Abstract
Objectives:
The present study was undertaken to evaluate and highlight the importance of hematological scoring system (HSS) in the early detection of neonatal sepsis.
Materials and Methods:
The cross-sectional study enrolled 110 neonates who were clinically suspected of infection (study group) and normal neonates for comparison (controls), during the 1st week of life. All peripheral blood smears were analyzed using HSS of Rodwell et al., by pathologists blinded to the infection status of the newborns. HSS assigns a score of 1 for each of seven findings significantly associated with sepsis: Abnormal total leukocyte count, abnormal total polymorphonuclear neutrophils (PMN) count, elevated immature PMN count, elevated immature: Total (I:T) PMN ratio, immature: Mature (I:M) PMN ratio ≥0.3, platelet count ≤150,000/mm3, and pronounced degenerative or toxic changes in PMNs. Score of ≤2 was interpreted as sepsis unlikely; score 3-4: Sepsis is possible and ≥5 sepsis or infection is very likely. Blood culture was taken as a standard indicator for septicemia. The perinatal history, clinical profile and laboratory data were recorded and correlated in each case. Each hematological parameter was assessed for its individual performance and also with the culture-proven sepsis. Sensitivity, specificity, positive and negative predictive values (NPVs) were calculated for each parameter and for different gestational ages. P value was also calculated for different parameters.
Results:
Out of the 110 infants, based on clinical findings and laboratory data were classified into three categories: Sepsis (n=42), probable infection (n=22) and normal (n=46). Out of these, 42 (38.2%) newborns had positive blood culture. 63 (57%) neonates were preterm and 47 (43%) term. Male: female ratio was 0.96:1. The P value was significant for the different gestational ages (0.0002) and sex ratio (0.003). Immature polymorphonuclear neutrophils (PMN) count was the most sensitive and I:M PMN ratio, the most specific indicator of sepsis. For sepsis and probable sepsis, I:T PMN count and immature PMN count have highest sensitivity whereas I:T and I:M PMN ratio have highest specificity. HSS has much higher sensitivity and specificity in preterms than in term neonates. Positive predictive value and NPV is also higher in preterm than term for HSS. It was also seen that with increasing scores, the likelihood of sepsis also increased.
Conclusion:
The sensitivities of the various screening parameters were found to be satisfactory in identifying early onset neonatal sepsis. It is a simple and feasible diagnostic tool to guide towards the decision-making for a rationale treatment.
Keywords: Culture, hematological scoring system, neonatal sepsis, polymorph, preterm
INTRODUCTION
Sepsis neonatorum continues to be a major cause of morbidity and mortality in developing countries, but is treatable if diagnosed on time.[1] One to eight cases of neonatal septicemia are reported in all live births.[2] Neonatal sepsis is the response of neonates to any kind of infections. It can be early or late in onset. In early onset, maximum cases are observed within 24 h of life, and smaller percentage thereafter up to 7 days.
The infection can be contracted from the mother via transplacental route, ascending infection, during passage through an infected birth canal, or exposure to infected blood at delivery.[3] The newborn infants are more prone to bacterial invasion than the older children or adults, due to their weaker immune system, premature babies being even more susceptible.[4]
The major concern of the clinicians is its non-specific presentation, sometimes the rapid progression of sepsis and the unavailability of tests with a high positive predictive value (PPV). Therefore, the early detection of neonatal sepsis is a vexing problem. A definite diagnosis is made by blood culture. However, the procedure is time consuming (takes 48-72 h),[5,6] yield is low (8-73%)[5,6,7,8,9] and the facilities for the test might not be available in many laboratories. Other tests for sepsis, like haptoglobin and counterimmunoeletrophoresis are also not easily accessible.[4]
So, the significance of various screening tests, either singly or in combination is observed. The need is for an infallible test for bacteremia's that is easily performed, quick, simple, and cost-effective.
Monroe devised a criteria which used three parameters of total PMN count, immature PMN count and I:T ratio, whereas in this hematologic scoring system, we used even more indices. Here, in this study, we undertake to evaluate the performance of the hematological scoring system (HSS) of Rodwell et al. (1988) in 110 neonates for the early detection of sepsis in high risk infants, which should improve the diagnostic accuracy of the complete blood cell count as a screening test. The present study was undertaken to evaluate and highlight the importance of HSS in the early detection of neonatal sepsis.
