Abstract
A 45-year-old patient on lifelong warfarin therapy after a metal aortic valve replacement developed a homonymous visual field defect following an occipital lobe haemorrhage. The patient received only conservative management and yet described continued improvement in her visual field defect for up to 20 months following the initial cerebral insult. We present the first conclusive illustrative documentation of visual recovery in a patient with an occipital lobe haemorrhage with sequential automated perimetric assessments over an extended period of time.
Background
In this case report we describe a patient who developed a homonymous visual field defect following a spontaneous intracranial haemorrhage. For the first time in literature we followed the patient with serial automated perimetric assessments charting resolution of the defect.
We feel this article would appeal to neurologists as well as ophthalmologists caring for patients who have suffered visual field defects following an intracranial insult.
Case presentation
A 45-year-old woman presented to the emergency department with a severe headache of sudden onset. Her medical history included a metal aortic valve replacement for aortic stenosis, for which she was on lifelong warfarin therapy. She was also known to be suffering from mechanical intravascular haemolysis associated with a failing aortic prosthesis. There was no other significant medical or surgical history of note.
Testing of confrontational fields revealed a left homonymous hemianopia, but clinical examination was otherwise unremarkable, with no other neurological deficits. A non-contrast CT scan of the head showed a large intraparenchymal haematoma in the right occipitoparietal area, with associated oedema and midline shift (figure 1). A coagulation screen on admission revealed an international normalised ratio (INR) was 3.9, and this was rapidly reversed by treatment with intravenous prothrombin complex concentrate and vitamin K. Following neurosurgical advice, the patient's haematoma was managed conservatively. The patient remained clinically and neurologically stable following a period of observation, and a repeat CT scan of the head performed 2 weeks postpresentation showed some resolution of the intracranial haematoma. At this point the patient was restarted on low-molecular-weight heparin prior to being restarted on warfarin and discharged from the hospital.
Figure 1.
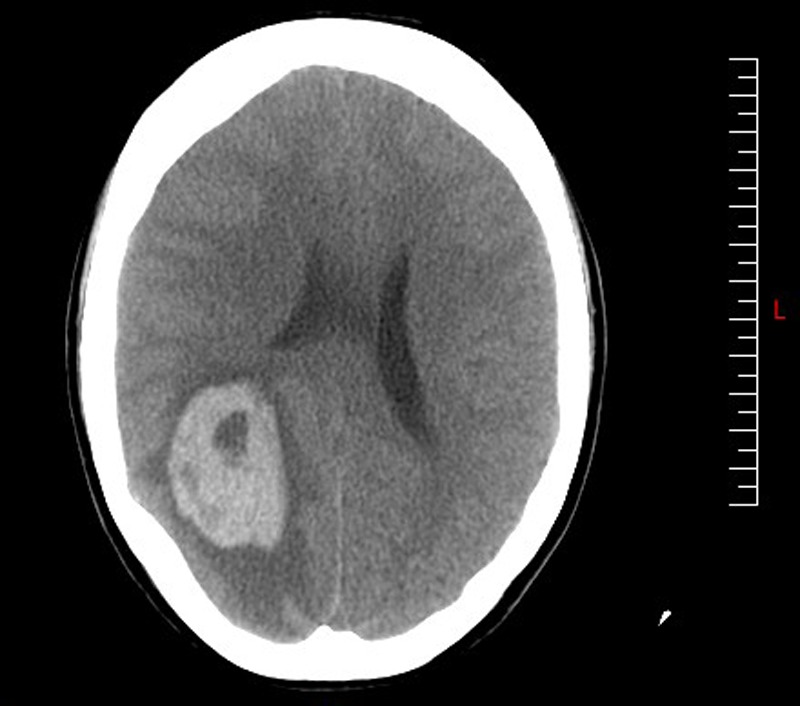
Non-contrast CT head scan performed at onset of symptoms show a large intraparenchyma haematoma in the right occipitoparietal lobe with significant associated oedema and mid-line shift.
The patient was reviewed in a neurosurgical clinic 4 months later. She described a gradual improvement in her visual fields, but with a persisting left-sided defect. At this point the patient was referred to the ophthalmology department for assessment of her visual fields.
