Abstract
An emphasis on increasing self-regulation is an alternate to nutrition education, which has had poor results in the behavioral treatment of obesity. Although appropriately designed weight-loss treatments may enhance one’s self-regulatory ability to control eating, whether improvements are moderated by psychosocial factors such as initial self-regulatory skills use, self-efficacy to control eating, and mood is unknown. Severely obese women (BMI 35-50 kg·m-2) were randomized into 26-week treatments of exercise supported by cognitive-behavioral methods paired with either nutrition education (n = 114) or cognitive-behavioral methods applied to controlled eating (n = 121). Improvement in self-regulation for controlled eating was 36.9% greater (p < 0.01) for the group incorporating cognitive-behavioral methods for controlled eating. Change in self-regulation was significantly associated with self-regulation at baseline (β = -0.33). Both mood and self-efficacy for controlled eating significantly moderated this relationship. Increased self-regulation was associated with both increases in fruit and vegetable consumption and fruit and vegetable intake at treatment end. The present findings increase our understanding of psychosocial variables associated with increased self-regulatory skills usage and improvements in eating that, after replication, may be used to improve the effects of behavioral weight-loss treatments.
Key points.
Initial self-regulatory abilities do not appear to affect improvements in self-regulation for eating, however direct training in behavioral skills are predictors of change.
The relationship of self-regulation improvements and improved eating is significant, and affected by mood and self-efficacy in women with obesity.
Instruction in behavioral skills such as cognitive restructuring and relapse prevention is associated with better improvements in eating than typical methods of nutrition education.
Cognitive-behavioral methods for exercise may be paired with cognitive-behavioral methods for eating to maximize longer-term effects on eating behaviors.
Key words: Behavioral treatment, cognitive-behavioral, health psychology, obesity treatment, self-regulation
Introduction
Although nutrition education is the most commonly used method for improving eating behaviors and promoting weight loss, results have been severely lacking (see Mann et al., 2007, for a review). Some research suggests that self-regulatory skills applied to controlled eating may be a much more critical factor than knowledge of appropriate principles of nutrition in the behavioral treatment of obesity (Powell et al., 2007). Interventions supporting this position typically maintain a cognitive-behavioral perspective and are likely to emphasize self-regulatory skills such as cognitive restructuring, preparing for barriers and lapses (i.e., relapse prevention), and self-monitoring incremental progress based on short-term goals. Although regular exercise is the most robust predictor of sustained weight loss (Fogelholm and Kukkomen-Harjula, 2000; Svetkey et al., 2008), and is often suggested, it has been systematically reinforced in only a few interventions. Without directed support (Annesi et al., 2011), even the minimum recommended volume of exercise (e.g., 150 minutes per week of walking; Haskell et al., 2007) is maintained by less than 4% of adults from the United States (Troiano et al., 2008; Tudor-Locke et al., 2010). It may be thought that between the adherence problem (Buckworth and Dishman, 2002), the minimal energy expenditures possible for deconditioned persons (American College of Sports Medicine, 2009), and the possibility that an individual’s limited ability to self-manage might be diluted by simultaneously undertaking exercise and changes in eating (Cooper et al., 2003), a strong emphasis on exercise is not advisable. This perception may be particularly prominent regarding individuals with severe and morbid obesity, whose participation in exercise may be especially uncomfortable, embarrassing, and aversive.
Conversely, however, recent research suggests that exercise supported by cognitive-behavioral methods may improve eating behaviors through positive effects on self-regulation, mood, and self-efficacy that carry-over to controlled eating (Annesi and Marti, 2011) - even if the volume is considerably less than official recommendations for health promotion. Our preliminary testing indicates that when treatment also focuses on improving self-regulation for controlled eating, weight management behaviors such fruit and vegetable consumption increase, and fat intake decreases, with associated weight loss significantly greater than with a more traditional treatment of nutrition education. Because this earlier research was preliminary, it was not, however, known whether a person’s initial ability to self-regulate was associated with amount of improvement in self-regulation for controlled eating, or if self-efficacy and mood moderated this relationship. It has been suggested that feelings of ability (self-efficacy) and psychological state (mood) may impact self-regulation by affecting motivation and persistence (Hagger et al., 2010).
