Abstract
Background:
Neonatal jaundice (NNJ) is a major cause of morbidity and mortality among neonates in Nigeria and exchange blood transfusion (EBT) is a common modality of its treatment in Ebonyi State University Teaching Hospital (EBSUTH), Abakaliki. This communication aims to audit this service.
Materials and Methods:
A 3-year retrospective review of the case files of all neonates that had EBT for NNJ at the new born special care unit of EBSUTH.
Result:
Two hundred and thirty seven (17.25%) out of 1374 neonatal admissions had NNJ. EBT was performed for 40 (16.9%) of them. The commonest indications for EBT were low birth weight/prematurity, ABO blood group incompatibility, sepsis and glucose 6 phosphate deficiencies. The mean serum bilirubin at which EBT was done was 28.3 mg/dl. The EBT was uneventful in 36 cases while in four (10%) cases there were reported adverse events. Seven neonates (17.5%) died after the procedure and documented causes of death include bilirubin encephalopathy, respiratory failure, and septic shock and disseminated intravascular coagulopathy.
Conclusion:
There is high rate of EBT use in the management of severe neonatal hyperbilirubinemia with significant morbidity and mortality in this study site. There is need to review the contribution of factors such as late presentation in the hospital to this and proffer solutions to it.
Keywords: Adverse effect, exchange blood transfusion, mortality, neonatal jaundice
INTRODUCTION
Severe neonatal Jaundice (NNJ) is a major cause of morbidity and mortality among neonates in Nigeria, the impact of its long-term sequel of hearing deficit and cerebral palsy is profound.[1] Neonatal jaundice was observed to be responsible for 1/3rd of the cerebral palsy cases in a pediatric neurology clinic in Nigeria.[2] In view of these serious outcomes, the goals in managing any infant with severe neonatal jaundice is to rapidly reduce the serum bilirubin level by using phototherapy and exchange blood transfusion (EBT).[1,3,4] While the effectiveness of these treatment modalities is not disputed, EBT is now infrequently performed in developed countries of Europe and North America because of the use of Rhogam to prevent rhesus isoimmunization, effectiveness of phototherapy and the morbidity and mortality associated with EBT.[4,5,6]
In Nigeria and other developing countries EBT is still widely used in the management of severe NNJ, a recent report in Nigeria showed that more than 5% of neonates admitted into a new born unit had EBT done[3] while in Iran about 68 cases of EBT were performed over a 3-year period.[7] A major drawback in determining the rightness or otherwise of the different management protocols is because levels at which EBT should be done were not determined by any scientific trials and recommended threshold levels are somewhat arbitrary.[8]
The mortality rate associated with this procedure has been reported to range from 0.4% to 3.2%.[5,7,9,10] Reports from Nigeria give conflicting results of 0.34% in Ibadan and 10% from Ilesha,[3] this wide range is because what is defined as EBT related death do not have a uniform interpretation. Complications associated with EBT include that arising from umbilical catheterization, metabolic disorders, transmission of diseases and blood transfusion reactions.[7,9,10] EBT is still done routinely in neonatal units in Nigeria due to a variety of reasons including poor and irregular power supply, shortage of facilities and late presentation.[3]
Ebonyi state university teaching hospital (EBSUTH), Abakaliki is a state-owned Teaching Hospital located in Abakaliki the capital of Ebonyi State in south eastern Nigeria; it serves Ebonyi State with a population of 2 million and neighboring states. The new born special care unit is run by two consultants and four resident doctors that offer 24 hours coverage of the facility.
This communication is intended to review the morbidity and mortality associated with EBT in EBSUTH, Abakaliki, a tertiary referral centre located in the South Eastern Nigeria. This should serve as an audit of the EBT services offered in this center with an aim of developing improved services.
MATERIALS AND METHODS
This is a retrospective review of the medical records of all cases admitted into the new born special care unit of the EBSUTH, Abakaliki which is one of 2 tertiary hospitals in Ebonyi State in the south east of Nigeria over a 3-year period between 1st January 2007 and 31st December 2009. Cases that had EBT done for neonatal jaundice were the subjects of this study. Excluded from the study were those for which EBTs were done for other reasons including anemia, polycythemia or sepsis. However, children with jaundice in association with or secondary to sepsis were included.
In our center, phototherapy and EBT are the only procedures for management of NNJ. In otherwise healthy term neonates with birthweight ≥ 2.5kg EBTs were done at serum bilrubim of ≥ 20mg/dl while in very ill-term babies or those with features of kernicterus, EBT were done at SB lower than 20 mg/dl. For very low birth weight infants weighing less than 1.5 kg they are routinely placed on prophylactic phototherapy and EBTs were done at much lower SB levels of between 10 and 15 mg/dl depending on their birth weight and how sick they were.
