Abstract
Primary cutaneous aspergillosis is a rare disease usually caused by Aspergillus fumigatus, Aspergillus flavus, Aspergillus terreus and Aspergillus ustus. It is usually seen in immunocompromised hosts, though some cases are also reported in immunocompetent hosts. We present a case of an immunocompetent farmer who presented with generalised nodules and plaques, mimicking erythema nodosum leprosum but turned out to be cutaneous aspergillosis caused by Aspergillus tamarii. The characteristic ascospores of Aspergillus species were found in skin lesions on fungus isolated in culture. The patient showed excellent response to antifungal therapy.
Background
Aspergillosis is usually seen in patients suffering from tuberculosis, malignancies, silicosis, diabetes or those on long-term corticosteroids, immunosuppression and antibiotics.1 2 The usual site of infections are lung, central nervous system and sinuses.3 4 Cutaneous aspergillosis is an uncommon opportunistic fungal infection that may occur either as a primary or a secondary infection.5 The most frequent causative organisms that cause cutaneous aspergillosis are Aspergillus fumigatus, Aspergillus flavus, Aspergillus terreus, Aspergillus niger and Aspergillus ustus.6–8 Primary cutaneous infection especially in immunocompetent patients is extremely rare but an increase in prevalence has been noted in the last 20 years.5 9 10 Primary cutaneous aspergillosis usually involves sites of skin injury or near intravenous access catheter sites at sites of traumatic inoculation or occlusive dressing due to surgery. Secondary cutaneous lesions result either from contiguous extension to the skin from an infected underlying structure or from widespread blood borne seeding of the skin.1 3
We present a case of a primary cutaneous aspergillosis caused by A tamarii in an immunocompetent farmer with erythematous nodular and plaque-like lesions mimicking erythema nodosum leprosum.8 9
Case presentation
A 65-year-old man, a farmer with no previous comorbities, presented with a high-grade fever, throat pain and loose stools 4–5 times with no mucous or blood, all of 3 days duration. He had a history of trauma to the right foot 1 month ago. On examination, the patient was febrile with a heart rate of 96 bpm and blood pressure of 130/80 mm Hg. The posterior pharyngeal wall was congested with white exudates that did not bleed on touch. Multiple tender erythematous nodules and plaques were present on extremities, back, trunk and forehead (figures 1 and 2). A partially healed traumatic wound was present on the right foot. There was no thickened nerve, hypopigmented or hypoanaesthetic patch. Systemic examination was unremarkable. A provisional clinical diagnosis of viral enteritis with secondary streptococcal pharyngitis with erythema nodosum was kept and treated with supportive therapy and antibiotics. Dermatologist gave the clinical diagnosis of erythema nodosum leprosum for the skin lesion.
Figure 1.
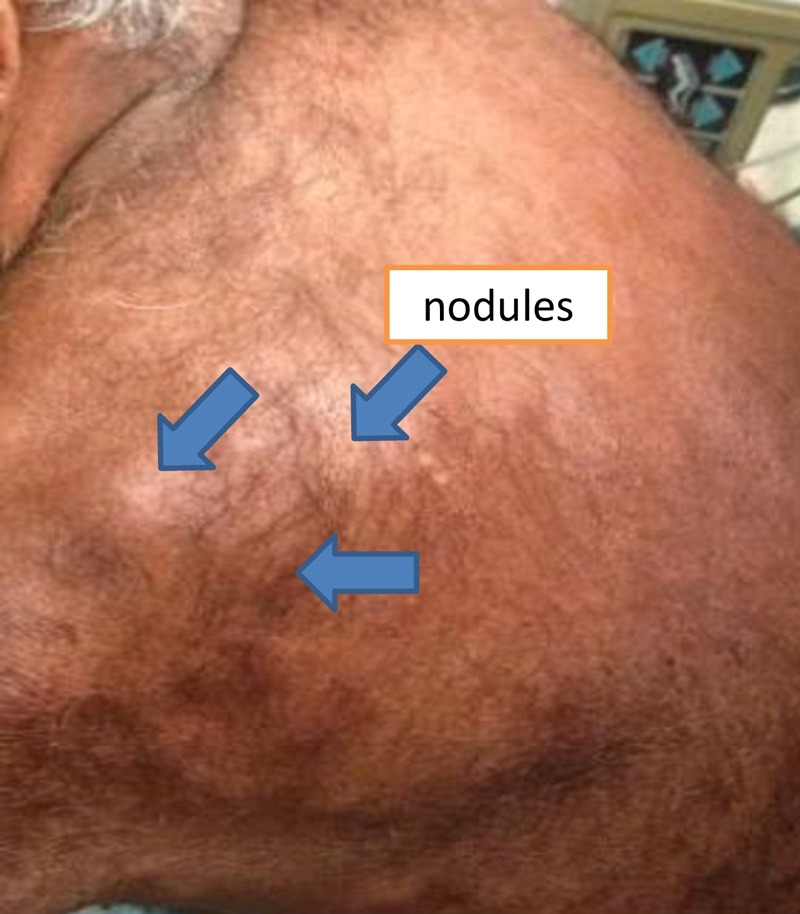
Nodular skin lesions.
