Abstract
Entrapment of a microwire related to intracranial endovascular therapy is an uncommon complication. A 64-year-old man with symptomatic basilar artery stenosis was treated with stenting. A 300 cm Synchro microwire became trapped in the P1 segment of the left posterior cerebral artery during the procedure. The decision was made to leave the microwire in place, considering that aggressive retrieval procedures could cause injury to the cerebral vasculature. The entrapped microwire was later inadvertently dislocated and removed while pulling the microwire back into the femoral artery with a looped catheter from the left femoral access. This demonstrates that, although entrapment of a microwire during endovascular therapy is a rare event, an optimal salvage technique needs to be explored further.
Keywords: Atherosclerosis, Balloon, Stent, Subarachnoid
Background
Entrapment of devices related to intracranial endovascular therapy is an uncommon complication. To the best of our knowledge, in vivo entrapment of a microwire during angioplasty and stenting for intracranial stenosis has not been previously described. In this report we describe a trapped microwire related to basilar artery (BA) stenting that occurred in a patient with symptomatic stenosis and the subsequent retrieval of this device on the following morning.
Case presentation
A 64-year-old man with a history of diabetes mellitus, hyperlipidemia and active smoking presented with recurrent transient attacks of dizziness and left limb weakness for the past 2 months. His National Institute of Health Stroke Scales (NIHSS) score was 1 upon admission.
Investigations
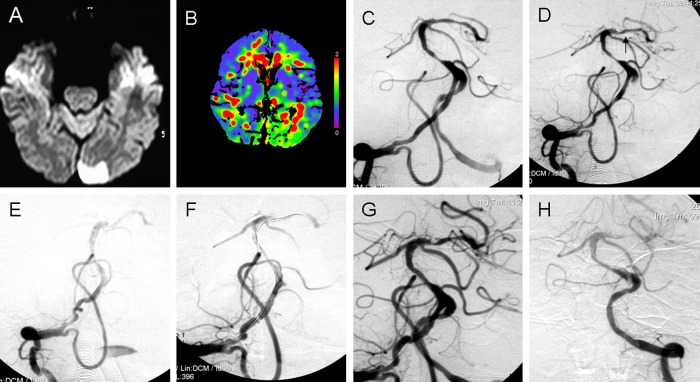
Brain MRI showed recent infarctions in the left occipital lobe and the cerebellum (figure 1A), and MR angiography demonstrated a 90% stenosis of the middle segment of the BA and right embryonic posterior cerebral artery (PCA) and absence of the left posterior communicating artery. CT perfusion demonstrated a significant perfusion deficit in the cerebellum and the left occipital lobe (figure 1B). An angiogram demonstrated a 90% stenosis of the middle segment of the BA (figure 1C) with a grade 2a thrombolysis in cerebral ischemia (TICI) score, suggesting flow-limiting stenotic BA disease. The angiogram also revealed that the bilateral vertebral arteries were equal in size and tortuosity to the V1 and V4 segments of the left vertebral artery.
Figure 1.
(A) Diffusion-weighted image showing recent infarction in the left occipital lobe. (B) CT perfusion showing prolonged mean transit time in the left lobe supplied by the stenotic basilar artery (BA). (C) Angiogram showing 90% stenosis in the middle segment of the BA. (D) After pre-dilation, an angiogram showing that the stenosis was partially resolved and that the tip of the microwire (arrow) was found outside the left posterior cerebral artery (PCA). (E) Angiogram showing that the P1 segment of the left PCA was curved and the right vertebral artery and BA were straight. (F) A pilot microwire was advanced over the lesion to the distal P1 segment of the left PCA, paralleling the entrapped Synchro microwire for implantation of an Apollo balloon-expandable stent. (G) After stenting, an angiogram showing the resolution of the stenosis. (H) The microwire tip was inadvertently dislocated from the left PCA during the manipulation to leave the microwire in place in the patient.