The EBTs were done by resident doctors using fresh whole blood usually less than 72-hour old, ABO and Rhesus compatible with both mother and baby. The double volume exchange procedure was generally completed in 60-90 minutes by repeatedly removing and replacing small aliquots of blood (5 ml/kg) according to standard published procedure.[9] One milliliter of calcium gluconate 10% was given after exchange of every 100 ml of blood.
Data collected from the case records include patients’ age, sex, age at onset of jaundice, age at EBT, conditions during EBT, types of adverse events, frequency of EBT, etiology of neonatal jaundice as documented in the case record were classified as low birth weight/prematurity if the babies birthweight was <2.5kg but ≥1.5kg and do not have any other obvious cause of hemolysis; very low birth weight/ prematurity if their birth weight was <1.5kg. ABO disease was defined as jaundice in a newborne with type A or B antigen borne to type O mother while Rhesus disease was defined as jaundice in Rh-positive newborne delivered to a Rh-negative mother, a positive coombs test against these antigens were supportive evidence but was not always obtained. Sepsis was diagnosed clinically with or without positive blood culture and Glucose-6-phosphate deficiency (G-6-PD) was dependent on a deficient Glucose-6-Phosphate in a jaundiced neonate. Bilirubin level before and after EBT was documented and outcome, which was classified as discharged and death, and causes of death. Analysis was performed using simple statistical methods.
RESULTS
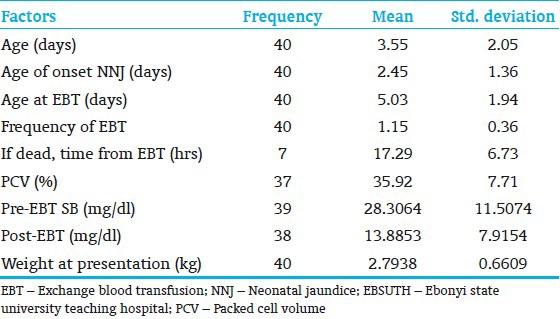
There were 1374 neonatal admissions of which 237 (17.25%) neonates had neonatal jaundice. Forty neonates (16.88%) had EBT done for neonatal jaundice during the study period. There were 24 males and 16 females giving a male: female ratio of 1.5:1. [Table 1] shows the description of the clinical characteristics of the subjects, the average age of the neonates was 3.55±2.05 days the range was from 1 to 10 days and their mean weight was 2.80 kg±0.67 kg with range of 0.8 to 4.35 kg. The age at onset of jaundice varied from the 2nd day of life to the 10th day with a mean of 2.45 day±1.36 (in 36 neonates the onset was on or before the 3rd day of life). The mean pre-EBT serum bilirubin was 28.3 mg/dl±11.51 and the post-EBT serum bilirubin was 13.89 mg/dl±7.92, while their packed cell volume was 35.92%±7.71.
Table 1.
Descriptive statistics of the neonates that had EBT done for NNJ in EBSUTH
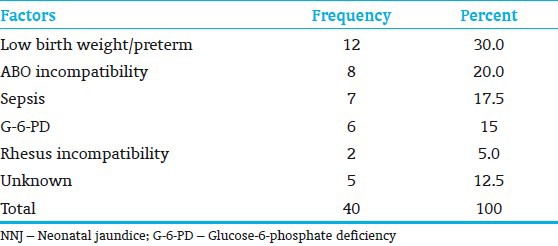
The etiologies of NNJ are highlighted in [Table 2]. The most common causes of neonatal jaundice were prematurity/low birth weight 12 (4(33.3%) of them were low birth weight while 8 (66.7%) were very low birthweight), ABO incompatibility 8 (7 (87.5%) had BO incompatibility mothers’ blood group was O and baby of blood group B while 1 (12.5%) baby had AO incompatibility in which mother had blood group O and baby had blood group A), Glucose-6-phosphate deficiency and sepsis. EBT was completed in 39 (97.5%) children while in 1 (2.5%) the procedure had to be suspended. The procedure was uneventful in 36 children while in four cases (10%), the procedure the children had problems, fever 1 (2.5%), gasping 1 (2.5%), gut perforation 1 (2.5%), and respiratory arrest 1 (2.5%). At the end of the procedure 33 (82.5%) children were assessed as being stable, 5 (12.5%) were unstable and the remaining 2 (5.0%) had cyanosis and encephalopathy, respectively.