Thus, an improved understanding of (a) the relationship of initial self-regulatory abilities with self-regulation change associated with treatment, (b) the association of self-regulatory ability with improved eating, and (c) whether self-efficacy and/or mood moderate self-regulatory change, is important because it may lead to an increased understanding of how self-regulation for controlled eating affects results of behavioral weight-loss treatment. Such knowledge may be useful for improving the architecture of future, more effective, weight-loss interventions by suggesting whether lower initial self-regulatory abilities predict greater improvements in self-regulation or, rather, self-regulatory ability is a trait-like characteristic that is resistant to change; and if mood and self-efficacy (psychological constructs theoretically malleable through treatment) affect propensities for changes in self-regulatory skill usage.
Because psychosocial correlates of controlling one’s eating differ between men and women (Tanofsky et al., 1997), it may be advisable to either study men or women separately, or include sex as a covariate in analyses of the aforementioned research questions. Because women with severe obesity (body mass index [BMI] ≥ 35 kg·m-2) have high health risks, and are most likely to turn to invasive and expensive medical methods such as bariatric surgery to reduce weight (Buchwald et al., 2004), an increased knowledge of relationships of psychological factors relevant to behavioral treatment was thought to be especially important for that subgroup. Thus, the present research assessed women with severe obesity who volunteered for a program of exercise support that was paired with either nutrition education or cognitive-behavioral methods. It was expected that change over 26 weeks in self-regulatory skills for controlled eating would be negatively associated with initial self-regulation abilities, and would improve most in a nutrition treatment with a cognitive-behavioral focus. Self-efficacy and mood were expected to significantly moderate relationships between self-regulation at baseline and change in self-regulatory skill usage. It was also expected that both change in self-regulation, and self-regulatory skills at treatment end, would be positively associated with fruit and vegetable consumption, a predictor of overall healthful eating and weight loss (Rolls et al., 2004).
Methods
Participants
Women responded to advertisements in local newspapers requesting volunteers for research incorporating physical activity and nutrition instruction for weight loss at YMCA facilities in the southeast United States. Inclusion criteria were: (a) minimum age of 21 years, (b) BMI between 35 and 50 kg·m-2, (c) no regular exercise within the previous year (less than 20 minutes per week average), and (d) a goal of weight loss. Exclusion criteria were current or planned pregnancy and taking medications for weight loss or a psychological/psychiatric condition. A written statement of adequate health to participate was required from a physician, and participants’ written informed consent was appropriately obtained. Approval was received from the Kaiser Permanente Georgia Institutional Review Board, Atlanta, Georgia.
There was no significant group difference (p > 0.10) in any assessed participant characteristic (Table 1). There was also no significant difference in racial/ethnic make-up (overall 42% white, 53% black, and 5% of other racial/ethnic groups). Nearly all participants were classified as middle-class.
Table 1.
Characteristics of participants. Data are means (±SD).
| Nutrition education group (n = 114) |
Cognitive-behavioral group (n = 121) |
Participants overall (n = 235) |
|
|---|---|---|---|
| Age (yrs) | 44.0 (9.4) | 42.0 (9.6) | 43.0 (9.5) |
| Height (m) | 1.7 (.1) | 1.7 (.1) | 1.7 (.1) |
| Weight (kg) | 111.7 (13.8) | 111.2 (13.7) | 111.5 (13.7) |
| BMI (kg·m-2) | 40.8 (4.0) | 39.5 (4.0) | 40.1 (4.1) |
| BP – systolic (mmHg) | 129.4 (14.3) | 127.7 (12.0) | 128.5 (13.2) |
| BP – diastolic (mmHg) | 82.0 (8.8) | 80.5 (9.1) | 81.2 (8.9) |
| RHR (beats/minute) | 77 (11) | 76.1 (9.2) | 76.3 (10.2) |
BP = blood pressure. RHR = resting heart rate.