Treatment
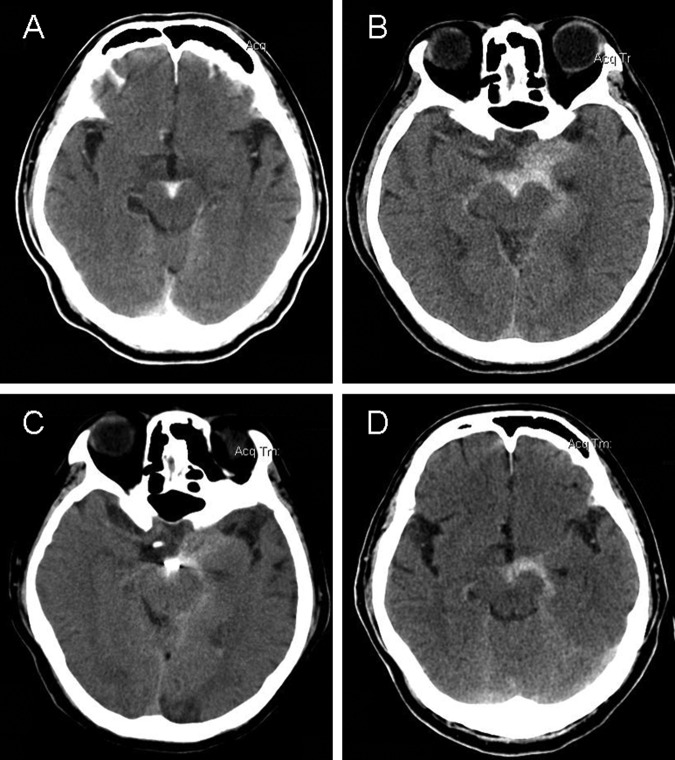
Conservative medical treatment and endovascular therapy were carefully discussed with the patient and his family. In light of his recent symptoms, endovascular revascularization of the BA stenosis was planned. Under general anesthesia, a 5 Fr guide catheter was placed into the V2 segment of the right vertebral artery. Upon visual examination it was estimated that the diameter of the BA distal to the lesion was 2.5 mm and proximal to the lesion was 3 mm, with a lesion length of 6 mm. After advancing a 300 cm Synchro microwire (Styker, West Valley City, Utah, USA) with a manually pre-formed J-shaped tip into the P1 segment of the left PCA, the BA stenosis was treated with a 2.0 mm×9 mm Gateway balloon (Styker, Maple Grove, Minnesota, USA). After pre-dilation, an angiogram showed that the stenosis was partially resolved, with a grade 2b TICI score, and that the tip of the microwire was found outside the left PCA (figure 1D). Because of the lack of contrast leaks, the entrance of the microwire tip into a perforator artery was considered. During the retrieval of the microwire, the tip became trapped in the left PCA lumen. An angiogram performed at this time demonstrated that the P1 segment of the left PCA was curved and that the right vertebral artery and BA were straight (figure 1E). It was thought that the entrapment of the microwire may have been caused by a vessel spasm so papaverine (10 mg over 3–4 min) and nimodipine (1 mg over 10 min) were administered intra-arterially through the guide catheter, but this did not result in the successful retrieval of the device. Subsequent unsuccessful attempts were then made to withdraw the microwire over a period of 20 min. An Excelsior SL-10 microcatheter (Boston Scientific, Cork, Ireland) was advanced through the microwire to provide a more stable construct against which to withdraw the microwire, but it was not able to advance past the junction of the BA and PCA. Aggressive retrieval of the microwire was not attempted to avoid arterial dissection and perforation. After stabilizing the microwire, the 5 Fr guide catheter was exchanged with a 6 Fr guide catheter. A 190 cm Pilot microwire (Abbott Vascular, Santa Clara, California, USA) was advanced over the lesion to the distal P1 segment of the left PCA, paralleling the entrapped Synchro microwire (figure 1F). A 2.5×8 mm Apollo balloon-expandable stent (MicroPort Medical, Shanghai, China) was then advanced over the Pilot microwire and deployed at the lesion. A subsequent angiogram demonstrated resolution of the stenosis and good antegrade perfusion to the BA territory with a grade 3 TICI score (figure 1G). The decision was then made to retain the groin sheath and the microwire in place temporarily for 1 day. At the time of recovery of consciousness, the patient had a headache, double vision and hemiparesis of the right limb. His NIHSS score remained at 1. A brain CT demonstrated a subarachnoid hemorrhage (SAH) (figure 2A,B). The next morning the patient's headache had disappeared and the brain CT showed improvement of the SAH (figure 2C). A new angiogram showed that the microwire remained fixed in place. Because it was believed that the microwire would be difficult to retrieve and could cause a catastrophic hemorrhage during the removal manipulations, no withdrawal attempt was made and it was decided that the microwire should be left in place. The microwire was sectioned at the groin. Because it was not possible to make the microwire end into the femoral artery by only pushing the distal end, it was decided to simultaneously pull the microwire back to the abdominal level with a looped Simmon I catheter from the left femoral access to move the proximal end of the microwire into the femoral artery. Inadvertently, the microwire tip was dislocated from the left PCA during this manipulation, during which the patient suffered a transient headache (figure 1H).
Figure 2.
(A) Brain CT showing a subarachnoid hemorrhage (SAH). (B) Brain CT 4 h later showing an increase in SAH size. (C) Brain CT the following morning showing a decrease in SAH size. (D) Brain CT after the microwire was removed showing a slight increase in SAH size.