MATERIALS AND METHODS
This study is a hospital based cross-sectional study of all the neonates during the 1st week after birth reporting to Pediatrics Department of Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana, Ambala from April to July 2011. Neonates who were clinically suspected to have bacterial infection within 1st week of life, based on perinatal risk factors and clinical features were taken as study group. For comparison neonates reporting to the department for immunization or attending well baby clinics were taken as controls. Infants with <37 weeks gestational age were regarded as preterm and >37 weeks, term.[10]
The study included three categories; category (1) infants with sepsis and positive blood culture; category (2) infants with probable infection and strong clinical history but negative blood culture; category (3) normal infants without any evidence of sepsis.
Under complete aseptic conditions, 0.5-1 ml of blood sample was obtained by peripheral venipuncture. The samples were collected in tripotassium ethylene diamine tetra-acetic acid containing non-siliconized vaccutainer tubes. Sepsis work-up involved complete blood counts along with hematological score and culture. Peripheral blood smears were prepared immediately, stained with Leishman stain and examined under oil-immersion lens of light microscope at a magnification of ×1000. Total leucocyte count reading was obtained by MS 95 automated analyzer and later, corrected for nucleated red blood cells. Differential counts were performed on these smears by counting at least 200 cells. All the peripheral blood smears were analyzed by pathologists blinded to the infection status of these infants, using HSS of Rodwell et al. HSS[11] includes:
White blood cell (WBC) count and its differential
Platelet count
Nucleated red blood cell count (to correct total WBCs count)
Assessment of degenerative and toxic changes in PMNs.
HSS assigns a score of 1 for each of seven findings significantly associated with sepsis: Abnormal total leukocyte count, abnormal total PMN count, elevated immature PMN count, elevated immature to total (I:T) PMN ratio, immature to mature (I:M) PMN ratio ≥0.3, platelet count ≤150,000/mm3, and pronounced degenerative or toxic changes in PMNs. An abnormal total PMN count is assigned score of two instead of 1, if no mature polymorphs are seen on the peripheral smear to compensate for the low I:M ratio [Table 1].
Table 1.
Hematological scoring system
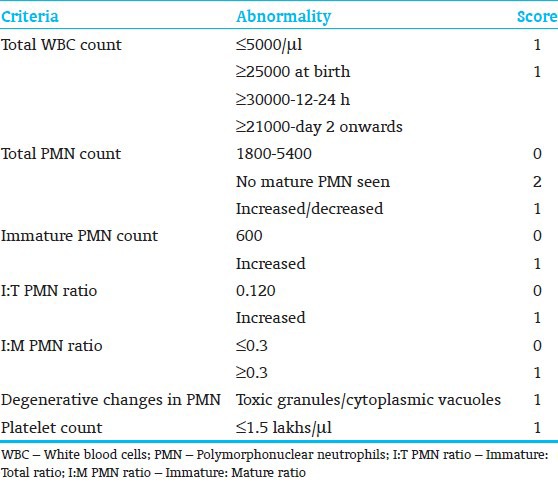
Immature polymorphs include promyelocyte, myelocyte, metamyelocyte and band forms. Band cell is described as a PMN in which the nucleus is indented by more than one-half, but in which the isthmus between the lobes is wide enough to reveal two distinct margins with nuclear material in between. Degenerative changes include vacuolization, toxic granulations and Dohle bodies [Figure 1].
Figure 1.

Peripheral blood film showing band form and toxic granulation (Leishman stain; ×1000)
Score of ≤2 was interpreted as sepsis unlikely; score 3-4: Sepsis is possible and ≥5 sepsis or infection is very likely. Minimum score that can be obtained is 0 and maximum score, 8.
Statistical analysis
Sensitivity, specificity, positive and negative predictive values (NPVs) were calculated for each parameter and for different gestational ages. P value was also calculated for different parameters. Data was compiled and statistically analyzed by using SPSS software.
The research work was approved by the institutional ethical committee and the informed consent was also obtained from the parents of all the neonates.
RESULTS
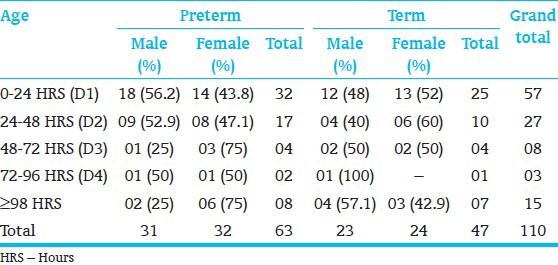
Out of the 110 infants, based on clinical findings and laboratory data were classified into three categories: Sepsis (n=42), probable infection (n=22) and normal (n=46). Of the total, 47 (43%) were term and 63 (57%) preterm. The study had 54 (49.09%) males and 56 (50.90%) females. Maximum 57 (51.81%) neonates presented within the first 24 h of life [Table 2].
