Abstract
We present a case of a fisherman who swallowed a live fish, which resulted in severe upper airway obstruction. The firm attachments of the fish's external fins and scales to the airway limit the removal when impacted. We outline our emergency airway management strategies and focus our discussion on the technique used to remove the impacted fish from the upper airway, which was paramount for the successful outcome of this case.
Background
Airway obstruction from the ingestion of a live fish is rare and usually fatal. The anatomy of a fish presents several challenges to anyone trying to remove it from the airway along its longitudinal axis. The firm attachments of the fish's external fins and scales to the oesophageal and tracheal mucosa limit the removal when impacted. We present a case of a fisherman who swallowed a live fish, which resulted in total upper airway obstruction. We outline our emergency airway management strategies, and focus our discussion on the technique used to remove the impacted fish from the upper airway, which was a paramount for the successful outcome of this case.
Case presentation
A fit 22-year-old man went fishing with friends in rural New South Wales, Australia. To celebrate his first catch of the day, the fisherman opened his mouth with his tongue protruding, and kissed the live fish. While doing so, the fish slipped through his fingers and lodged in his hypopharynx. He immediately developed symptoms of upper airway obstruction and respiratory distress. Bystanders attempted to remove the fish but failed, resulting in the fishing line and part of the tail breaking off. The fisherman collapsed and was transported by friends to the nearest district hospital in the country town of Barham, located 10 min away. Barham has an approximate population of 1200 people. The Barham Hospital has eight acute and one accident and emergency beds.
Treatment
On arrival, the patient was cyanosed, with oxygen saturations of 80%, and was unable to talk with signs of severe upper airway obstruction. The hospital medical officer performed an emergency needle cricothyrotomy using two 14-gauge intravenous cannulae, and 100% oxygen was delivered through both cannulae. The patient was then immediately transferred to Kerang district hospital, located 15 min away in the bordering state of Victoria. Kerang Hospital is a regional hospital with community medical and surgical care, obstetrics, community nursing, day care and aged care services. With a population of less than 4000, there was only one general practitioner with postgraduate training in anaesthesia, who was summoned urgently. On his arrival, the patient was tachycardic, hypertensive and hypoxic with oxygen saturations varying between 82% and 88%. Over the next 5 min, the patient became profoundly cyanosed and unconscious. Attempts at intubation using a standard Macintosh Size 3 blade failed as the oropharynx was completely obscured by the body of the fish. Blind orotracheal intubation using a size 4 microlaryngoscopy endotracheal tube was successfully performed by careful advancement of the microlaryngoscopy tube lateral to the body of the fish towards the anticipated direction of the vocal cords. Clinical signs of bilateral chest movement, positive breath sounds on auscultation and fogging of the endotracheal tube confirmed correct endotracheal placement. Once the airway was secured, the patient was paralysed with vecuronium (0.1 mg/kg) and ventilated with 100% oxygen. The patient was then immediately transferred to a regional tertiary centre in Bendigo, located 129 km (80 miles) away, by a specialist retrieval team.
In the operating room at Bendigo Hospital, a Doughty tongue blade stabiliser retractor (Kaiser Surgical Instruments, Lifehealthcare, Western Australia) and a Davis Boyle mouth gag (Kaiser Surgical Instruments, Lifehealthcare), employed in surgery for tonsillectomies, were inserted into the patient's mouth and manipulated into a position that enabled good visualisation of the fish in the upper airway (figure 1). Portable image intensification confirmed that the 14-gauge cannulae had penetrated the cricothyroid membrane and demonstrated the fishhook in situ, in the region that corresponds anatomically to the upper trachea (figure 2). Oesophagoscopy then revealed the fish obstructing the hypopharynx. The fish could not to be removed en bloc due to firm attachments of the external spines and fins to the oesophageal and hypopharygeal mucosa. Coring out the centre of the fish with a 19 cm Ruskin bone rongeur (Kaiser Surgical Instruments, Lifehealthcare) enabled scissors to be passed down the sides of the fish to cut the spines and free the fish from the upper oesophagus (figure 3). The remaining spines, fins and scales were then individually removed from the mucosa. Once the fish was removed, the microlaryngosocopy endotracheal tube was exchanged for a size 9.0 endotracheal tube and the patient transferred to an intensive care unit.