Outcome and follow-up
The microwire remained intact after removal from the patient. A brain CT showed that the SAH size was slightly increased (figure 2D), but the patient's symptoms and NIHSS score remained stable. The patient was asymptomatic 10 days later. At his 2-month follow-up by telephone the patient maintained adherence to his prescribed medical treatment and remained asymptomatic.
Discussion
Entrapped devices related to intracranial endovascular therapy, including microcatheters following Onyx treatment of intracranial arteriovenous malformations and the Merci embolectomy device following mechanical thrombolysis, have been described.1–3 The reasons for entrapment include the glue used in microcatheters and the induction of vasospasms for the embolectomy device. However, the in vivo entrapment of a microwire has not previously been reported. The reason for entrapment in this case remains unclear, and we speculate that the tip of the microwire may have become entangled with the intima flap caused by a minor dissection as the P1 segment was found to be curved during the procedure. The SAH at the interpeduncular cistern after the procedure may be related to the rupture of perforator arteries due to the pronounced straightness of the BA and PCA.
Some reports have described various methods for retrieving a trapped microcatheter after Onyx embolization of an arteriovenous malformation, including the use of a balloon microcatheter to provide distal counter tension for the retrieval of the trapped microcatheter, the utilization of a monorail snare technique and a microsurgical retrieval method.4–6 We considered that these salvage techniques might not be suitable for retrieving entrapped microwire because the microwire is more stiff and less flexible than microcatheters. After treatment with spasmolytics and gentle removal attempts failed, the last choice was to leave the trapped microwire in place. Of note, as with all intravascular foreign bodies, the long-term retention of the microwire poses a thromboembolic risk that is particularly concerning in the cerebrovascular system.7
In this case we used spasmolytic treatments and a coaxial microcatheter technique to retrieve the trapped microwire but these were unsuccessful. We considered that it might be safe to leave the microwire in place after the prescribed retrieval attempts failed. A subsequent stenting through another microwire pressing the trapped microwire against the lumen wall at the stenosis was necessary, as this increases forward blood flow and decreases the acute thrombus risk. Fortunately, the microwire was retrieved unintentionally during the attempt to move the distal end of the microwire in the femoral artery.
Based on this case, we feel that an optimal salvage technique needs to be explored. For prevention of this fairly rare event, monitoring the movement of the microwire J-shaped tip to ensure its position within the true lumen during any maneuver is critical.
Conclusion
The complication of entrapment of a microwire during endovascular therapy is a rare occurrence. An optimal salvage technique needs to be explored.
Learning points.
The in vivo entrapment of microwire during endovascular therapy has not been previously reported.
A potential complication of endovascular therapy with basilar artery stenting is microwire entrapment.
An optimal salvage technique needs to be explored.
Footnotes
Contributors: Analysis and interpretation of data: Z-RM, NM, LL, T-JW and X-TX. Drafting of this report: NM and Z-RM.
Competing interests: None.
Patient consent: Obtained.
Ethics approval: Ethical Committee of Beijing Tiantan Hospital.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Natarajan SK, Ghodke B, Britz GW, et al. Multimodality treatment of brain arteriovenous malformations with microsurgery after embolization with Onyx: single-center experience and technical nuances. Neurosurgery 2008;2013:1213–25; discussion 1225–6 [DOI] [PubMed] [Google Scholar]
- 2.Weber W, Kis B, Siekmann R, et al. Endovascular treatment of intracranial arteriovenous malformations with Onyx : technical aspects. AJNR Am J Neuroradiol 2007;2013:371–7 [PMC free article] [PubMed] [Google Scholar]
- 3.Gordhan A, Soliman J. In vivo retrieval of a trapped Merci embolectomy device: technical case report. Neurosurgery 2010;2013(3 Suppl Operative):ONSE304. [DOI] [PubMed] [Google Scholar]
- 4.Santillan A, Zink W, Knopman J, et al. Balloon-assisted technique for trapped microcatheter retrieval following Onyx embolization. A case report. Interv Neuroradiol 2009;2013:453–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kelly ME, Turner R, Gonugunta V, et al. Monorail snare technique for the retrieval of an adherent microcatheter from an Onyx cast: technical case report. Neurosurgery 2008;2013(1 Suppl 1):ONSE89. [DOI] [PubMed] [Google Scholar]
- 6.Walcott BP, Gerrard JL, Nogueira RG, et al. Microsurgical retrieval of an endovascular microcatheter trapped during Onyx embolization of a cerebral arteriovenous malformation. J Neurointerv Surg 2011;2013:77–9 [DOI] [PubMed] [Google Scholar]
- 7.Lee JI, Choi CH, Ko JK, et al. Retained microcatheter after Onyx embolization of intracranial arteriovenous malformation. J Korean Neurosurg Soc 2012;2013:374–6 [DOI] [PMC free article] [PubMed] [Google Scholar]