
Cengizhan Özgürbüz
Employment
Assoc. Prof., Ege University School of Medicine, Sports Medicine Department, Izmir, Turkey
Degree
MD
Research interests
Sports traumatology, exercise physiology
E-mail: cengizhan.ozgurbuz@ege.edu.tr
Metin Ergün
Employment
Assoc. Prof., Ege University School of Medicine, Sports Medicine Department, Izmir, Turkey
Degree
MD
Research interests
Sports traumatology
Oğuz Yüksel
Employment
EgeUniversity School of Medicine, Sports Medicine Department, Izmir, Turkey
Degree
MD
Research interests
Sports traumatology
Emin Taskiran
Employment
Prof., Ege University School of Medicine, Orthopedics and Traumatology Department, Izmir, Turkey
Degree
MD
Research interests
Knee surgery, sports traumatology, arthroscopy
Çetin Işlegen
Employment
Prof., Ege University School of Medicine, Sports Medicine Department, Izmir, Turkey
Degree
MD
Research interests
Exercise physiology
References
- Agel J., Arendt E.A., Bershadsky B. (2005) Anterior cruciate ligament injury in national collegiate athletic association basketball and soccer: A 13-year review. American Journal of Sports Medicine 33(4), 524-530 [DOI] [PubMed] [Google Scholar]
- Arendt E., Dick R. (1995) Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. American Journal of Sports Medicine 23, 694-701 [DOI] [PubMed] [Google Scholar]
- Boden B.P., Breit I., Sheehan F.T. (2009) Tibiofemoral alignment: contributing factors to noncontact anterior cruciate ligament injury. Journal of Bone and Joint Surgery-American Volume 91, 2381-2389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandon M.L., Haynes P.T., Bonamo J.R., Flynn M.I., Barrett G.R., Sherman M.F. (2006) The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy 22(8), 894-899 [DOI] [PubMed] [Google Scholar]
- Chappell J.D., Herman D.C., Knight B.S., Kirkendall D.T., Garrett W.E., Yu B. (2005) Effect of fatigue on knee kinetics and kinematics in stop-jump tasks. American Journal of Sports Medicine 33, 1022-1029 [DOI] [PubMed] [Google Scholar]
- Childs S.G. (2002) Pathogenesis of anterior cruciate ligament injury. Orthopaedic Nursing 21(4), 35-40 [DOI] [PubMed] [Google Scholar]
- Çullu E., Özkan Ý., Şavk Ş.Ö., Alparslan B. (1999) Tibial egim. Clinical Research 10, 174-178 (In Turkish: English abstract) [Google Scholar]
- Dejour H., Bonnin M. (1994) Tibial translation after anterior cruciate ligament rupture: Two radiological tests compared. Journal of Bone and Joint Surgery-British Volume 76(5), 745-749 [PubMed] [Google Scholar]
- Dvorak J., Peterson L., Junge A. (2000) Risk factors and incidence of injury in football players. American Journal of Sports Medicine 28, 1-74 [DOI] [PubMed] [Google Scholar]
- Giffin R.J., Vogrin M.T., Zantop T., Woo S.L.Y., Harner C.D. (2004) Effects of increasing tibial slope on the biomechanics of the knee. American Journal of Sports Medicine 32, 376-382 [DOI] [PubMed] [Google Scholar]
- Griffin L.Y., Angel J., Albohm M.J., Arendt E.A., Dick R.W., Garrett W.E., Garrick J.G., Hewett T.E., Huston L., Ireland M.L., Johnson R.J., Kibler W.B., Lephart S., Lewis J.L., Lindenfeld T.N., Mandelbaum B.R., Marchak P., Teitz C.C., Wojtys E.M. (2000) Noncontact anterior cruciate ligament injuries: risk factors and prevention strategy. Journal of the American Academy of Orthopaedic Surgeons 8(3), 141-150 [DOI] [PubMed] [Google Scholar]
- Griffin L.Y., Albohm M.J., Arendt E.A., Bahr R., Beynnon B.D., Demaio M., Dick R.W., Engebretsen L., Garrett W.E., Jr, Hannafin J.A., Hewett T.E., Huston L.J., Ireland M.L., Johnson R.J., Lephart S., Mandelbaum B.R., Mann B.J., Marks P.H., Marshall S.W., Myklebust G., Noyes F.R., Powers C., Shields C., Jr, Shultz S.J., Silvers H ., Slauterbeck J., Taylor D.C., Teitz C.C., Wojtys E.M., Yu B. (2006) Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II Meeting, January 2005. American Journal of Sports Medicine 34, 1512-1532 [DOI] [PubMed] [Google Scholar]
- Hashemi J., Chandrashekar N., Mansouri H., Gill B., Slauterbeck J.R., Schutt R.C., Jr, Dabezies E., Beynnon B.D. (2010). Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. American Journal of Sports Medicine 38, 54-62 [DOI] [PubMed] [Google Scholar]
- Hawkins R., Fuller C. (1999) A prospective epidemiological study of injuries in four English professional football clubs. British Journal of Sports Medicine 33, 196-203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins R., Hulse M., Wilkinson C., Hodson A., Gibson M. (2001) The association football medical research programme: An audit of injuries in professional football. British Journal of Sports Medicine 35, 43-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernigou P., Medevielle D., Debeyre J., Goutallier D. (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. Journal of Bone and Joint Surgery-American Volume 69(A), 332-354 [PubMed] [Google Scholar]