Measures
Self-regulation for controlled eating was measured using a modified version of a scale by Saelens and colleagues (2000), where items are based on intervention content (see Appendix I). The scale required responses to 10 items ranging from 1 (“never”) to 5 (“often”). In a previous version, internal consistency (0.75), test-retest reliability over 2 weeks (0.77), and predictive validity were supported (Dishman et al., 2005). For the present version, the internal consistency was 0.81, and test-retest reliability was 0.74 (Annesi and Marti, 2011).
Self-efficacy for controlled eating was measured using the Weight Efficacy Lifestyle Questionnaire (see Clark et al., 1991, for items). It is made up of five subscales (Negative Emotions, Social Pressure, Availability, Physical Discomfort, and Positive Activities) of 4 items each. Responses range from 0 (“not confident”) to 9 (“very confident”). Subscale responses are summed for a total score. Internal consistencies were reported to range from 0.70 to 0.90 (Clark et al., 1991).
Overall mood was measured using Total Mood Disturbance, an aggregate measure of the Profile of Mood States Short Form (McNair and Heuchert, 2005) subscales of Tension (e.g., Anxious), Depression (e.g., Sad), Fatigue (e.g., Weary), Confusion (e.g., Bewildered), Anger (e.g., Annoyed), and Vigor (e.g., Energetic) (5 items for each subscale). Respondents rate feelings over the past week ranging from 0 (“not at all”) to 4 (“extremely”). Internal consistencies for the subscales were reported to range from 0.84 to 0.95, and test-retest reliability at 3 weeks averaged 0.69 (McNair and Heuchert, 2005).
A survey summing the number of fruits and the number of vegetables consumed “in a typical day” (“looking back over the last month”), based on the United States Food Guide Pyramid and its descriptions of foods and possible portion sizes, was used. Research suggests the adequacy of this measure for both its responsiveness in the context of the present treatments, and to minimize participant burden, thereby increasing accuracy (Kristal et al., 1994). Test-retest reliability over 2 weeks averaged 0.82, and concurrent validity was suggested through significant correlations with longer, more invasive, food frequency questionnaires (Sharma et al., 2004).
Procedure
Each participant received an orientation to study processes associated with her treatment group, and was provided access to a YMCA facility for the duration of the investigation. The exercise support protocol (i.e., Coach Approach; Annesi et al., 2011) was identically administered to both the nutrition education and cognitive-behavioral treatment groups. It consisted of six 1-hour meetings with a wellness specialist over 26 weeks. These private sessions included an orientation to exercise apparatus and facilities, however, most time was spent on cognitive-behavioral methods intended to foster adherence. For example, (a) long-term goals were identified, documented, and broken down into process-oriented short-term goals where progress was tracked graphically, (b) instruction in self-regulatory skills such as cognitive restructuring, stimulus control, self-reward, and preparedness for occurrences of barriers and lapses in exercise (i.e., relapse prevention; Marlatt and George, 2006) was provided, and (c) behavioral contracts were cooperatively derived and updated at each meeting. Specific modalities used in exercise plans (e.g., walking; stationary cycling) were based on each participant’s ability and preference. Widely used recommendations for volume of weekly exercise (150 minutes of moderate or 60 minutes of vigorous aerobic physical activity, or combinations thereof; Haskell et al., 2007) were described; however, the premise that any volume of exercise may be beneficial was also discussed.
In the nutrition education group, a standardized protocol (Kaiser Permanente Health Education Services, 2008) of six, 1-hour sessions was administered by a certified wellness specialist in a group format of approximately 15 participants. Examples of program components were: (a) understanding macronutrients, (b) using the United States Food Guide Pyramid, (c) menu planning, and (d) developing a plan for snacking. The primary focus was on participants understanding healthy eating.
In the cognitive-behavioral nutrition group, the identical administrative format of six group meetings was used, but the components differed substantially. They included: (a) establishing caloric goals and logging daily food and calorie intake, (b) behavioral contracting, (c) cognitive restructuring, (d) relapse prevention training, (e) understanding cues to overeating, and (f) relaxation strategies. The primary focus was on increasing self-regulatory skills for overcoming barriers to controlled eating. The importance of fruit and vegetable consumption was stressed throughout in both treatment conditions.
