Abstract
A 12-year-old girl presented with a sudden onset of per rectal bleeding. After admission, she had further episodes of large volume per rectal bleeding and developed hypotensive shock. Hence a massive haemorrhage protocol was activated. Surgical, paediatric and anaesthetic support was sought immediately. Further resuscitation with packed red cells, platelets and fresh frozen plasma was successful. An urgent CT angiogram of the abdomen confirmed active arterial bleeding from an arteriovenous malformation in the caecum. After a detailed discussion between the surgeons and the interventional radiologists, it was decided to attempt therapeutic embolisation first, failing which surgery was the option. The patient and family were fully informed. Through a right femoral approach under local anaesthesia, the superior mesenteric artery was catheterised and the bleeding vessel was successfully controlled with two microembolisation coils. Except for some initial abdominal discomfort, she made an uneventful recovery and was discharged home.
Background
Though massive per rectal bleeding is a well-established entity in the adult population, it is rare in the paediatric age group and hence not adequately researched. This poses diagnostic dilemmas and therapeutic uncertainties.
Our case highlights that with a multidisciplinary approach and good communication, even such rare life-threatening conditions could be managed successfully in a district general hospital. Importantly, even in a paediatric age group, interventional radiology if available could be safely utilised to manage gastrointestinal bleeding, avoiding the need for a laparotomy.
We believe that the readers will find this very interesting and useful as massive per rectal bleeding is a common surgical presentation in an acute setting, but has presented in an unusual age group in our case and has been successfully dealt with in an unconventional way.
Case presentation
A very co-operative 12-year-old girl was brought in by ambulance to our district general hospital accident and emergency resus department following two large volumes of per rectal bleeding. She was accompanied by her mother. The rectal bleeding was dark red in colour and thought to be more than a litre in total. There was no recent history of diarrhoea or rectal mucous discharge. She felt dizzy and unwell, but denied abdominal pain.
There was no previous history of per rectal bleeding, melaena, recurrent abdominal pain or trauma. She was premenarchal. Her appetite has been good, and has not lost weight. She denied taking any medications recently. Her medical history included constipation and mild asthma, needing occasional salbutamol inhaler. Her development was appropriate for her age and was up to date in her immunisations. There was no relevant social or family history of note.
Clinically she was anxious but alert and oriented. Her skin and conjunctiva were pale. There was no evidence of circumoral pigmentation, telangiectases or purpuric lesions in the skin. She had a thready pulse and her observation showed a blood pressure of 96/61 mm Hg, heart rate of 130 bpm and a respiratory rate of 21/min. Abdominal examination was unremarkable. Her haemoglobin was 8.4 g/dL with a low haematocrit of 25% and a normal mean corpuscular volume of 83 fL after initial fluid resuscitation. Her coagulation profile, renal and liver function and electrolytes were normal. The surgeons were involved.
Though she responded well to our initial resuscitation with intravenous fluids and intravenous tranexamic acid, she had further episodes of large, dark red per rectal bleeding and developed frank hypotensive shock with a systolic blood pressure of 54 and a heart rate of 145 bpm. Hence a massive haemorrhage protocol was activated. Paediatric and anaesthetic support was sought immediately. She was resuscitated with further intravenous fluids, two units of packed red cells, one unit of platelets and one unit of fresh frozen plasma with good response.
Investigations
Though an upper gastrointestinal (GI) endoscopy would have been indicated as a ‘protocol’ in an adult with a similar clinical presentation, it was considered unnecessary in our patient as the differentials at this stage were bleeding from a colonic lesion or from a Meckel's diverticulum and not upper GI bleeding. Owing to the uncertainty of the site of bleeding, that is, small or large bowel, a colonoscopy was felt to be inappropriate. Moreover with massive per rectal bleeding, the views at colonoscopy may be suboptimal for a meaningful visualisation of the colon to aid diagnosis and treatment. Hence after a discussion with the radiologist, the patient underwent an urgent three-phase CT angiogram of the abdomen to identify the source of bleeding. This confirmed active arterial bleeding from an arteriovenous malformation (AVM) in the caecum (figures 1 and 2).
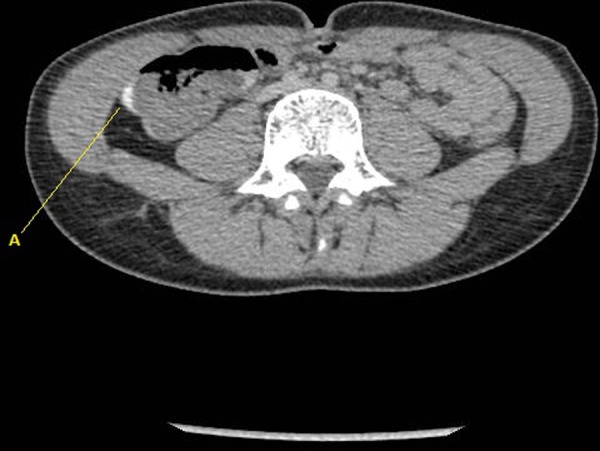
Figure 1.