- Hootman J.M., Dick R., Agel J. (2007) Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. Journal of Athletic Training 42(2), 311-319 [PMC free article] [PubMed] [Google Scholar]
- Hudek R., Fuchs B., Regenfelder F., Koch P.P. (2011) Is noncontact ACL injury associated with the posterior tibial and meniscal slope? Clinical Orthopaedics and Related Research 469, 2377-2384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes G., Watkins J. (2006) A risk-factor model for anterior cruciate ligament injury. Sports Medicine 36(5), 411-428 [DOI] [PubMed] [Google Scholar]
- Kirkendall D.T., Garrett W.E., Jr (2000) The anterior cruciate ligament enigma. Injury mechanisms and prevention. Clinical Orthopaedics and Related Research 372, 64-68 [DOI] [PubMed] [Google Scholar]
- McLean S.G., Huang X., Su A., Van Den Bogert A.J. (2004) Sagittal plane biomechanics cannot injure the ACL during sidestep cutting. Clinical Biomechanics (Bristol, Avon) 19(8), 828-838 [DOI] [PubMed] [Google Scholar]
- McLean S.G., Lucey S.M., Rohrer S., Brandon C. (2010) Knee joint anatomy predicts high-risk in vivo dynamic landing knee biomechanics. Clinical Biomechanics 25, 781-788 [DOI] [PubMed] [Google Scholar]
- McLean S.G., Oh Y.K., Palmer M.L., Lucey S.M., Lucarelli D.G., Ashton-Miller J.A., Wojtys E.M. (2011) The relationship between anterior tibial acceleration, tibial slope, and ACL strain during a simulated jump landing task. The Journal of Bone and Joint Surgery 93, 1310-1317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meister K., Talley M.C., Horodyski M.B., Indelicato P.A., Hartzel J.S., Batts J. (1998) Caudal slope of the tibia and its relationship to noncontact injuries to the ACL. The American Journal of Knee Surgery 11, 217-219 [PubMed] [Google Scholar]
- Mihata L., Beutler A., Boden B. (2006) Comparing the incidence of anterior cruciate ligament injury in collegiate lacrosse, soccer and basketball players. Implications for anterior cruciate ligament mechanism and prevention. American Journal of Sports Medicine 34, 899-904 [DOI] [PubMed] [Google Scholar]
- Olsen O.E., Mykelbust G., Engebretsen L., Bahr R. (2004) Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. American Journal of Sports Medicine 32(4), 1002-1012 [DOI] [PubMed] [Google Scholar]
- Shao Q., MacLeod T.D., Manal K., Buchanan T.S. (2011) Estimation of ligament loading and anterior tibial translation in healthy and ACL-de?cient knees during gait and the in?uence of increasing tibial slope using EMG-driven approach. Annals of Biomedical Engineering 39(1), 110-121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelburne K.B., Kim H.J., Sterett W.I., Pandy M.G. (2011) Effect of posterior tibial slope on knee biomechanics during functional activity. Journal of Orthopaedic Research 29(2), 223-231 [DOI] [PubMed] [Google Scholar]
- Shultz S.J., Schmitz R.J., Nguyen A.D., Chaudhari A.M., Padua D.A., McLean S.G., Sigward S.M. (2010) ACL research retreat V: An update on ACL injury risk and prevention, March 25-27, 2010, Greensboro, NC. Journal of Athletic Training 45(5), 499-508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stijak L., Herzog R.F., Schai P. (2008) Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case-control study. Knee Surgery Sports Traumatology Arthroscopy 6, 112-117 [DOI] [PubMed] [Google Scholar]
- Terauchi M., Hatayama K., Yanagisawa S., Saito K., Takagishi K. (2011) Sagittal alignment of the knee and its relationship to noncontact anterior cruciate ligament injuries. American Journal of Sports Medicine 39, 1090-1094 [DOI] [PubMed] [Google Scholar]
- Todd M.S., Lalliss S., Garcia E., DeBerardino T.M., Cameron K.L. (2010) The relationship between posterior tibial slope and anterior cruciate ligament injuries. The American Journal of Sports Medicine 38(1), 63-67 [DOI] [PubMed] [Google Scholar]
- WMADH (2000) World Medical Association Declaration of Helsinki. The Journal of the American Medical Association 20, 3043-3045 [PubMed] [Google Scholar]
- Wojtys E.M., Wylie B.B., Huston L.J. (1996) The effects of muscle fatigue on neuromuscular function and anterior tibial translation in healthy knees. American Journal of Sports Medicine 24, 615-621 [DOI] [PubMed] [Google Scholar]
- Yu B., Garrett W.E. (2007) Mechanisms of non-contact ACL injuries. British Journal of Sports Medicine 41(Suppl. 1), i47-51 [DOI] [PMC free article] [PubMed] [Google Scholar]