Wellness specialists administering treatments were blind to the purposes of the investigation. Compliance with treatment protocols was monitored by study investigators, and corrective measures were taken if indicated. Assessments were administered in a private area at baseline, Week 13, and Week 26.
Data analyses
An a priori power analysis for the regression procedures incorporated indicated that to detect a small-to-moderate effect size (f2 = 0.07) at the statistical power of 0.90, the minimum overall sample size required was 205 participants. Statistical significance was set at α = 0.05 (two-tailed). An intention-to-treat design was employed with multiple imputation (Kline, 2005) used for the 19% of overall missing cases. A mixed-model repeated measures analysis of variance (ANOVA) was first conducted to determine if self-regulatory skills usage for controlled eating increased over the 26-week investigation, and if that increase significantly differed between the two treatment groups. Next, using data aggregated from both groups, the bivariate relationship between change in self-regulation for controlled eating and baseline self-regulation score was assessed, after which scores on mood (mean of each participant’s Total Mood Disturbance score) and self-efficacy for controlled eating (mean of Weight Efficacy Lifestyle Questionnaire score) were evaluated for their moderation of that relationship.
To test moderation, suggestions by Baron and Kenny, 1986 and Frazier et al., 2004 were incorporated. In Step 1 of each of the corresponding multiple regression equations, the predictor and moderator were simultaneously entered. These variables were subsequently centered and standardized (X - MX/SDX) prior to being multiplied with one another to create an interaction term. This interaction term was then forced into the multiple regression equation in Step 2. If the interaction term significantly added to the variance explained in Step 1 (if the associated ∆R2 was significant), then significant moderation had been identified. Finally, self-regulation change and self-regulation at treatment end were contrasted for their strength in predicting fruit and vegetable consumption at treatment end.
Results
Attendance in the six exercise support and six nutrition sessions did not significantly differ (p > 0.50) by group (overall M = 4.2 sessions, SD = 0.9, or 70%; and overall M = 4.1 sessions, SD = 1.0, or 68%, respectively). There was also no significant difference (p = 0.32) in self-regulatory skills usage for controlled eating at baseline between the two treatment groups. The mixed-model repeated measures ANOVA indicated an overall significant increase in self-regulatory skills usage, F(1, 233) = 4893.44, p < 0.001, η2p = 0.955, with the cognitive-behavioral treatment group demonstrating a significantly greater increase (from M = 22.59, SD = 5.44 to M = 28.25, SD = 6.53) than the nutrition education group (from M = 21.86, SD = 5.71 to M = 25.43, SD = 6.63), F(1, 233) = 6.39, p = 0.01, η2p = 0.012.
The relationship between changes in self-regulation for controlled eating and baseline self-regulation was significant, and was significantly moderated by both Total Mood Disturbance (aggregated Profile of Mood States scores) and total Weight Efficacy Lifestyle Questionnaire scores (Table 2). Post hoc follow-up analyses of corresponding subscales indicated that the Profile of Mood States - Vigor; and the Weight Efficacy Lifestyle - Availability, Negative Emotions, and Physical Discomfort scores significantly moderated the relationship of self-regulation for controlled eating and baseline self-regulation.
Table 2.
Moderation analyses of Weight Efficacy Lifestyle Questionnaire and Total Mood Disturbance scores on the relationship of self-regulation for controlled eating at baseline and change in self-regulation over 26 weeks (n = 235).