Axial image of the arterial phase (25 s postinjection of contrast) of three-phase CT angiogram showing arterial blush and active extravasation of contrast in the caecal region (A).
Figure 2.
Delayed phase (5 min postinjection of contrast) of three-phase CT angiogram showing contrast layering in the caecum (A) indicating active bleeding.
Differential diagnosis
As the only positive finding was a large volume, painless and dark red per rectal bleeding, the differentials considered were bleeding from intestinal polyps, AVM of the bowel or from a Meckel's diverticulum.
Though infective colitis, inflammatory bowel disorder, peptic ulcer disease, bleeding diathesis, haemolytic uraemic syndrome, vasculitis (Henoch-Schonlein purpura), etc can also cause massive per rectal bleeding in this age group, there was no corroborative evidence in the patient's history, clinical examination or blood investigations to support any of them.
Treatment
Once the diagnosis of AVM of the caecum was made on the CT scan, the real debate was whether to attempt embolisation of the bleeding vessel or to proceed with an urgent laparotomy in our hospital. Transferring the patient to a tertiary unit was considered too. After a detailed discussion between the surgeons, interventional radiologists and the anaesthetist, it was decided to attempt therapeutic embolisation of the bleeding vessel in the interventional radiology suite.
After full discussion with the patient and her mother, a second interventionist was requested to attend. The emergency theatre was alerted as surgery was the back-up plan if embolisation failed or a complication occurred during the interventional radiology procedure.
Under local anaesthesia, through the right femoral approach, using a 4 French sheath in the groin, the superior mesenteric artery was catheterised and active bleeding in the caecum confirmed (figures 3 and 4). Two micro-embolisation coils were successfully placed in the feeding vessel to achieve complete control (figure 5).
Figure 3.
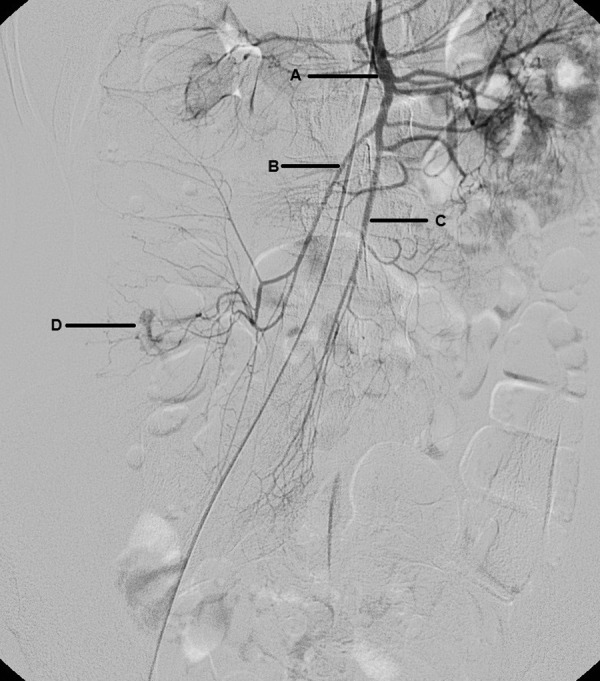
Superior mesenteric artery angiogram delineating the anatomy (A, superior mesenteric artery; B, right colic artery; C, ileocolic artery; D, contrast extravasation in the caecal region).
Figure 4.
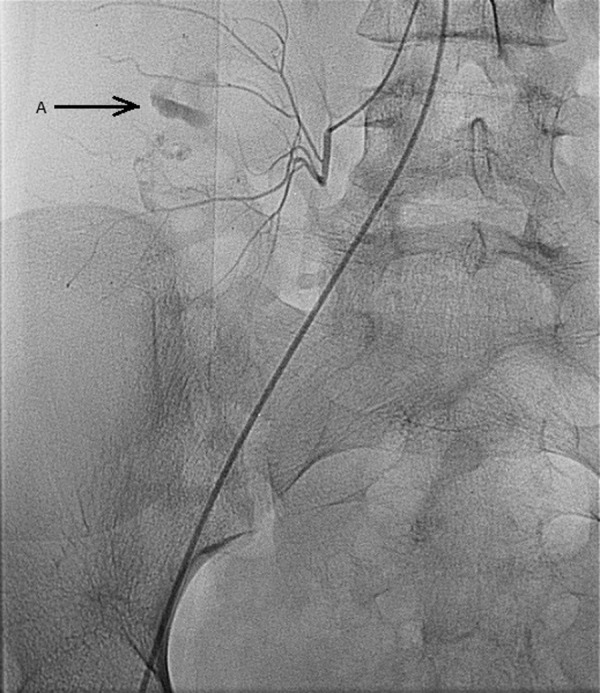
Super selective superior mesenteric artery angiogram using microcatheter demonstrating bleeding in the caecum (A).