Table 2.
Age and sex of the study population
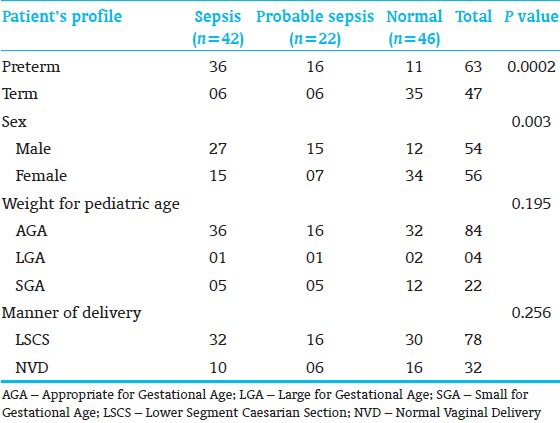
The P value for the various gestational ages and sex ratio was found to be significant [Table 3].
Table 3.
Association of neonatal profile with neonatal sepsis
Out of 42 cases with culture proven sepsis, 35 (83.33%) infants had score ≥5, and 7 (16.67%) had scores 3-4. 12 (54.55%) cases with probable infection had scores 3-4; 6 (27.27%) had score ≥5. 10 (21.74%) of the normal infants had score ≥5 suggesting the presence of sepsis and 13 (28.26%) had scores 3-4 suggesting the possibility of sepsis in these cases. 23 (50%) of the normal infants and 4 (18.18%) with probable infection had score ≤2 which implies that sepsis was unlikely in these cases [Table 4].
Table 4.
Score of each of the categories

Immature PMN count was highly sensitive (96.87%), followed by immature: Total (I:T) ratio (93.75%) and total PMN count (90.62%). Immature: Mature (I:M) PMN ratio (97.22%), followed by I:T PMN ratio (94.44%), degenerative changes (94.44%) and platelet count (94.44%) were highly specific tests for diagnosing sepsis. The PPV was highest with I:M PMN ratio (994.44%) whereas NPV was highest with immature PMN count [Table 5].
Table 5.
The performance of individual hematological parameter in diagnosing neonatal septicemia
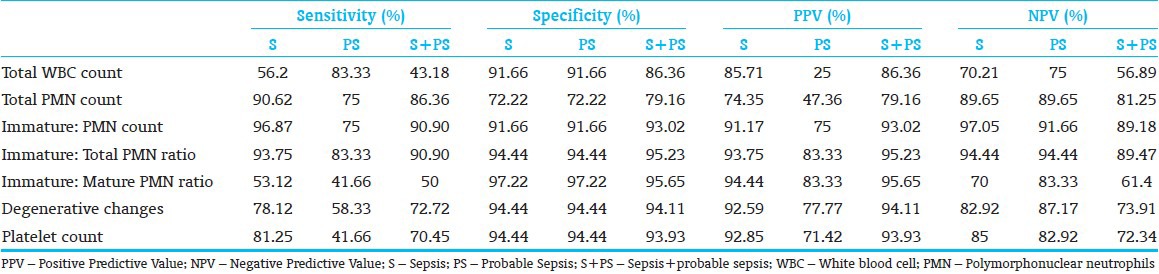
For probable sepsis, both total WBC count and I:T PMN ratio have highest sensitivity of 83.33%. Highest specific parameter is I:M PMN ratio (97.22%) [Table 5].
I:T PMN ratio and I:M ratio have highest PPV of 83.33% and I:T ratio had highest NPV. Thus, for sepsis and probable sepsis, I:T PMN count and immature PMN count have highest sensitivity, whereas I:T and I:M PMN ratio have highest specificity [Table 5].
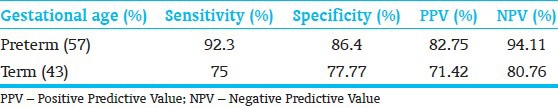
HSS has much higher sensitivity and specificity in pre-terms than in term neonates. PPV and NPV are also higher in preterm than term for HSS [Table 6].
Table 6.
