Abstract
A woman in her early 60s presented to our Movement Disorders Centre with a 5-year history of progressive peripheral neuropathy, gait instability with falls, blurred vision, cognitive impairment and tremors. The patient was found to have profound sensory ataxia, chronic ophthalmoplegia, dementia with significant deficits in registration and construction and bilateral resting tremor of the hands. Investigations revealed an unremarkable MRI of the brain, negative cerebrospinal fluid studies, and unremarkable chemistries. Nerve conduction studies found a severe sensorimotor axonal polyneuropathy. Genetic testing revealed a compound heterozygous mutation in the POLG1 gene consistent with the diagnosis of Sensory Ataxia Neuropathy Dysarthria and Ophthalmoplegia (SANDO) syndrome.
Background
Sensory Ataxia Neuropathy Dysarthria and Ophthalmoplegia (SANDO) syndrome is a rare mitochondrial inherited disorder that can present early to late in life1 and can be associated with multiorgan dysfunction2 requiring a collaborative effort among multiple specialties to effectively manage an affected patient. This particular case is of importance as it highlights difficulties in diagnosing the syndrome, which in our patient was originally due to diabetic peripheral neuropathy or Parkinson's disease with autonomic dysfunction.
Case presentation
A woman in her early 60s with medical history significant for diabetes mellitus 2, congestive heart failure, hypothyroidism, hypertension, depression with psychotic features and gastric bypass surgery presented to the Movements Disorders Clinic as a referral from a local neurologist for evaluation of several chronic neurological problems including gait difficulties, cognitive impairment, ophthalmoplegia, resting tremor and peripheral neuropathy. Her family history was unremarkable for known neurological problems. Five years prior to this presentation the patient had experienced shooting pains and numbness in her lower extremities. As time progressed the pain and sensation loss began to involve her upper extremities. Given her history of diabetes she was diagnosed with diabetic neuropathy and was treated symptomatically with topiramate and gabapentin. Approximately 1 year after this diagnosis she developed occasional rectal incontinence. Her primary care physician deemed this to also be the result of the autonomic dysfunction seen with diabetic neuropathy. At this time she also started stumbling and having trouble walking up and down stairs. The following year the patient underwent a gastric bypass surgery and successfully lost over 100 pounds but did not see improvement in her walking. She felt her 17-year history of chronic depression had worsened despite selective serotonin reuptake inhibitors therapy. At this time she was placed on valproic acid for psychotic features associated with her depression described as visual hallucinations. These mostly consisted of seeing items race across the floor or hearing music playing. Occasionally, she reported seeing her husband in doorways when she knew him not to be in the house. Over time she began to report more falls and presyncopal dizziness. This presyncope once progressed to a total loss of consciousness which resulted in a motor vehicle accident without significant injury. She reported worsening vision over the next couple of years but was known to have complicated diabetic retinopathy and had undergone several laser procedures in the past. Approximately 5 years after the onset of symptoms she was referred to a local neurologist. During his examination he observed sensory ataxia secondary to a sensorimotor polyneuropathy, chronic supranuclear ophthalmoplegia, and a resting tremor of her right hand. This neurologist was concerned that her presentation represented Parkinson's disease with autonomic dysfunction and referred her to our centre.
On initial presentation to our Movement Disorders Centre the patient's general examination was unremarkable. Neurological examination revealed a supranuclear ophthamoplegia with restricted eye movements only recoverable with the doll's eyes maneuver. She displayed bilateral ptosis and marked temporal muscle wasting. The rest of her cranial nerve examination was without deficit. Her sensory examination found loss of pinprick sensation, temperature and vibration bilaterally up to her hips. She had bilateral vibration loss at her fingertips. She had loss of proprioception at her toes. Her gait was very wide based and swaying. She had bilateral dysdiadochokinesia with significant ataxia on finger to nose testing. She had a bilateral resting tremor in her hands but no action or intention tremor. On neuromuscular exam the patient was found to be arreflexic in her lower extremities with preserved reflexes in her upper extremities. On strength testing she was found to be weaker in her left arm (4/5) as compared to her right. Her hip flexors were weakest at 3+ bilaterally. Strength testing was normal in all other muscle groups. On cognitive testing she was found to have moderate dementia with significant deficits in registration and construction as well as ideomotor apraxia. Her speech was intact without signs of dysarthria.