Figure 2.
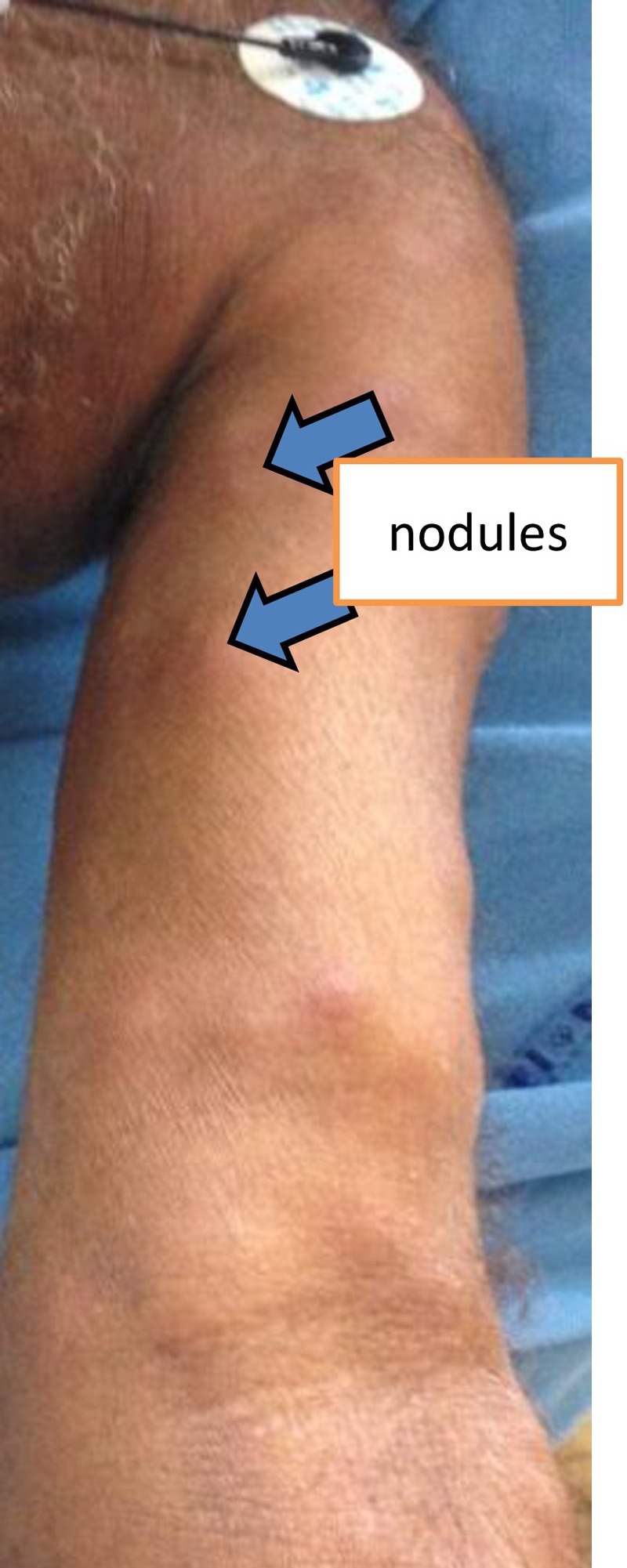
Nodular skin lesions.