On examination, the patient's visual acuities were measured at 6/4−4 in the right eye and 6/5+3 in the left eye. An ocular examination was unremarkable with healthy optic disc appearances and no significant retinal pathology. Automated perimetry testing on a Humphrey visual field analyser II was first performed 7 months postpresentation, and showed a persistent left inferior homonymous quadrantanopia consistent with the occipital location of the haematoma. Further visual field testing performed at 10, 14 and 19 months postpresentation showed gradual resolution of the visual field defect (figure 2). Binocular Esterman visual field tests also showed gradual recovery of central visual field, with the patient eventually achieving fitness to drive under driver and vehicle licensing agency regulations (figure 3).
Figure 2.
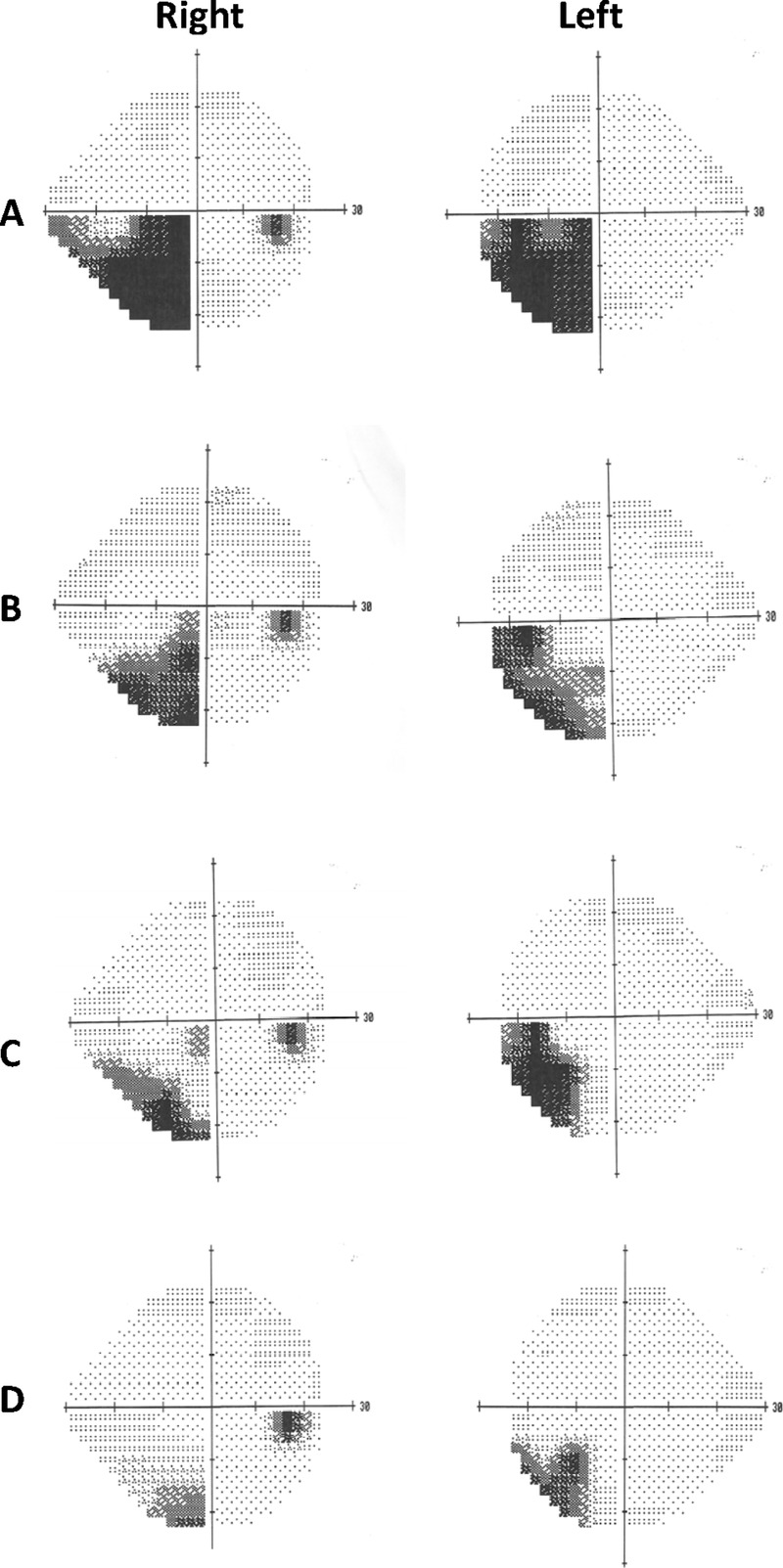
Sequential Humphrey 24-2 automated perimetric visual fields performed at (A) 7 months, (B) 10 months, (C) 14 months and (D) 19 months postinitial intracerebral insult, showing gradual resolution of the left homonymous visual field defect.