Table 2.
Etiology of NNJ
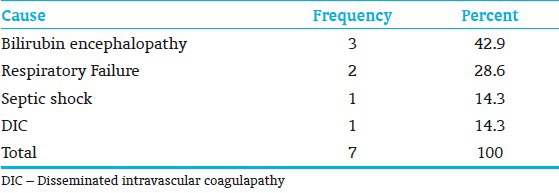
Seven children (17.5%) died after the procedure. The mean duration of interval between the procedure and death was 17.29 hours±6.73. The most common documented cause of death was bilirubin encephalopathy 3 (42.9%), other causes include respiratory failure 2 (25.8%), septic shock 1 (14.3%), and disseminated intravascular coagulopathy 1 (14.3%) [Table 3].
Table 3.
Cause of death
DISCUSSION
The EBT rate of 17% in the management of severe neonatal Hyperbilirubinemia in this study is high. However, similar findings were reported from previous Nigerian studies and from other developing countries.[3] This differs from what is obtainable in developed countries of North America and Europe where EBT is now rarely done because of the availability of powerful and efficient phototherapy units.[4,5,6] Other proffered reasons for these dissimilarities include the recent introduction of new forms of interventions like the use of supplementary fiberoptic phototherapy blankets, prophylaxis with metallo-porphyrins and casein-containing infant formulae.[11,12] This has reduced the need for EBT. Unfortunately, these interventions are not yet available in most developing countries including Nigeria. The present study shows surprising similarity with the finding in Canada with an EBT rate of 22.1% for NNJ.[13] This high rate was attributed to early discharge of babies from nurseries, under recognition and inadequate investigation for severe hyperbilirubinemia. This led to increased rate of re-admission and re-emergence of kernicterus in Canada.[13] The contribution of early discharge from hospital was not sought for in this report but delayed presentation may have been contributory. There was on the average 48-hour delay between onset of NNJ and hospital presentation. The effectiveness of the phototherapy units is also questionable since on the average the babies spend 24 hours on phototherapy but still needed EBT. This may be due to the shortage of modern phototherapy units which can be used to administer intensive phototherapy and the frequent cuts in power supply.
The relative rarity of rhesus isoimmunization as an etiological factor of NNJ in Nigeria is also confirmed in this report.[1,3] Among the 40 neonates with NNJ that had EBT, only two were due to rhesus isoimmunization. Prematurity/ low birth weight was the most common cause, followed by ABO isoimmunization, sepsis and G-6-PD. This finding is similar to previous reports from Nigeria.[1,3] The high contribution of G-6-PD, an X-linked recessive disorder to the etiology of NNJ in this study could have contributed to the observed male predominance among the neonates that had EBT. George et al.[14] reported G-6-PD to be responsible for about half of the neonates with NNJ in Port Harcourt Southern Nigeria and NNJ were more severe among male neonates with G-6-PD.
In this study, approximately 10% of the patients had problems resulting from the procedures including fever, gasping, gut perforation and respiratory arrest compared to 12% in the Iranian study who developed apnea following the procedure.[7] Hypocalcemia, thrombocytopenia, hyponatremia and hypoglycemia which were the most common complications noted by Jackson[9] in Washington and Badie[7] in Iran were absent in this series probably because these were asymptomatic laboratory findings that were not routinely checked for in this center. However, hypocalcemia and thrombocytopenia were unlikely to occur prominently in these patients because calcium gluconate were routinely given to these patients and fresh blood that were at most 48-hours old were used for the EBTs.
The mortality rate of 17.5% in this study is obviously higher than the widely varying figures of 0.34% - 10% obtained from earlier studies in Nigeria.[3] This wide variation is probably because what was defined as EBT related death do not have a uniform interpretation.[3] The mortality rate from studies outside Nigeria on the other hand revealed lower ranges of 0.5% in USA, 0.75% in Greece to 1.5% obtained in Iran.[7] This very low mortality were obtained in spite of very low EBT rate with expected reduced skill in performance of these procedure and may be due to early intervention and stricter definition of EBT-related mortalities. The higher mortality rate obtained from the study may have resulted from late presentation, most of the infants with severe NNJ were admitted from outside because of the hospital policy of discharge of well neonates within 24 hours of delivery. Some researchers have demonstrated that measuring the serum bilirubin level within the first 24 hours of life is helpful in predicting which infants will experience severe hyperbilirubinemia.[14] The other possible explanation is delay in commencing therapy in the affected neonates; this is mainly for financial reasons since parents had to pay for investigations and the materials for the EBTs. One also wonders that in spite of the recent promotion of a less aggressive approach to the management of NNJ and the adoption of higher bilirubin values in which EBTs should be done by AAP,[8,15] is it not likely that Nigerian neonates may need a more aggressive approach with the threshold for EBT set at lower levels in order to achieve a better result, considering that the high morbidity and mortality was despite that the bilirubin levels at which these EBTs were done were within the recommended levels.