Investigations
Throat swab showed Gram-positive cocci in pairs, tetrads and oval budding yeast cells with pseudohyphae. Zeihl-Neelsen staining was negative for acid-fast bacilli. Slit skin smear from seven sites were negative for acid-fast bacilli. Wedge biopsy from the nodular lesions from two different sites showed normal intact pigmented keratinised squamous epidermis with periadnexal-mixed inflammation, abscess cavity involving deep dermis and subcutis. Plenty of fungal elements branching at acute angles some septate were identified in the abscess (figure 3). A modified Fite-Faracco stain was negative for acid-fast bacilli. KOH mount and Gram stain showed branched septate fungal hyphae (figure 4A,B).Sabouraud's dextrose agar culture showed brownish powdery colonies on macroscopy while microscopy showed septate dichotomous branching hyphae with conidiophores terminating in vesicle. The fungus isolated was finally identified as Aspergillus species. The strain was sent to National Reference Laboratory at PGIMER, Chandigarh, India and it was identified as A tamarii both phenotypically and genotypically.
Figure 3.
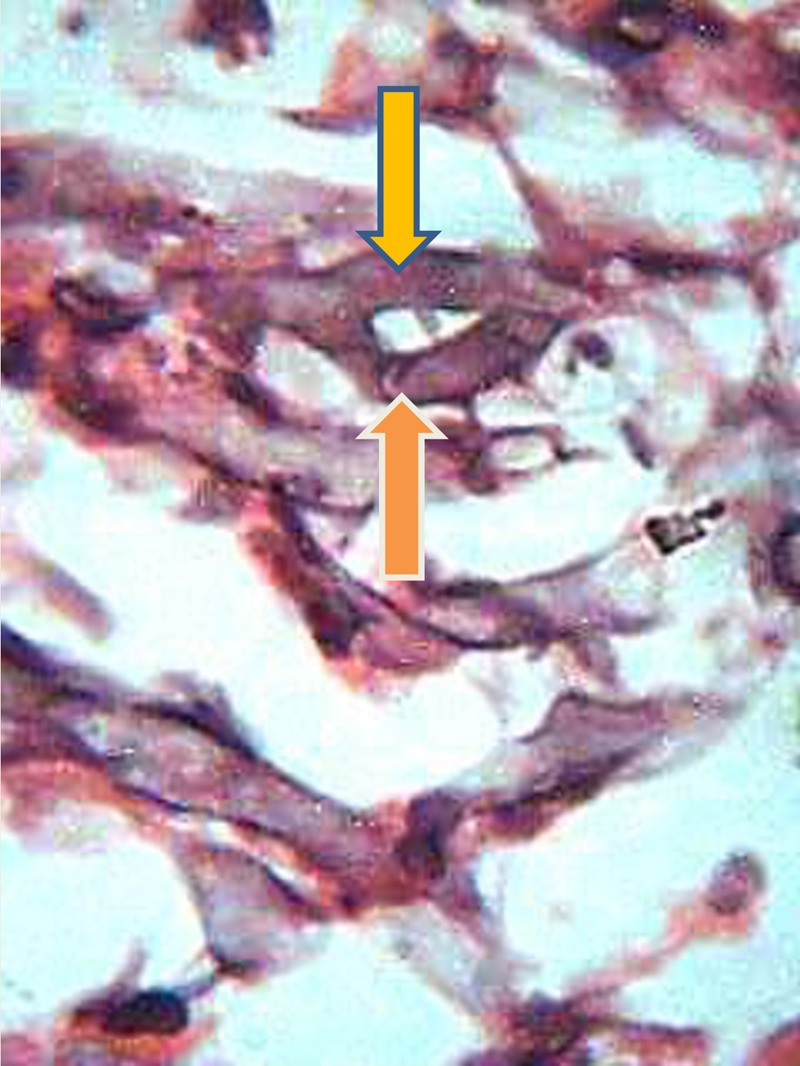
Abscess cavity with septate fungal hyphae (H&E stain ×1000).