Figure 3.
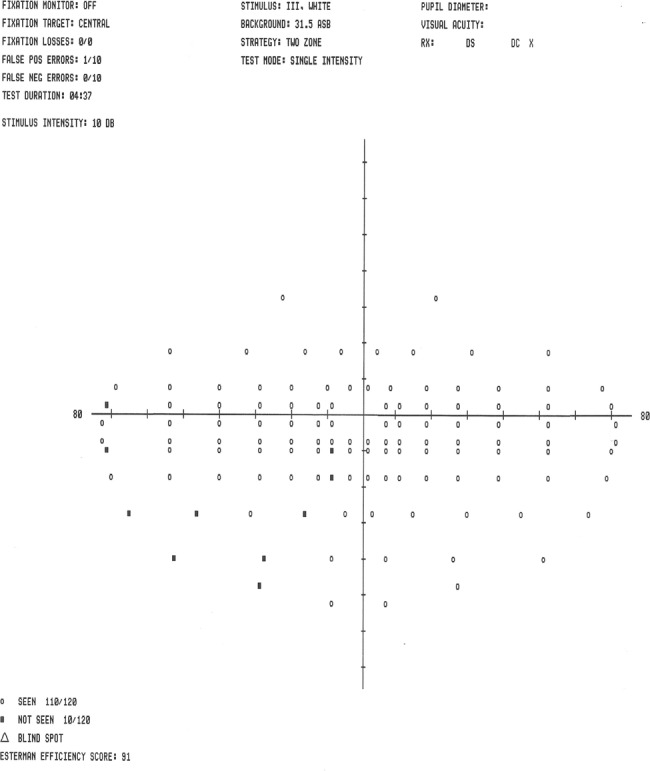
Binocular Esterman visual field test showing preservation of central visual field allowing fitness to drive under driver and vehicle licensing agency regulations.
Discussion
Homonymous hemianopia is a form of visual field defect that can be caused by a variety of cerebral lesions. In adults, a homonymous hemianopia is most commonly caused by a stroke, with an occipital infarct being the commonest underlying pathology.1–3 In fact, on careful examination 20% of patients with an acute stroke will show clinical evidence of a hemianopic field defect.4
Homonymous hemianopias are often very disabling, with patients reporting difficulties with reading and visual scanning. They may fail to notice relevant objects or avoid obstacles on the affected side, and collide with approaching people or cars.5 The homonymous visual field defect may also affect their legal ability to drive.6 7 This can have significant consequences on the patient functional independence and ability to maintain employment. Patients and caregivers are therefore often keen to obtain information regarding the timescale and prognosis for visual recovery.
Studies of visual field recovery in homonymous hemianopias suggest that spontaneous improvement of visual field defect occurs in nearly 40% of patients.8 In most cases the improvement is usually seen within the first 3 months following the intracranial insult.8–10 Improvement after 6 months from injury was often mild, and thought to be related to improvement of the underlying disease or increased ability at performing the visual field test reliably on follow-up visits.8 11 Our patient however, described continued objective, improvement in her visual fields for up to 20 months following the initial cerebral insult. We speculate that the improvement demonstrated in this patient may be due to a difference in the underlying pathology. Our patient's homonymous hemianopia was caused by a primary intracranial haemorrhage, whereas, in the above studies of visual recovery in homonymous hemianopias, the causative insult was most commonly a cerebral infarct.8–11 Reversing anticoagulation in patients with proembolic states who have suffered an intracranial haemorrhage is always a balance of risks and benefits. Stopping anticoagulation for 7–14 days appears to be generally well tolerated, but should only be undertaken after discussion with senior stroke or neurosurgical physicians.12
Our case report is the first to our knowledge to conclusively document visual recovery in a patient with an occipital lobe haemorrhage with sequential automated perimetry over an extended period of time. Although the patient did initially present with a left homonymous hemianopia on confrontational fields testing, no formal perimetric visual fields were obtained until the patient was referred to the ophthalmology services 6 months later. By this time, the patient had reported a subjective improvement in her visual field symptoms. We were subsequently only able to demonstrate a left homonymous inferior quadrantanopia, in keeping with the occipitoparietal location of the intracranial haemorrhage.