Investigations
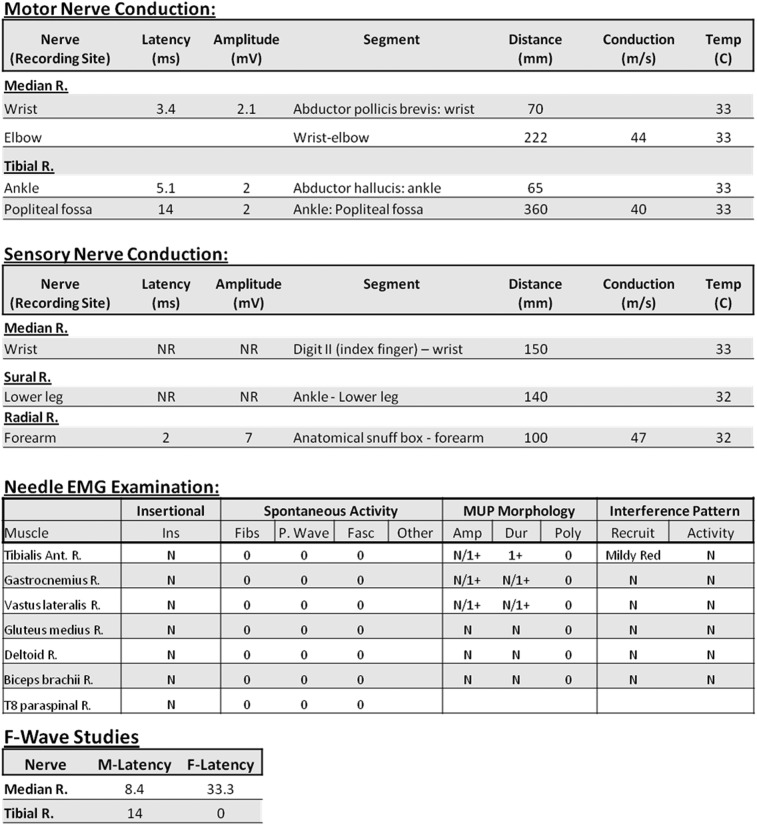
Prior to presentation at our Movement Disorders Clinic the patient had undergone an MRI of the brain without contrast. This showed mild scattered periventricular white matter disease. The scan did not reveal any pontine or cerebellar atrophy or significant mass lesion. She had undergone an electromyography (EMG) and nerve conduction studies (NCS) after her initial presentation to her referring neurologist that showed a severe sensorimotor axonal polyneuropathy in her legs, bilateral carpal tunnel disease and an absent right ulnar sensory potential. Serum studies had revealed a normal complete blood count and comprehensive metabolic panel, borderline elevation in thyroid stimulating hormone , normal B12 and folate levels, a normal serum protein electrophoresis SPEP and negative antinuclear antibody ANA. Serum antibody testing was negative for anti-Hu or anti-Yo.
After presentation to our clinic the patient underwent a lumbar puncture under fluoroscopy. Her cerebrospinal fluid (CSF) results revealed normal cell counts, protein and glucose levels. CSF lactate and pyruvate levels were not evaluated. CSF testing for oligoclonal bands and a full paraneoplastic antibody panel were negative. Serum testing for vitamin E and B1 levels was normal. Protein electrophoresis and cryoglobulin testing were also normal. Given the patient's ptosis and myopathy on examination the patient underwent another EMG/NCS 2 years after her initial neuromuscular study. This found severe length dependent sensorimotor axonal polyneuropathy (figure 1). She also had acetylcholine receptor antibody testing that was negative. Finally, 6 years after initial symptom onset the patient underwent genetic testing that confirmed a diagnosis of SANDO syndrome.
Figure 1.
Nerve conduction studies and electromyography.
Differential diagnosis
Prior to her evaluation by a neurologist, the patient's symptoms were attributed to diabetic peripheral polyneuropathy. This initial diagnosis was not unreasonable. The patient had suffered from diabetes for several years and peripheral neuropathy is a well known complication of diabetes. Her gait ataxia, orthostatic syncope and rectal incontinence were attributed to proprioceptive and autonomic dysfunction secondary to this neuropathy.3 Her symptoms fit well with this diagnosis until further neurological deficits such as opthalmoplegia and tremors began to appear. This led to the patient's referral to our clinic out of concern for Parkinson's disease with autonomic dysfunction.
Once evaluated in our clinic, it was felt the patient was unlikely to have idiopathic Parkinson's disease given her rate of progression, the prominence of her sensory ataxia, her ophthalmoplegia and the symmetric nature of her rest tremor. We considered parkinsonisms such as progressive supranuclear palsy (PSP) and multiple systems atrophy of cerebellar type (MSA-C). Though PSP would account for her ophthalmoplegia and falls, the presence of tremor, ataxia and neuropathy were atypical, as was the lack of gait freezing.4 MSA-C can present with autonomic signs such as urinary dysfunction and prior to the development of motor signs.5 Our patient had mild bilateral resting tremor noted on examination and significant gait ataxia, both consistent with MSA-C. Arguing against this disease entity were her ophthalmoplegia, neuropathy, hallucinations and dementia.6 Her relatively normal brain MRI revealed no atrophy of her putamen, middle cerebellar peduncle or pons, which also argued against this disease.7 Given the lack of supporting evidence for these parkinsonisms the patient's differential diagnosis was broadened to include other pathologies with significant ataxia such as a spinocerebellar ataxia (SCA).
