Abstract
Internal hernias of the abdomen are uncommon. They represent less than 1% of bowel obstruction cases. The left Paraduodenal hernia (PH) is the most frequent type of internal hernias. We report a case of 77 year- old woman consulting for bowel obstruction evolving since two days. The abdominal computed tomography revealed a retroperitoneal small bowel contained in a peritoneal sac. The surgical exploration confirmed the diagnosis of a left internal PH by showing incarcerated jejunal loops in a PH through a narrow opening to the left of the angle of Treitz. A surgical reduction of the hernia and closure of the hernia neck were performed. The follow-ups were uncomplicated. Through this observation and a literature review, we try to recall the clinical and radiological characteristics of this disease and to clarify the therapeutic modalities.
KEYWORDS: Computed tomography, internal hernia, paraduodenal hernia, small bowel obstruction
INTRODUCTION
Internal hernias are an uncommon cause of bowel obstruction, accounting for less than 1% of cases.[1] Paraduodenal hernia (PH) represents the most common type of congenital internal hernia. It can be asymptomatic, causes chronic abdominal pain or presents with acute intestinal obstruction. The diagnosis of this congenital malformation is often made during surgical intraoperative exploration for intestinal obstruction.
CASE REPORT
It's about a 77 year-old woman consulting for an acute bowel obstruction evolving since two days. Physical examination showed a discrete abdominal distension and slight tenderness in the epigastric and the left upper quadrant. The digital rectal examination found anempty rectal vault. The abdominal X-ray showed an air-fluid small bowel levels. The computed tomography (CT) showed the presence of a jejunal loop contained in a retroperitoneal sac interposed between the stomach pushed forward, the tail of the pancreas to the right and back and the left colon to the left and back [Figure 1]. The mesenteric vessels of these loops were stretched with displacement of the inferior mesenteric artery to the left. The diagnosis of a left PH complicated with acute bowel obstruction has been well discussed. The patient was operated emergency by median laparotomy. Surgical exploration found about 40 cm of proximal healthy small bowel in an internal left paradoudenal hernia. The neck hernia was 3 cm of diameter. After reduction of intestinal loops, the hernia orifice was sutured. The postoperative course was uncomplicated. The patient remained asymptomatic after 18 months of follow-up.
Figure 1.

Abdominal CT showing the presence of dilated loops in the back cavity of the omentum interposed between the pancreas (1) stomach (2) and the descending colon (3)
DISCUSSION
An internal hernia is a protrusion of bowel through abnormal orifice in the peritoneum or mesentery,[2] it account for only 0.25-0.9% of all patients with small intestinal obstructions.[3] Based on the former definition, the most commonly seen hernia types are as follows: Paraduedonal, transmesenteric, pericecal, intersigmoid, supravesical, foramen Winslow, retroanastomotic, and omental hernias. PH was first defined by Treitz in 1857. PH is the most common form of congenital internal hernia, making up 53% of all reported cases.[4] The left sided hernias are more common than right sided ones, representing 75% of cases [Figure 2].[5]
Figure 2.
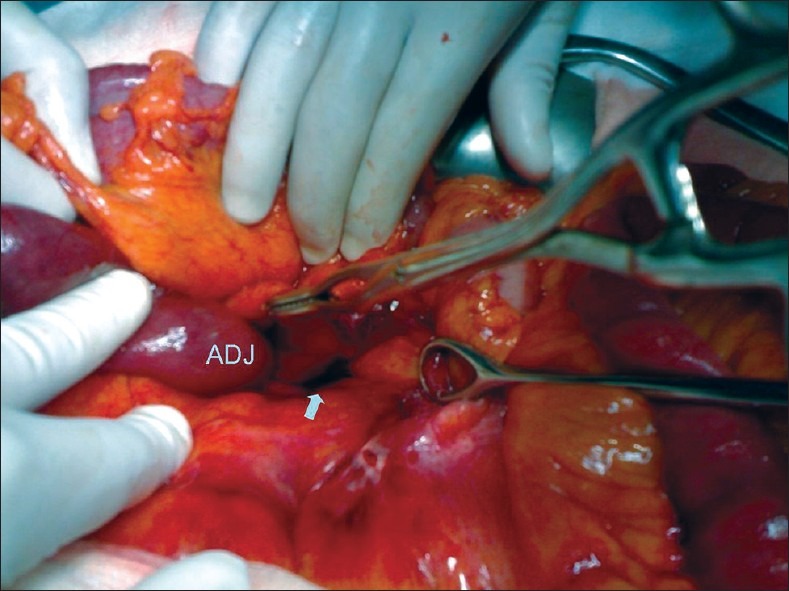
peroperative view: the neck of the hernia (arrow) on the left side of the duodeno-jejunal junction (ADJ)
Paraduedonal hernias result from abnormal rotation of the midgut during embryonic development [Figure 3].
Figure 3.