Figure 5.
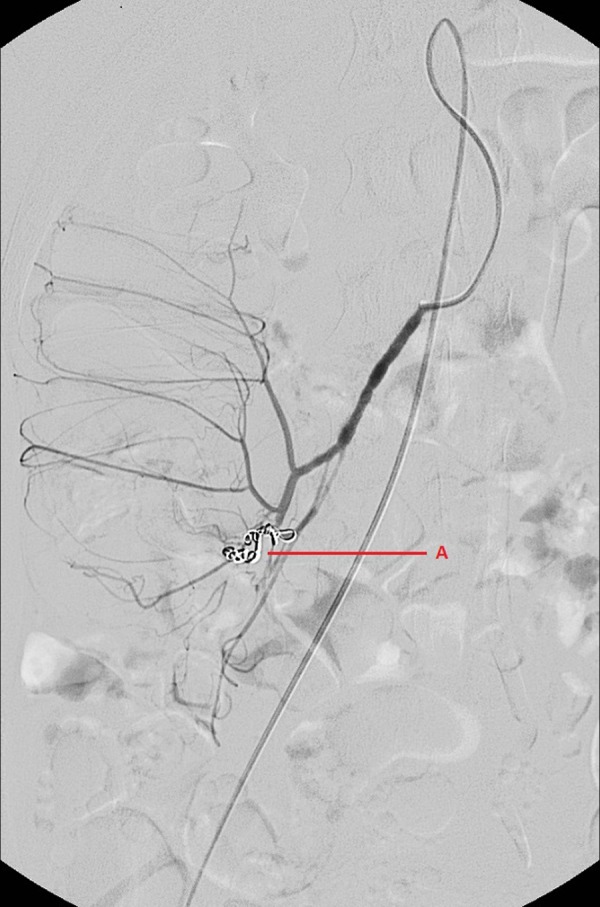
Digital subtraction angiography showing two microembolisation coils (A) deployed within the feeding artery to stop the bleeding.
Outcome and follow-up
Postprocedure, she was admitted to the paediatric ward for close observation. Though there was no further per rectal bleeding, a further 6 units of packed red cells was transfused during the first postprocedure day to replace the blood loss. As per massive blood transfusion protocol and as advised by the haematologist, a unit each of platelets and fresh frozen plasma were transfused during the first postprocedure day. Except for some minor right iliac fossa discomfort in the first 24 h postprocedure, she made an uneventful recovery under the joint care of the surgeons and paediatricians and was discharged home on day 5, with a haemoglobin of 14.5 g/dL. The postprocedure stay in the hospital helped her to recuperate from her illness as well as giving us valuable time to closely monitor her for signs for rebleeding, bowel ischaemia secondary to embolisation and effects of massive transfusion. Subsequently, she has been referred to a paediatric gastroenterologist in a tertiary unit for expert opinion, who has not recommended a colonoscopy or further imaging, provided she remains asymptomatic.
She continues to remain asymptomatic at her 4-week surgical follow-up and is back to her normal activities including rugby and dancing.
Discussion
Massive rectal bleeding in the paediatric age group is very rare. A detailed history and thorough clinical examination performed alongside resuscitation is the key to initial management. A full blood count, coagulation profile, liver and renal function test, blood group and crossmatch should be performed. The diagnostic armamentarium for identifying the source of bleeding is vast. This includes endoscopy (upper gastrointestinal endoscopy, flexible sigmoidoscopy and colonoscopy), stool culture, contrast CT scan, radionuclide scan, capsule endoscopy and angiography. Careful thought should be given prior to requesting investigations, taking into account the most likely source of bleeding and the diagnostic and potential therapeutic value of some of these tests. It may be difficult to distinguish colonic AVMs from colonic varicosis on angiography.1
Once the cause of bleeding is identified, specific treatment to control bleeding is initiated. This includes correction of coagulation defect, acid suppression, therapeutic endoscopy (epinephrine injection, clips, banding, electrocautery, polypectomy and argon plasma coagulation), interventional radiology (embolisation) and emergency surgery, depending on the diagnosis. More than one therapeutic modality may be needed to stop the bleeding.
Various terminologies have been used to describe vascular malformations causing gastrointestinal bleeding. They include angiodysplasia, AVM, haemangioma, telangiectasia, vascular ectasia, etc. Angiodysplastic lesions are usually multiple and is thought to represent venous bleeding, whereas AVMs are usually solitary and have been classified into low flow (venous bleeding) and high flow (arterial bleeding).