There are several different subtypes of SCA based on different genetic mutations in the gene encoding fibroblast growth factor 14 and all of the SCAs have a wide phenotypical variation. Common to the SCAs are oculomotor disorders, ataxic gait and dysarthria and/or dysmetria. They usually are chronic and progressive in their course.8 The patient’s initial opthalamoplegia, ataxia, cognitive dysfunction and tremor on examination were especially concerning for SCA type 1, 2 or 3. SCA however did not completely fit the patient’s disease picture in that the MRI of her brain was grossly unremarkable. SCA patients’ imaging would be expected to reveal cerebellar, olivopontocerebellar or global cerebral atrophy. In addition, SCA 1–3 are autosomal dominant.9 Our patient had no family history for any SCA-like symptoms. The SCAs do have a broad phenotypic presentation and a spontaneous mutation in a patient was also considered. However, the diagnosis of SCA was made less likely by the patient’s progressive myopathy and bilateral ptosis. In fact, the patient’s ptosis had become such a problem that she had undergone a blepharoplasty for visual obstruction. Myopathy is not associated with these diseases, although other signs and symptoms can be seen in SCAs such as extrapyramidal symptoms, pyramidal symptoms and seizures.8 This finding led us to broaden the differential further to include phenotypically similar disorders that may also present with myopathy. This led us to consider mitochondrial disease.
The mitochondrial disorders are also an inherited group of diseases. Unlike the SCAs they are usually autosomal recessive in their inheritance or due to sporadic mutations. Phenotypically they present with a broad range of symptoms and many have been classified based on their specific symptoms into syndromes. Based on the patient's presentation with sensory ataxia, dysarthria, dysphagia and ophthalmoplegia it was decided that she best fit into the mitochondrial disorder of SANDO syndrome. In addition to the acronym-derived symptoms of the disorder patients are often reported to have peripheral neuropathy, cognitive dysfunction, tremor, and multiorgan manifestations of the disease including diabetes, thyroid disorders, and liver dysfunction.10
Treatment
Treatment of mitochondrial disorders is largely supportive in nature: physical and occupational therapy for weakness and gait stability training and speech therapy for monitoring of swallowing dysfunction in patients with bulbar symptoms. Some patients have undergone blepharoplasty for palliative treatment of severe bilateral ptosis. The patients with seizures require close management with anticonvulsive drugs. Valproic acid is considered contraindicated as its metabolism interferes with oxidative phosphorylation and in these patients may lead to fulminant liver failure.11
Outcome and follow-up
Genetic testing revealed three pathogenic mutations in the POLG1 gene. One allele was found to have two sequence variants: c.[752C>T; 1760C>T]. Both of these variants coded for amino acid substitutions [THR>ILE;PRO>LEU]. The other allele displayed a compound heterozygous mutation of c.1399G>A, which resulted in coding for threonine rather than alanine. All of these mutations were felt to be autosomal recessive in inheritance, and have been reported in other cases involving mitochondrial disorders. Given her genetic mutations and clinical presentation it was felt her diagnosis was most consistent with SANDO syndrome.
The patient's case was discussed with her primary care physician with recommendation to stop the patient's valproic acid given the potential of provoking liver disease in this patient population. She continues to follow-up in the Movement Disorders Clinic for continued monitoring of her disease progression and supportive care.
Discussion
SANDO syndrome is characterised by a triad of sensory or cerebellar ataxia, dysarthria and opthalmoparesis. The patients often present with a peripheral neuropathy which contributes to the ataxia experienced. It can present anywhere from early adulthood to late in life. The first cases of SANDO were reported in 1997 by Fadic et al.1 Since that time relatively few cases have been reported as this disorder appears to be strikingly rare. The prevalence of this disease in the general population is unknown, however, the prevalence in the general population reported for all mitochondrial disorders is 9/100 000.