Figure 4.
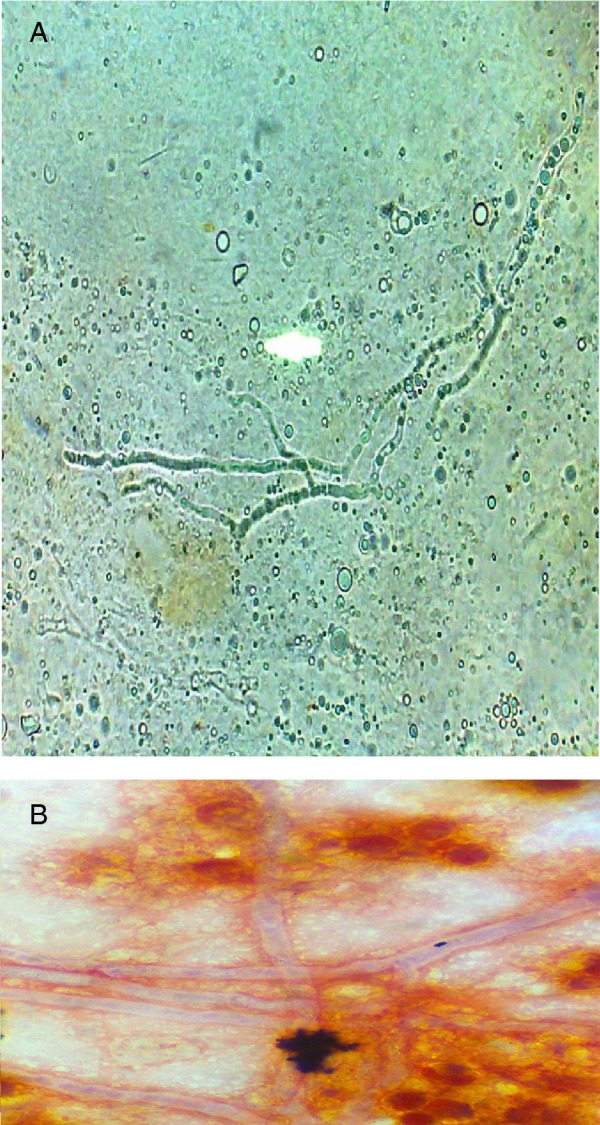
(A and B) KOH mount and Gram stain showing branched septate fungal hyphae.
Treatment
Our patient presented with multiple erythematous nodules and plaques out of which the two nodules ulcerated after biopsy. Our patient being a farmer working bare foot in fields acquired this from the soil following a trauma to the right leg.9 11 12 The widespread distribution and morphology of the lesion misled the dermatologist for erythema nodosum leprosum but mycological and histological examination confirmed the diagnosis. Although complete healing of cutaneous aspergillosis after oral antifungals is rare, our patient recovered completely after first line treatment with itraconazole.10 13 Itraconazole was given as 200 mg orally twice daily for 4 weeks.
Outcome and follow-up
The patient is asymptomatic with no skin lesions during 1-year follow-up (figure 5).
Figure 5.

Healed lesions post-treatment.
Discussion
Primary cutaneous aspergillosis though reported quite often in recent years in immunosupressed patients still poses a diagnostic challenge in immunocompetent patients.1 5 Healthy hosts can develop cutaneous aspergillosis in surgical wounds, traumatic inoculation or by exposure to high spore counts in occupations such as farming.1 11
Although over 300 species of aspergillosis exist, over 90% of human infection is by A fumigatus, A flavus, A niger, A ustus. This fungus is commonly found in decaying vegetation, stored grains and soil.1 9–11
Primary cutaneous aspergillosis may present as erythematous indurated macules, papules, plaques or haemorrhagic bullae, which may progress to necrotic ulcers that are covered by black eschar, nodular and pustular lesions or subcutaneous abscesses.9 10
Learning points.