Figure 1.
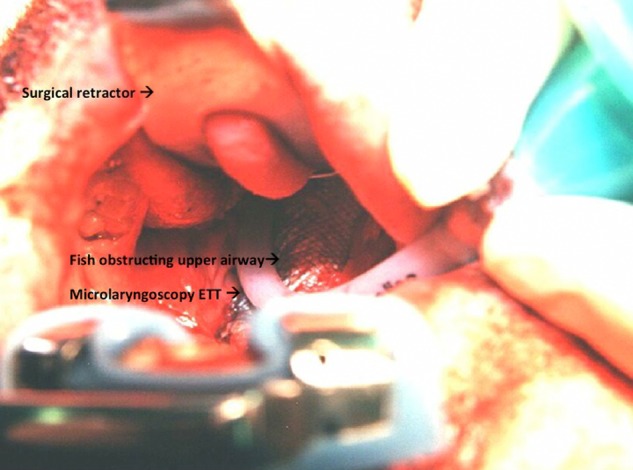
The fish obstructing the hypopharynx of the upper airway. The airway is visualized after a stabiliser retractor employed in surgery for tonsillectomies was inserted into the airway. ETT, endotracheal tube.
Figure 2.
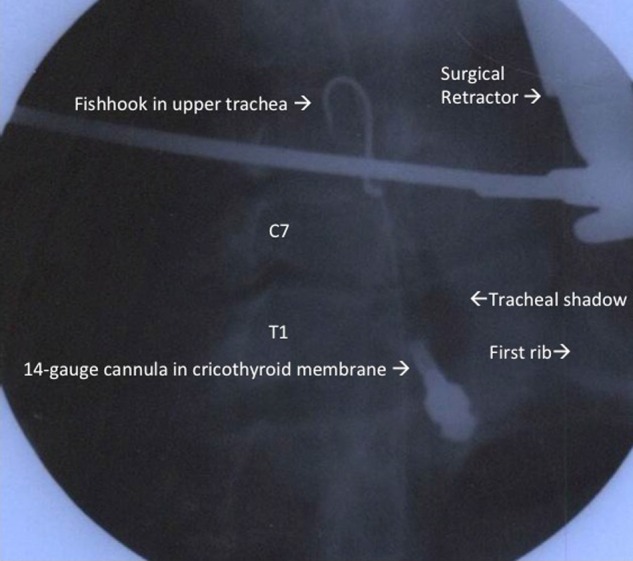
Image intensification of upper airway showing 14-gauge cannulae in the cricothyroid membrane (foreshortened view). The fishhook is visualised in the upper trachea. C7, seventh cervical vertebra; T1, first thoracic vertebra.
Figure 3.
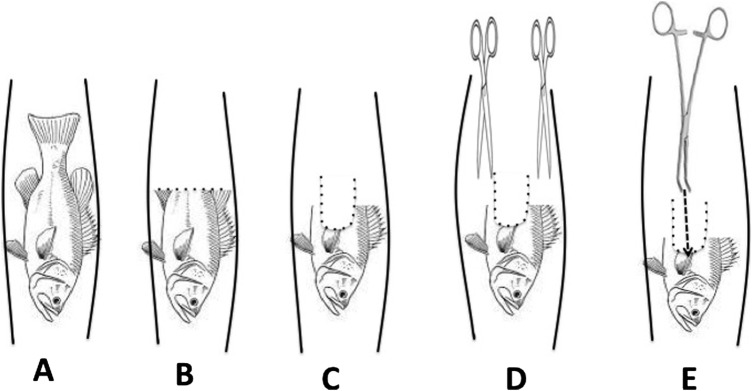
Diagram outlining removal of the fish from the hypopharynx. (A) The position of the fish in the upper airway with fins and spines impacting the fish into the mucosa of the hypopharynx. (B) The tail of the fish is then cut off. (C) A bone rongeur is used to core out the middle of the fish. (D) The spines of the fish are then cut using a small scissors freeing the fish from the mucosa of the hypopharynx. (E) Finally, the fish is grasped with an artery forceps and extracted from the airway.