The pathophysiology of SANDO most often results from mutations in the POLG1 gene. POLG1 usually encodes for DNA polymerase-γ which is important in mitochondrial DNA (mtDNA) replication. There are now over 150 POLG1 mutations known and collectively these mutations result in errors in mtDNA. These errors accumulate and cause dysfunction in the respiratory chain of the oxidative-phosphorlation pathway leading to clinical symptoms and findings. SANDO can be either autosomal recessive or sporadic in inheritance. Rarely, the disorder has been reported as autosomal dominant in inheritance resulting from a twinkle-helicase mutation.12
Classically the disorder presents with the aforementioned triad of sensory or cerebellar ataxia, dysarthria and opthalmoparesis. However there is a wide phenotypical variation among patients. The patients with the disease can present with dysphagia, cognitive impairment, peripheral neuropathy, myopathy, seizure, encephalopathy, hepatopathy, psychiatric disorders, headaches and ptosis.10 As is typical for mitochondrial syndromes, patients may be severely affected by progressive neurological deficits or may have relatively mild and stable symptoms. This wide variation in patient presentation often makes diagnosis difficult, as was the case in our patient. Once a mitochondrial disorder is suspected making the diagnosis between the different mitochondrial syndromes can be difficult as there is often significant symptom overlap.11 Though genetic testing assists with the diagnosis, a given gene mutation can give rise to multiple syndromes. POLG1 mutations are not specific for SANDO alone and can be seen in progressive external PEO, myoclonic epilepsy myopathy and sensory ataxia, childhood myocerebrohepatopathy syndrome, Alpers-Huttenlocher syndrome and ataxia neuropathy spectrum. Therefore it is imperative to have thorough clinical and genetic evaluations prior to arriving at the proper diagnosis.
Diagnosis of SANDO is not made on examination alone. Support for the diagnosis comes from histological, electrophysiological and genetic testing. Sural nerve biopsy can also be helpful. This often reveals a loss of small and large myelinated fibres as well as possible onion bulb formations.12 Nerve conduction testing is likely to reveal a sensory peripheral neuropathy as sensory disturbances predominate in the disease. However, this testing can also show motor or mixed neuropathic findings. Ultimately the diagnosis is best made with genetic testing coupled with typical clinical findings. If a POLG1 mutation is confirmed by genetic testing in a patient with symptoms consistent with the disease it is highly advisable for family members to undergo genetic testing and counselling as well.11
Learning points.
Sensory Ataxia Neuropathy Dysarthria and Ophthalmoplegia (SANDO) syndrome is defined by a triad of sensory or cerebellar ataxia, dysarthria and opthalmoparesis but can include many other neurological deficits and symptoms.
SANDO syndrome is due to a mutation in the POLG1 gene for mitochondrial DNA polymerase.
Consider mitochondrial disorders in patients presenting with peripheral neuropathy and other neurological complaints.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Weiss M, Saneto R. Sensory ataxia neuropathy with dysathria and ophthalmoparesis (SANDO) in late life due to compound heterozygous POLG mutations. Muscle Nerve 2010;2013:882–5 [DOI] [PubMed] [Google Scholar]
- 2.Finsterer J. Inherited mitochondrial neuropathies. J Neurol Sci 2011;2013:9–16 [DOI] [PubMed] [Google Scholar]
- 3.Smith A, Singleton R. Diabetic neuropathy. Continuum Lifelong Learn Neurol 2012;2013:60–84 [DOI] [PubMed] [Google Scholar]
- 4.Litvan I, Agid Y, Calne D, et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): report of the NINDS-SPSP international workshop. Neurology 1996;2013:1–9 [DOI] [PubMed] [Google Scholar]
- 5.Jecmenica-Lukic M, Poewe W, Tolosa E, et al. Premotor signs and symptoms of multiple system atrophy. Lancet Neurol 2012;2013:361–8 [DOI] [PubMed] [Google Scholar]
- 6.Gilman S, Low PA, Quinn N, et al. Consensus statement on the diagnosis of multiple system atrophy. J Neurol Sci 1999;2013:94–8 [DOI] [PubMed] [Google Scholar]
- 7.Gilman S, Wenning G, Low P, et al. Second consensus statement on the diagnosis of multiple system atrophy. Neurology 2008;2013:670–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manto M. The wide spectrum of spinocerebellar ataxias (SCAs). Cerebellum 2005;2013:2–6 [DOI] [PubMed] [Google Scholar]
- 9.Paulson H. The spinocerebellar ataxias. J Neuroophthalmol 2009;2013:227–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hudson G, Chinnery P. Mitochondrial DNA polymerase-γ and human disease. Hum Mol Genet 2006;2013:244–52 [DOI] [PubMed] [Google Scholar]
- 11.Cohen B, Naviaux R. The clinical diagnosis of POLG disease and other mitochondrial DNA depletion disorders. Methods 2010;2013:364–73 [DOI] [PubMed] [Google Scholar]
- 12.Finsterer J. Mitochondrial ataxias. Can J Neurol Sci 2009;2013:543–53 [DOI] [PubMed] [Google Scholar]