Performance of scoring system in preterm and term infants for sepsis
DISCUSSION
The mortality and the morbidity caused by neonatal sepsis make HSS an important tool in its early diagnosis. It helps in the early intervention compared to the culture reports, which may take days for the positive result and thus, saving the life of many neonates and avoid the unnecessary and prolonged exposure to the antibiotics. Hence, aids to provide a more rational approach in the antibiotic usage. The culture reports may follow later. The results of this study, found out to be more accurate in pre-terms (57%) than in full-term infants (43%), which is further a boon in diagnosing sepsis. This is because, preterm are more susceptible to infections than are the terms, which is due to their poor immune system, low levels of immunoglobulins and low weight at birth.[12]
This scoring system is significant in many other ways also, regarding its easy availability, accessibility, low cost, less time consuming and practically possible in all the laboratories, which makes it convenient for any common man to get a high risk infant tested and diagnosed on time.
Neonatal sepsis is also known as sepsis neonatorum and neonatal septicemia. It is the infection occurring in the newborn infants, the cause for which can be bacterial, viral etc., its diagnosis is very crucial as its presentation is very nonspecific and the death toll is very high, especially in the developing countries.
Maximum cases present on the 1st day of life, with majority in less than 12 h,[13] as is the case in our study, i.e., 51.81% neonates were less than 24 h.
Monroe devised a criteria which used three parameters of total PMN count, immature PMN count and I:T ratio.[14] whereas in this hematologic scoring system, we used even more indices.
In our study, we correlated the sensitivity, specificity, PPV, and NPV of the various parameters with different groups and also with the other studies. Elevated I:T ratio was found to be the most reliable indicator of sepsis in our study, and also in various other studies like those done by Ghosh et al.[4] and Narasimha et al.[15] Immature PMN count and I:T PMN ratio was also a very sensitive indicator of neonatal sepsis. Degenerative changes in the PMNs made no significant contribution in the diagnosis, in this study. Moreover the presence of toxic granules indicates the production of unusual PMNs during infection and stress induced leucopoiesis. They are never seen in healthy babies. Their presence invariably indicates sepsis, but their count is not always increased.[15,16]
Also, in our study, the total PMN count had a limited role in sepsis screening. This finding correlated well with the study done by Akenzua, who inferred that these patients had normal PMN count but the bands forms are raised, and the elevation was often very late and inconsistent.[17]
Thrombocytopenia was frequently associated with sepsis and indicated poor prognosis. This is thought to be due to increased platelet destruction, sequestration secondary to infections, failure in platelet production due to reduced megakaryocytes or damaging effects of endotoxin.[18] This correlated well with various other studies done by Speer et al., Rodwell et al., Philip et al., and Basu et al.[11,19,20,21]
We also found out that higher the score, more are the chances of sepsis and vice versa. The simplification and standardization of the interpretation of this global test is still required.[11] Variety of other rapid detection methods of microorganisms, like DNA probes, automated blood culture system and fluorometric detection systems are available, but HSS can still be used as a screening test for diagnosing sepsis and to differentiate infected neonates from the non-infected ones. Furthermore, the sensitivity and the specificity of the test is also high, with certainty of sepsis increasing with the score.[15,22]
CONCLUSION