Cutaneous aspergillosis in immunocompetent hosts is rare; however, one may come across such cases in individuals with skin exposure to soil.
Lesions can be widespread and generalised.
Morphology and distribution of lesions are not enough for making a diagnosis.
Lesions can be clinically mistaken for erythema nodosum leprosum.
Footnotes
Contributors: SS was involved in the management of the case and in the write-up of the manuscript, coordinated with the reference laboratory at PGIMER, Chandigarh, India, regarding phenotyping and genotyping of the specimen. BMY contributed in preparation and interpretation of slides and write-up of the microbiology specimen. SKN had a role in bibliography preparation. PP was involved in preparation, interpretation of Fite-Faraco stain of skin biopsy specimen, interpretation and write-up of the same.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.van Burik JA, Colven R, Spach DH. Cutaneous aspergillosis. J Clin Microbiol 1998;2013:3115–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chakrabarti A, Gupta V, Biswas G, et al. Primary cutaneous aspergillosis: our experience in10 years. J Infect 1998;2013:24–7 [DOI] [PubMed] [Google Scholar]
- 3.Khatri ML, Stefenato CM, Benghazeil M, et al. Cutaneous and paranasal aspergillosis in an immunocompetent patient. Int J Dermatol 2000;2013:853–6 [DOI] [PubMed] [Google Scholar]
- 4.Domergue V, Orlandini V, Begueret H, et al. Cutaneous, pulmonary and bone aspergillosis in a patient presumed immunocompetent presenting subacute cutaneous lupus erythematosus. Ann Dermatol Venereol. 2008;2013:217–21 [DOI] [PubMed] [Google Scholar]
- 5.Mohapatra S, Xess I, Swetha JV, et al. Primary cutaneous aspergillosis due to Aspergillus niger in an immunocompetent patient. Indian J Med Microbiol 2009;2013:367–70 [DOI] [PubMed] [Google Scholar]
- 6.Ozer B, Kalaci A, Duran N, et al. Cutaneous infection caused by aspergillus terreus: case report. J Med Microbiol 2009;2013:968–70 [DOI] [PubMed] [Google Scholar]
- 7.Ricci RM, Evans JS, Meffert JJ, et al. Primary cutaneous Aspergillus ustus infection: second reported case. J Am Acad Dermatol 1998;2013:797–8 [DOI] [PubMed] [Google Scholar]
- 8.Andresen J, Nygaard EA, Størdal K. Primary cutaneous aspergillosis—a case report. Acta Paediatr 2005;2013:761–2 [DOI] [PubMed] [Google Scholar]
- 9.Tahir C, Garbati M, Nggada HA, et al. Primary cutaneous aspergillosis in an immunocompetent patient. J Surg Tech Case Rep 2011;2013:94–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang QQ, Li L, Zhu M, et al. Primary cutaneous aspergillosis due to aspergillus flavus: a case report. Chin Med J (Engl) 2005;2013:255–7 [PubMed] [Google Scholar]
- 11.Camus M, Anyfantakis V, Dammak A, et al. [Primary cutaneous aspergillosis in an immunocompetent farm worker]. Ann Dermatol Venereol 2010;2013:373–6 [DOI] [PubMed] [Google Scholar]
- 12.Romano C, Miracco C. Primary cutaneous aspergillosis in an immunocompetent patient. Mycoses 2003;2013:56–9 [DOI] [PubMed] [Google Scholar]
- 13.Ajith C, Dogra S, Radotra BD, et al. Primary cutaneous aspergillosis in an immunocompetent individual. J Eur Acad Dermatol Venereol 2006;2013:738–9 [DOI] [PubMed] [Google Scholar]