AVM is an abnormal connection between the arteries and the veins, due to the failure of normal capillary bed development. This leads to shunting of blood between the high-pressure arterial system and the low-pressure venous system. They are usually congenital and the exact aetiology is unknown. The acquired AVMs are either secondary to trauma or due to a degenerative process leading to dilation of blood vessels and formation of AVMs. Although AVMs have been commonly associated with the nervous system (cerebral hemisphere, cerebellum, brain stem and spinal cord), they can occur in other areas including the skin, eyes, solid viscera (liver, spleen and kidneys) and hollow viscera (small and large bowel), etc.
Fortunately, a majority of the AVMs are asymptomatic. Symptomatic AVMs are due to bleeding, pressure effects or shunting of blood between the arterial and venous system causing congestive cardiac failure. Symptoms vary according to the location of the lesion. Cerebral AVMs can present with headache, epilepsy or focal neurological deficit whereas lesions in the bowel commonly present as chronic bleeding. Lesions in the extremities can lead to limb hypertrophy (Parkes-Weber syndrome: port-wine stain, varicose veins and limb hypertrophy).
Investigations that are helpful are CT angiography and MR angiography, but digital subtraction angiography remains the gold standard investigation for the diagnosis of AVM. The main purpose of imaging is not only to identify and locate the lesion but also to delineate the vascular anatomy which guides treatment options. Intestinal AVMs can be diagnosed by endoscopy.
Broadly, treatment options are conservative, embolisation or surgery. In addition, stereo tactic radio surgery could be used for inaccessible lesions in the brain. Skin lesions are treated with compression garments, sclerotherapy or surgery. Intestinal AVMs could be treated endoscopically using electrocautery or injection with sclerosants, surgical excision being reserved for re-bleeding or failure of the above procedures.
Vascular malformation of the colon is a rare cause of per rectal bleeding in a child. Though it tends to affect the right colon predominantly in the adult population, it seems to be commoner on the left side in children.Right-sided2 and left-sided colonic preponderance3 4 have been reported in children, but the study groups have been very small to arrive at a safe conclusion. Surgical resection of the involved segment is the standard treatment in the majority of cases, especially in the emergency setting. Though bleeding from the rectosigmoid area has been reported to be controlled with embolisation coils prior to surgery in the paediatric age group,5 6 after reviewing the English Pub Med and Medline, we believe this is the only reported successful single modality treatment with embolisation for an AVM of the caecum in a child.
Learning points.
Consider interventional radiology even in a paediatric age group to diagnose, localise and treat massive gastrointestinal bleeding.
Multidisciplinary approach and good communication are the key in dealing with such rare emergencies successfully.
Plan investigations based on clinical presentation rather than by ‘protocol’, especially in unfamiliar situations.
Bleeding protocol three-phase CT scan of the abdomen and pelvis should be performed rather than a ‘routine’ contrast CT scan to evaluate gastrointestinal bleeding.
Develop a pathway for managing paediatric gastrointestinal bleeding presenting in a district general hospital.
Acknowledgments
The authors would like to acknowledge Dr Ian Driver, Dr Gary Picken and Mr Visesh Sankaran for their active participation in the management of the patient.
Footnotes
Contributors: All authors contributed to the content and writing of this article.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Defreyne L, Meersschaut V, van Damme S, et al. Colonic arteriovenous malformation in a child misinterpreted as an idiopathic colonic varicosis on angiography: remarks on current classification of childhood intestinal vascular malformations. Eur Radiol 2003;2013:L138–41 [DOI] [PubMed] [Google Scholar]
- 2.Chuang FJ, Lin JS, Yeung CY, et al. Intestinal angiodysplasia: an uncommon cause of gastrointestinal bleeding in children. Pediatr Neonatol 2011;2013:214–18 [DOI] [PubMed] [Google Scholar]
- 3.Abdoon H. Angiodysplasia in a child as a cause of lower GI bleeding: case report and literature review. Oman Med J 2010;2013:49–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De la Torre Mondragon L, Vargas Gomez MA, Mora Tiscarreno MA, et al. Angiodysplasia of the colon in children. J Pediatr Surg 1995;2013:72–5 [DOI] [PubMed] [Google Scholar]
- 5.Natterer J, Joseph JM, Denys A, et al. Life threatening rectal bleeding with Klippel-Trenaunay syndrome controlled by angiographic embolisation and rectal clips. J Pediatr Gastroenterol Nutr 2006;2013:581–4. [DOI] [PubMed] [Google Scholar]
- 6.Pierce J, Matthews J, Stanley P, et al. Perirectal arteriovenous malformation treated by angioembolization and low anterior resection. J Pediatr Surg 2010;2013:1542–5 [DOI] [PubMed] [Google Scholar]