The feasibility and the cost effectiveness of the system increase the usefulness of this test. This helps the clinicians to reach a probable diagnosis, decreasing the death toll and institute a rational approach towards the patient medication, i.e., avoiding unnecessary instillation of antibiotics and preventing the development of resistance to these drugs.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Manucha V, Rusia U, Sikka M, Faridi MM, Madan N. Utility of haematological parameters and C-reactive protein in the detection of neonatal sepsis. J Paediatr Child Health. 2002;38:459–64. doi: 10.1046/j.1440-1754.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- 2.Baley J, Goldfarb J. MH, Klaus MH, Fanaroff AA. 4th edition. Philadelphia: WB Saunders Company; 1993. Neonatal infections. Care of the high risk neonate. [Google Scholar]
- 3.Mayuga WA, Isleta PF. Clinical correlation of neonatal and maternal hematological parameters as predictors of neonatal sepsis. PIDSP. 2005;9:36–42. [Google Scholar]
- 4.Ghosh S, Mittal M, Jaganathan G. Early diagnosis of neonatal sepsis using a hematological scoring system. Indian J Med Sci. 2001;55:495–500. [PubMed] [Google Scholar]
- 5.Sharma A, Kutty CV, Sabharwal U, Rathee S, Mohan H. Evaluation of sepsis screen for diagnosis of neonatal septicemia. Indian J Pediatr. 1993;60:559–63. doi: 10.1007/BF02751434. [DOI] [PubMed] [Google Scholar]
- 6.Misra PK, Kumar R, Malik GK, Mehra P, Awasthi S. Simple hematological tests for diagnosis of neonatal sepsis. Indian Pediatr. 1989;26:156–60. [PubMed] [Google Scholar]
- 7.Baltimore RS, Huie SM, Meek JI, Schuchat A, O’Brien KL. Early-onset neonatal sepsis in the era of group B streptococcal prevention. Pediatrics. 2001;108:1094–8. doi: 10.1542/peds.108.5.1094. [DOI] [PubMed] [Google Scholar]
- 8.Gladstone IM, Ehrenkranz RA, Edberg SC, Baltimore RS. A ten-year review of neonatal sepsis and comparison with the previous fifty-year experience. Pediatr Infect Dis J. 1990;9:819–25. doi: 10.1097/00006454-199011000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Varsha, Rusia U, Sikka M, Faridi MM, Madan N. Validity of hematologic parameters in identification of early and late onset neonatal infection. Indian J Pathol Microbiol. 2003;46:565–8. [PubMed] [Google Scholar]
- 10.Arias F, Daftary SN, Bhide AG. Practical Guide to High Risk Pregnancy and Delivery. A South Asian Perspective. 3rd ed. New Delhi: Elsevier; 2008. Preterm parturition syndrome; pp. 193–216. [Google Scholar]
- 11.Rodwell RL, Leslie AL, Tudehope DI. Early diagnosis of neonatal sepsis using a hematologic scoring system. J Pediatr. 1988;112:761–7. doi: 10.1016/s0022-3476(88)80699-1. [DOI] [PubMed] [Google Scholar]
- 12.Bhat YR, Rao A. Sepsis screen in early neonatal sepsis. J Clin Diagn Res. 2010;4:3331–6. [Google Scholar]
- 13.Anwer SK, Mustafa S. Rapid identification of neonatal sepsis. J Pak Med Assoc. 2000;50:94–8. [PubMed] [Google Scholar]
- 14.Bellig L, Ohning B. Neonatal Sepsis. EMedicine Journal Pediatrics/Neonatology. 2003;4(1):6. Thilo EH, Rosenberg AA. Infections of the Newborn. Current Pediatric Diagnosis and Treatment, 14th edition. Hay WW, Hayward AR, Levin MJ, Sondheimer JM: editors. New Jersey: Appleton and Lange, 1999. [Google Scholar]
- 15.Manroe BL, Weinberg AG, Rosenfeld CR, Browne R. The neonatal blood count in health and disease. I. Reference values for neutrophilic cells. J Pediatr. 1979;95:89–98. doi: 10.1016/s0022-3476(79)80096-7. [DOI] [PubMed] [Google Scholar]
- 16.Narasimha A, Harendra Kumar ML. Significance of Hematological Scoring System (HSS) in early diagnosis of neonatal sepsis. Indian J Hematol Blood Transfus. 2011;27:14–7. doi: 10.1007/s12288-010-0050-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akenzua GI, Hui YT, Milner R, Zipursky A. Neutrophil and band counts in the diagnosis of neonatal infections. Pediatrics. 1974;54:38–42. [PubMed] [Google Scholar]
- 18.Zipursky A, Palko J, Milner R, Akenzua GI. The hematology of bacterial infections in premature infants. Pediatrics. 1976;57:839–53. [PubMed] [Google Scholar]
- 19.Speer CP, Gahr M, Schröter W. Early diagnosis of neonatal infection. Monatsschr Kinderheilkd. 1985;133:665–8. [PubMed] [Google Scholar]
- 20.Philip AG, Hewitt JR. Early diagnosis of neonatal sepsis. Pediatrics. 1980;65:1036–41. [PubMed] [Google Scholar]
- 21.Basu S, Guruprasad, Narang A, Garewal G. Diagnosis of sepsis in the high risk neonate using a hematologic scoring system. Indian J Hematol Blood Transf. 1999;17:32–4. [Google Scholar]
- 22.Khair KB, Rahman MA, Sultana T, Roy CK, Rahman MQ, Shahidullah M, et al. Role of hematologic scoring system in early diagnosis of neonatal septicemia. BSMMU J. 2010;3:62–7. [PubMed] [Google Scholar]