CONCLUSIONS
High rate of EBT use in the management of severe neonatal hyperbilirubinemia and significant morbidity and mortality has been demonstrated in this study. The role played by certain factors such as late presentation to the hospital and lack of facility to provide qualitative and intensive phototherapy cannot be overlooked. Provision of regular power supply and overhauling existing health facilities such that there will be provision of intensive and qualitative phototherapy will reduce the requirement for EBT. Health education of the general population, especially pregnant women on the risk of NNJ and the need for early presentation to hospital will greatly reduce the need of EBT and its associated risk.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ibe BC. Neonatal Jaundice. In: Azubuike JC, Nkangineme KE, editors. Paediatrics and child health in a tropical region. Owerri: African Educational services; 1999. pp. 204–11. [Google Scholar]
- 2.Asindi AA. The pattern of neurological disabilities in children seen at the University of Calabar Teaching Hospital. Nig J Paediatr. 1986;13:127–31. [Google Scholar]
- 3.Owa JA, Ogunlesi TA. Why we are still doing so many exchange blood transfusion for neonatal jaundice in Nigeria. World J Pediatr. 2009;5:51–5. doi: 10.1007/s12519-009-0009-2. [DOI] [PubMed] [Google Scholar]
- 4.Hansen TW. Acute management of extreme neonatal jaundice – the potential benefits of intensified phototherapy and interruption of enterohepatic bilirubin circulation. Acta Paediatr. 1997;86:843–6. doi: 10.1111/j.1651-2227.1997.tb08608.x. [DOI] [PubMed] [Google Scholar]
- 5.Steiner LA, Bizzarro MJ, Ehrenkranz RA, Gallagher PG. A decline in the frequency of neonatal exchange transfusions and its effect on exchange-related morbidity and mortality. Pediatr. 2007;120:27–32. doi: 10.1542/peds.2006-2910. [DOI] [PubMed] [Google Scholar]
- 6.Maisels MJ. Why use homeopathic doses of phototherapy? Pediatr. 1996;98:283–7. [PubMed] [Google Scholar]
- 7.Badie Z. Exchange transfusion in neonatal hyperbilirubinaemia: experience in Isfahan, Iran. Singapore Med J. 2007;48:421–3. [PubMed] [Google Scholar]
- 8.Watchko JF. Vingintiphobia revisited. Pediatrics. 2005;115:1747–53. doi: 10.1542/peds.2004-1748. [DOI] [PubMed] [Google Scholar]
- 9.Jackson JC. Adverse events associated with exchange transfusion in healthy and ill newborns. Pediatrics. 1997;99:E7. doi: 10.1542/peds.99.5.e7. [DOI] [PubMed] [Google Scholar]
- 10.Behjati S, Sagheb S, Aryasepehr S, Yaghmai B. Adverse events associated with neonatal exchange transfusion for hyperbilirubinemia. Indian J Pediatr. 2009;76:83–5. doi: 10.1007/s12098-009-0033-1. [DOI] [PubMed] [Google Scholar]
- 11.Mills JF, Tudehope D. Fibreoptic phototherapy for neonatal jaundice. Cochrane Database Syst Rev. 2001;1:CD002060. doi: 10.1002/14651858.CD002060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gourley GR, Kreamer BL, Cohnen M. Inhibition of betaglucuronidase by case in hydrolysate formula. J Pediatr Gastroenterol Nutrit. 1997;25:267–72. doi: 10.1097/00005176-199709000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Sgro M, Campbell D, Shah V. Incidence and causes of severe neonatal hyperbilirubinemia in Canada. CMAJ. 2006;175:587–90. doi: 10.1503/cmaj.060328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Randev S, Grover N. Predicting neonatal hyperbilirubinemia using first day serum bilirubin levels. Indian J Pediatr. 2010;77:147–50. doi: 10.1007/s12098-009-0335-3. [DOI] [PubMed] [Google Scholar]
- 15.American Academy of Pediatrics, Subcommittee on hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 weeks or more gestation. Pediatrics. 2004;114:297–316. doi: 10.1542/peds.114.1.297. [DOI] [PubMed] [Google Scholar]