Outcome and follow-up
The admission was complicated by aspiration pneumonia and sepsis requiring antibiotic therapy. Subsequent bronchoscopy excluded any endobronchial foreign matter, but the patient required ventilation for 5 days until the airway oedema resolved. He was then extubated and discharged home 3 days later. He made an uneventful recovery. The patient has given consent for this case report. He remains a keen and committed fisherman.
Discussion
Foreign body ingestion causing airway obstruction is a common clinical scenario. While fish bone is one of the most common foreign bodies ingested,1 2 airway obstruction from the accidental ingestion a whole fish is rare. Pinheiro et al3 reported the choking death of a healthy fisherman who put a live sole between his jaws to free up his hands so that he could collect more fish to put into his basket. The fish squirmed into the larynx and upper trachea; attempts by his colleagues to rescue the man using pliers did not succeed, and the man died. At postmortem examination, the fish's head was pointing down the fisherman’ throat, and the fins and spines were firmly attached to the tracheal mucosa, which explains why the fish was unable to be removed by bystanders. The authors stated that it was impossible to remove the fish by using external manoeuvres or instruments even during autopsy, and only sectioning of the trachea with scissors allowed the release of the fish. Three other deaths from airway obstruction due to swallowing a whole fish are also reported in the medical and forensic literature.4–6
As seen in this case report, the firm streamlined and aerodynamic attachments of the fish's external spines, fins and spines, while facilitating the fishes’ natural swimming movement in the anterograde direction, when attached to the oesophageal and tracheal mucosa, result in difficult retrograde extraction. This may be an important factor contributing to the fatal outcome of the previous reported cases of live fish ingestion. If the lodgement of the fish is in the larynx or trachea, then the likelihood of complete airway obstruction is high. In contrast, if the fish occupies only part of the pharynx or is lodged only in the oesophagus, breathing may still possible, and manual removal is less tedious.
In the case described here, the decision to perform emergency needle cricothyrotomy was paramount to a successful outcome. The delivery of oxygen via the cricothyrotomy cannulae prevented severe hypoxia from airway obstruction. Hypoxia from airway obstruction is recognised as a significant contributing factor in up to 34% of prehospital deaths.7 In this case, by the time the fisherman arrived at Kerang district hospital, his level of consciousness had deteriorated due to a combination of worsening hypoxia and hypercarbia. While 100% oxygen could be effectively delivered through both 14-Gauge cannulae, ventilation was significantly impaired. The resulting hypercarbia likely precipitated cerebral vasodilation, respiratory acidosis and a reduced level of consciousness. Although needle cricothyrotomy involving the insertion of large-bore cannulae though the cricothyroid membrane is a standard emergency technique employed as a temporising measure to correct hypoxia in acute upper airway obstruction, the blind insertion of a 4 mm microlaryngoscopy tube, as described in this report, is not a conventional emergency airway management technique. This could have impacted fish further into the airway during the intubation process worsening the obstruction or inducing laryngospasm. Conventional airway management techniques in this setting include performing a surgical cricothyrotomy, with the placement of a 6.0 mm or 6.5 mm cuffed tracheal tube railroaded over a bougie through the cricothyroid space and into the trachea, with or without the use of a tracheal hook, or using a commercially available percutaneous cricothyrotomy catheter kit, for example, Melker Kit (Cook Medical) to convert a cannula emergency airway into a definitive airway.
Our technical method for removing the fish is noteworthy (figure 3). A bone ronguer was used to core out the body of the fish, which allowed the fish to be grasped by artery forceps; this ‘collapsed’ the fish sufficiently to pass scissors down its sides, cutting the spines and scales and freeing the fish from the hypopharynx. The spines of the fish were then individually removed from the airway mucosal wall allowing the head of the fish to be completely extracted (figure 4).