| B | SEB | β | R2 | p | ΔR2 | p | |||
|---|---|---|---|---|---|---|---|---|---|
| Total Mood Disturbance as moderator | |||||||||
| Step 1 | .16 | <.001 | |||||||
| Self-regulation for controlled eating | -.36 | .06 | -.35 | <.001 | |||||
| Total Mood Disturbance | -.11 | .03 | -.26 | <.001 | |||||
| Step 2 | .18 | <.001 | .02 | .04 | |||||
| Self-regulation for controlled eating | -.35 | .06 | -.34 | <.001 | |||||
| Total Mood Disturbance | -.11 | .03 | -.26 | <.001 | |||||
| Self-regulation × Total Mood Disturbance | -.73 | .35 | -.12 | .04 | |||||
| Weight Efficacy Lifestyle as moderator | |||||||||
| Step 1 | .13 | <.001 | |||||||
| Self-regulation for controlled eating | -.35 | .07 | -.34 | <.001 | |||||
| Weight Efficacy Lifestyle | .03 | .01 | .18 | .01 | |||||
| Step 2 | .15 | <.001 | .02 | .03 | |||||
| Self-regulation for controlled eating | -.34 | .07 | -.33 | <.001 | |||||
| Weight Efficacy Lifestyle | .03 | .01 | .18 | .004 | |||||
| Self-regulation × Weight Efficacy Lifestyle | -.80 | .36 | -.14 | .03 | |||||
The relationship between self-regulation at treatment end and fruit and vegetable consumption (β = 0.38, SE = 1.91, p < 0.001) was significantly stronger, t(232) = 3.35, p = 0.001) than the relationship between self-regulation change and fruit and vegetable intake (β = 0.20, SE = 2.02, p = 0.003).
Discussion
The greater improvement in self-regulatory skills associated with the cognitive-behavioral nutrition treatment indicates that, while skills developed through focusing on self-regulation for exercise likely carry over to self-regulation for controlled eating (Annesi and Marti, 2011), additional improvements are made by adding a nutrition treatment component emphasizing self-regulatory skill development for controlled eating (rather than the more common approach of education in the principles of appropriate nutrition). The finding that increases in self-regulation were inversely related to the initial self-regulatory skill usage of participants suggests that improvement in self-regulation is not stifled by a possible trait-like personal characteristic of low ability to self-regulate. In fact, the opposite was suggested. Close inspection of the data indicated that ceiling effects did not confound the relationship. Although most research suggests that self-regulatory abilities may be enhanced (Hagger et al., 2010), an understanding of the impact of existing self-regulatory abilities was lacking. This research was useful in that regard.
Although in previous research, neither mood nor self-efficacy showed much effect on self-regulation depletion after an initial difficult task (e.g., controlling eating after utilizing self-regulatory resources for adhering to a program of exercise) (Hagger et al., 2010), their indirect effects after treatments that actively seek to promote specific self-regulatory skills, as was the case here, may be distinctly different. For example, mood and self-efficacy may affect the considerable commitment and volition required to implement and maintain new self-regulatory skills, thus the significant moderation of the relationship of initial self-regulatory skills and increases in self-regulatory skill usage found here may be logically reconciled. Within this research, the aspect of mood that was most salient was vigor (energy); and the aspects of self-efficacy for controlled eating appearing to be most remarkable were food availability, emotional eating, and eating in response to physical discomfort. These findings may be useful for tailoring treatments to address these specific areas.
Limitations of this research included its field design that reduced control over experimental artifacts such as effects of social support (e.g., from fellow participants) and expectations (e.g., from instructors). Some researchers have, however, specifically suggested such applied designs because if their high external validity, manifested by an ease in generalizing findings to professional practice and ability to rapidly affect treatments in real-life settings (Glasgow, 2008). It is also possible that participants in the cognitive-behavioral nutrition group perceived the non-conventional nature of their treatment, which may have affected their commitment. Moreover, the intervention was of a relatively brief duration. Extensions of this research using longitudinal designs are particularly needed, especially because relapses into old eating behavior patterns, resulting in regain of weight lost, are extremely common 1 to 3 years post-treatment (Mann et al., 2007). Although approximately one-third of participants, overall, obtained a reduction of at least 5% of their baseline weight, it is not known to what extent this would be maintained long term. Finally, it will be important to determine if the present findings are replicable with men, women of a lower or higher weight, and participants affected by diabetes, cancer, or bariatric surgery. The strength of the present investigation was, however, to further the sparse amount of health psychology research into the effects of initial self-regulatory ability, self-efficacy, and mood on self-regulatory skill usage and resulting improvements in eating behaviors.