Automated perimetry appears to be a more sensitive method of accurately assessing visual field defects following a stroke compared with non-perimetric confrontational assessment, and can be useful in decision-making regarding eligibility for driving13 14 (figure 3). In addition, anecdotally, patients who are improving seem to benefit psychologically from being shown objective evidence of their clinical improvement. We would propose setting up a study to assess patients’ perspectives on formalised perimetric visual field testing following an intracranial event. In the future we feel that automated perimetric assessments of visual fields would be a useful adjunct in the assessment and rehabilitation of stroke patients with homonymous visual field defects.
Learning points.
Hemianopic visual field defects are present in up to 20% of patients who have suffered an acute stroke. Initial work-up of such patients should therefore include an assessment of visual fields by both confrontational fields testing and automated perimetric testing if possible.
Homonymous hemianopias following acute cerebrovascular events can show continued improvement for up to 20 months following the intracranial insult, although in most cases the improvement is usually seen within the first 3 months.
Automated perimetry can be used to accurately assess baseline visual field defects following a stroke, as well as objectively document any improvements. It can also be useful in decision-making regarding eligibility for driving.
Footnotes
Contributors: SL wrote the manuscript. BZG edited the manuscript. NJW-H edited the manuscript and provided advice on the final draft.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Zhang X, Kedar S, Lynn MJ, et al. Homonymous hemianopia in stroke. J Neuroophthalmol 2006;2013:180–3 [DOI] [PubMed] [Google Scholar]
- 2.Trobe JD, Lorber ML, Schlezinger NS. Isolated homonymous hemianopia. A review of 104 cases. Arch Ophthalmol 1973;2013:377–81 [DOI] [PubMed] [Google Scholar]
- 3.SMITH JL. Homonymous hemianopia. A review of one hundred cases. Am J Ophthalmol 1962;2013:616–23 [PubMed] [Google Scholar]
- 4.Isaacs B, Marks R. Determinants of outcome of stroke rehabilitation. Age Ageing 1973;2013:139–49 [DOI] [PubMed] [Google Scholar]
- 5.Pambakian AL, Kennard C. Can visual function be restored in patients with homonymous hemianopia? Br J Ophthalmol 1997;2013:324–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DVLA. 2012. At a glance: Guide to the current Medical Standards of Fitness to Drive. (Issued by the Drivers Medical Group DVLA)
- 7.Royal College of Ophthalmologists. 2005. Visual standards for driving. http://www.rcophth.ac.uk/core/core_picker/download.asp?id=214.
- 8.Zhang X, Kedar S, Lynn MJ, et al. Natural history of homonymous hemianopia. Neurology 2006;2013:901–5 [DOI] [PubMed] [Google Scholar]
- 9.Gray CS, et al. Recovery of visual fields in acute stroke: homonymous hemianopia associated with adverse prognosis. Age Ageing 1989;2013:419–21 [DOI] [PubMed] [Google Scholar]
- 10.And KT, Kolmel HW. Patterns of recovery from homonymous hemianopia subsequent to infarction in the distribution of the posterior cerebral artery. Neuroophthalmology 1991;2013:33–9 [Google Scholar]
- 11.Messing B, Ganshirt H. Follow-up of visual field defects with vascular damage of the geniculostriate visual pathway. Neuroophthalmology 1987;2013:231–42 [Google Scholar]
- 12.Phan TG, Koh M, Wijdicks EF. Safety of discontinuation of anticoagulation in patients with intracranial hemorrhage at high thromboembolic risk. Arch Neurol 2000;2013:1710–13 [DOI] [PubMed] [Google Scholar]
- 13.Çelebisoy M, Çelebisoy N, Bayam E, et al. Recovery of visual-field defects after occipital lobe infarction: a perimetric study. J Neurol Neurosurg Psychiatry 2011;2013:695–702 [DOI] [PubMed] [Google Scholar]
- 14.Townend BS, et al. Perimetric homonymous visual field loss post-stroke. J Clin Neurosci 2007;2013:754–6 [DOI] [PubMed] [Google Scholar]