Figure 4.
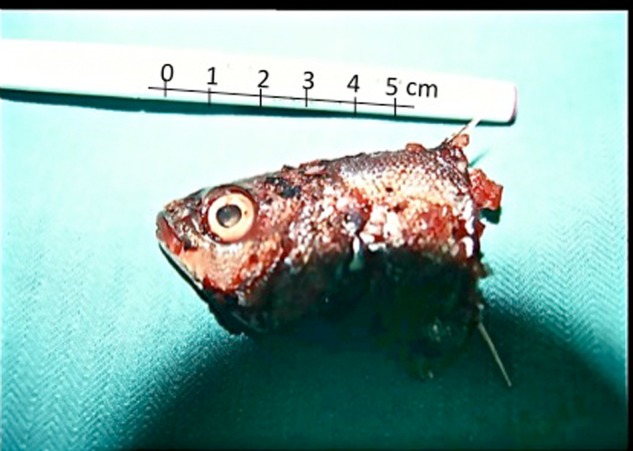
The head of the fish after removal. The scales and external fins were cut using a scissors, freeing the fish from the mucosa of the hypopharynx.
In conclusion, we report a rare case of survival after accidental ingestion of a whole live fish resulting in complete airway obstruction. The streamlined and aerodynamic attachments of the fish's external fins and spines to the mucosa of the hypopharynx prevented immediate removal, and made subsequent removal technically challenging. Successful extraction required cutting the fishes’ external fins and scales that were attached to the hypopharyngeal mucosa. In any clinical scenario where the upper airway is obstructed, the priorities are to prevent hypoxia and hypercarbia and to expediently secure the airway. If orotracheal intubation is not possible, alternative airway strategies should not be delayed and should follow a ‘cannot intubate, cannot ventilate algorithm’.8
Learning points.
Accidental ingestion of any foreign body is potentially fatal due to upper airway obstruction.
Signs of upper airway obstruction require immediate medical intervention.
Needle cricothyrotomy may be life-saving in extreme circumstances, but is a temporising measure until a definitive airway can be established.
A surgical cricothyrotomy may be indicated for immediate oxygenation during life-threatening airway obstruction.
Footnotes
Contributors: LW coauthored the manuscript, assisted with the literature review and was responsible for the submission of the manuscript. TT assisted with the literature review and the writing of the manuscript. JE was the leading critical care physician that managed this case. In addition he assisted with the writing of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Nandi P, Ong GB. Foreign body in the oesophagus: review of 2394 cases. Br J Surg 1978;2013:5–9 [DOI] [PubMed] [Google Scholar]
- 2.Ngan JH, Fok PJ, Lai EC, et al. A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg 1990;2013:459–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pinheiro J, Cordeiro C, Vieira DN. Choking death on a live fish (Dicologoglossa cuneata). Am J Forensic Med Pathol 2003;2013:177–8 [DOI] [PubMed] [Google Scholar]
- 4.Trevett AJ, Lalloo DG, Kevau IH. A piscatorial epistle. BMJ 1992;2013:1578–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pritchard JR. Sudden death by Lepomis macrochirus (the killer fish). Am J Forensic Med Pathol 1989;2013:245–6 [DOI] [PubMed] [Google Scholar]
- 6.Deidiker R. Return of the killer fish: accidental choking death on a bluegill (Lepomis macrochirus). Am J Forensic Med Pathol 2002;2013:197–8 [DOI] [PubMed] [Google Scholar]
- 7.Hussain LM, Redmond AD. Are pre-hospital deaths from accidental injury preventable? BMJ 1994;2013:1077–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heard AM, Green RJ, Eakins P. The formulation and introduction of a ‘can't intubate, can't ventilate’ algorithm into clinical practice. Anaesthesia 2009;2013:601–8 [DOI] [PubMed] [Google Scholar]