Conclusion
Based on the present findings, researchers in the area of weight-loss treatment development are encouraged to attend to psychological correlates of improved eating considered here, and seek to uncover additional constructs of equal or greater importance in order to contribute in the development of interventions with improved effect and reliability. Given the high prevalence of obesity in most industrialized countries, and poor results within its behavioral treatment, innovative findings on the dynamics of the health behavior change process should play a central role in the development and widespread application of more effective interventions.
Biography
James J. Annesi
Employment
Director of Wellness Advancement for the YMCA of Metropolitan Atlanta.
Degree
PhD.
Research interests
Exercise adherence treatment, health behavior change, relations of physical activity and depression, anxiety, and self-image, and the behavioral treatment of obesity
E-mail: jamesa@ymcaatlanta.org
Appendix
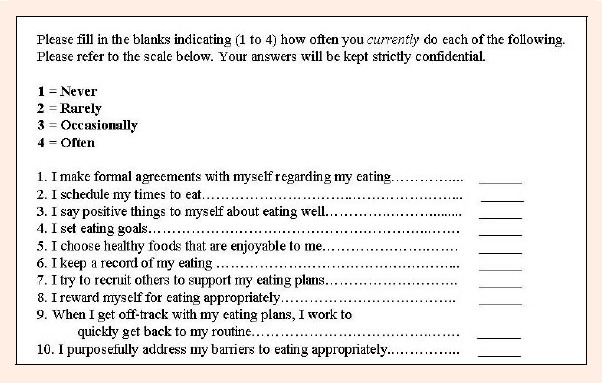
Appendix I. Self-regulation for controlled eating items.
References
- 1.American College of Sports Medicine. (2009) Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Medicine & Science in Sports & Exercise 42, 459-471 [DOI] [PubMed] [Google Scholar]
- 2.Annesi J.J., Marti C.N. (2011) Path analysis of exercise treatment-induced changes in psychological factors leading to weight loss. Psychology and Health 26(8), 1081-1098 [DOI] [PubMed] [Google Scholar]
- 3.Annesi J.J., Unruh J.L., Marti C.N., Gorjala S., Tennant G. (2011) Effects of the Coach Approach intervention on adherence to exercise in obese women: Assessing mediation of social cognitive theory factors. Research Quarterly for Exercise and Sport 28, 99-108 [DOI] [PubMed] [Google Scholar]
- 4.Baron R.M., Kenny D.A. (1986) The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology 51, 1173-1182 [DOI] [PubMed] [Google Scholar]
- 5.Buchwald H., Avidor Y., Braunwald E., Jensen M.D., Pories W., Fahrbach K., Schoelles K. (2004) Bariatric surgery: A systematic review and meta-analysis. Journal of the American Medical Association 292, 1724-1737 [DOI] [PubMed] [Google Scholar]
- 6.Buckworth J., Dishman R.K. (2002) Exercise psychology. Champaign, IL: Human Kinetics [Google Scholar]
- 7.Clark M.M., Abrams D.B., Niaura R.S., Eaton C.A., Rossi J.S. (1991) Self-efficacy in weight management. Journal of Consulting and Clinical Psychology 59, 739-744 [DOI] [PubMed] [Google Scholar]
- 8.Cooper Z., Fairburn C.G., Hawker D.M. (2003) Cognitive-behavioral treatment of obesity: A clinician’s guide. New York: Guilford [Google Scholar]
- 9.Dishman R.K., Motl R.W., Sallis J.F., Dunn A.L., Birnbaum A.S., Welk G.J., Jobe J.B. (2005) Self-management strategies mediate self-efficacy and physical activity. American Journal of Preventive Medicine 29, 10-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fogelholm M., Kukkomen-Harjula K. (2000) Does physical activity prevent weight gain - a systematic review. Obesity Reviews 1, 95-111 [DOI] [PubMed] [Google Scholar]
- 11.Frazier P.A., Tix A.P., Barron K.E. (2004) Testing moderator and mediator effects in counseling research. Journal of Consulting Psychology 51, 115-134 [Google Scholar]
- 12.Glasgow R.E. (2008) What types of evidence are most needed to advance behavioral medicine? Annals of Behavioral Medicine 35, 19-25 [DOI] [PubMed] [Google Scholar]
- 13.Hagger M.S., Wood C., Stiff C., Chatzisarantis N.L.D. (2010) Ego depletion and the strength model of self-control: A meta-analysis. Psychological Bulletin 136, 495-525 [DOI] [PubMed] [Google Scholar]
- 14.Haskell W.L., Lee I.M., Pate R.R., Powell K.E., Blair S.N., Franklin B.A., Bauman A. (2007) Physical activity and public health: Updated recommendations from the American College of Sports Medicine and the American Heart Association. Medicine & Science in Sports & Exercise 39, 1423-1434 [DOI] [PubMed] [Google Scholar]
- 15.Kaiser Permanente Health Education Services. (2008) Cultivating Health weight management kit. 8thedition Portland, OR: Kaiser Permanente [Google Scholar]
- 16.Kline R.B. (2005) Principles and practice of structural equation modelling. 2ndedition New York: Guilford [Google Scholar]
- 17.Kristal A.R., Beresford S.A.A., Lazovich D. (1994) Assessing change in diet-intervention research. American Journal of Clinical Nutrition 59(Suppl.), S185-S189 [DOI] [PubMed] [Google Scholar]
- 18.Mann T., Tomiyama J., Westling E., Lew A.M., Samuels B., Chatman J. (2007) Medicare’s search for effective obesity treatments: Diets are not the answer. American Psychologist 62, 220-233 [DOI] [PubMed] [Google Scholar]
- 19.Marlatt G.A., George W.H. (2006) Relapse prevention: Introduction and overview of the model. Addiction 79, 261-273 [DOI] [PubMed] [Google Scholar]
- 20.McNair D.M., Heuchert J.W.P. (2005) Profile of Mood States technical update. North Tonawanda, NY: Multi-Health Systems [Google Scholar]
- 21.Powell L.H., Calvin J.E., Calvin J.E. (2007) Effective obesity treatments. American Psychologist 62, 234-246 [DOI] [PubMed] [Google Scholar]
- 22.Rolls B.J., Ello-Martin J.A., Tohill B.C. (2004) What can intervention studies tell us about the relationship between fruit and vegetable consumption and weight management? Nutrition Reviews 62, 1-17 [DOI] [PubMed] [Google Scholar]
- 23.Saelens B.E., Gehrman C.A., Sallis J.F., Calfas K.J., Sarkin J.A., Caparosa S. (2000) Use of self-management strategies in a 2-year cognitive-behavioral intervention to promote physical activity. Behavior Therapy 31, 365-379 [Google Scholar]
- 24.Sharma S., Murphy S.P., Wilkens L.R., Shen L., Hankin J.H., Monroe K.R., Kolonel L.N. (2004) Adherence to the Food Guide Pyramid recommendations among African American and Latinos: Results from the Multiethnic Cohort Study. Journal of the American Dietetic Association 104, 1873-1877 [DOI] [PubMed] [Google Scholar]
- 25.Svetkey L.P., Stevens V.J., Brantley P.J., Appel L.J., Hollis J.F., Loria C.M., Aicher K. (2008) Comparison of strategies for sustaining weight loss. Journal of the American Medical Association 299, 1139-1148 [DOI] [PubMed] [Google Scholar]
- 26.Tanofsky M.B., Wilfley D.E., Spurrell E.B., Welch R., Brownell K.D. (1997) Comparison of men and women with binge eating disorder. International Journal of Eating Disorders 21, 49-54 [DOI] [PubMed] [Google Scholar]
- 27.Troiano R.P., Berrigan D., Dodd K.W., Mâsse L.C., Tilert T., McDowell M. (2008) Physical activity in the United States measured by accelerometer. Medicine & Science in Sports & Exercise 40, 181-188 [DOI] [PubMed] [Google Scholar]
- 28.Tudor-Locke C., Brashear M.M., Johnson W.D., Katzmarzyk P.T. (2010) Accelerometer profiles of physical activity and inactivity in normal weight, overweight, and obese U.S. men and women. International Journal of Behavioral Nutrition and Physical Activity 7(1), 6. [DOI] [PMC free article] [PubMed] [Google Scholar]