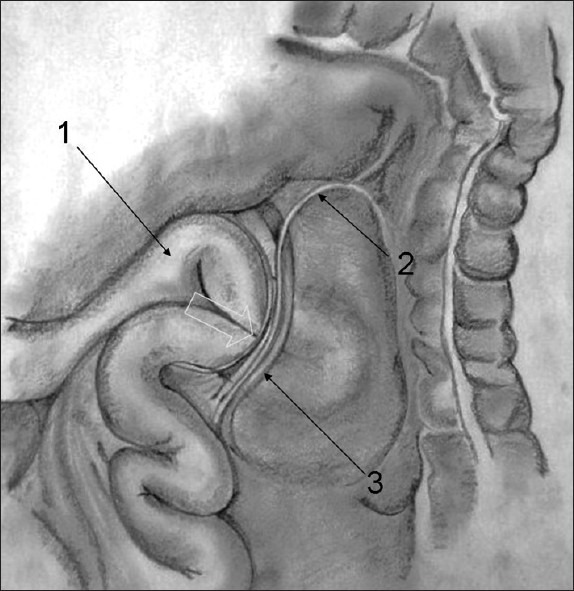
Left parduodenal hernia: Landzert's parduodenal fossa (arrow), (1) The fourth portion of the duodenum, (2) Inferior mesenteric vein, (3) Left colic artery
Although PH is congenital, most cases are discovered between the 4th and 6th decades of life with mean age about 38.5 years,[5] they are exceptionally manifested in the elderly patients over 75 years old. Men are commonly 3 times more affected than women.
The clinical presentation is no specific. Some of internal hernia may remain asymptomatic during the whole life time. About 10% to 15% of cases are discovered preoperatively.[6] Often, the clinical signs are dominated by periombilical cramps or postprandial epigastric pain, nausea, vomiting and so rarely the presence of an abdominal mass in the left side of the abdomen. But the most common presentation of left PH is acute small bowel obstruction.
At least 50% of patients with PH ultimately develop intestinal obstruction.[7] Regarding the risk of incarceration of PH witch mortality as higher as 20-50%, it is recommended that all cases of PH, including asymptomatic ones, should be surgically corrected.[8]
The classic radiological findings of left PH were originally described from the small bowel follow-through examination. Abdominal CT has now become the study of choice to provide the correct diagnosis during symptomatic periods. Left PH have a characteristic appearance of a formation include clustering of small bowel loops, a saclike mass with encapsulation at the ligament of Treitz, duodenojejunal junction depression, mass effect on the posterior stomach wall, engorgement and crowding of the mesentery vessels with frequent right displacement of the main mesenteric trunk, and depression of the transverse colon.[9] Anterior and upward displacement of the inferior mesenteric vein that lies in the ventral circumference of the hernia orifice has been postulated as an additional diagnostic feature on CT. The preoperative diagnosis of these internal hernias could be often unknown even after CT well guided, its discovery sometimes occurs during surgery.
After diagnosis of PH is made, the treatment is surgical. The contents of PH should be reduced manually. If it's difficult to reduce because of its bulky size or adhesions within the sac, an incision in the avascular portion of the hernia sac to the right side of the inferior mesenteric vessels, can be made so to enlarge the neck hernia. During this procedure, it's important to consider the relationship with the inferior mesenteric vessels to avoid injury of these structures. The defect is dealt with in two ways, either by simple closure or by wide opening of the sac by making it continuous with the peritoneal cavity. Intestinal resection is necessary in cases of unhealthy small bowel.
Since 1998, Uematsu reported the first laparoscopic repair of PH,[10] the laparoscopic approach has been reported as a way of diagnosis and repair of PH in many literature reports. As with open repair, laparoscopic repair of PH can be performed either by wide extension or by surgical closure of the hernia defect. Although laparoscopic repair would be expected to reduce postoperative pain and the hospital stay, the paucity of data precludes any final conclusions regarding these issues as well as rates of recurrence. The current data suggest that acute small bowel obstruction can be managed by laparoscopy in selected cases.
CONCLUSION
Although relatively uncommon, left PH should be included in the differential diagnosis of small bowel obstruction despite any history of previous abdominal surgery. The combination of a high index of suspicion, familiarity with this disease entity, and modern imaging technology make preoperative diagnosis easier today. Surgical treatmentis the treatment of choice.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mathias J, Bruot O, Ganne P A, Laurent V, Regent D. Hernies internes. EMC Radiodiagnostic - Appareil digestif 33-015-A-37-2 [Google Scholar]
- 2.Khalaileh A, Schlager A, Bala M, Abu-Gazala S, Elazary R, Rivkind AI. Left laparoscopic paraduodenal hernia repair. Surg Endosc. 2010;24:1486–9. doi: 10.1007/s00464-009-0794-7. [DOI] [PubMed] [Google Scholar]
- 3.Huang YC, Chen HL, Hsu WM, Chen SJ, Lai MW. Left paraduodenal hernia presenting as intestinal obstruction: Report of one case. Acta Paediatr Taiwan. 2001;42:172–4. [PubMed] [Google Scholar]
- 4.Brigham RA, D’Avis JC. Paraduodenal hernia. In: Nyhus LM, Condon RE, editors. Hernia. 3rd ed. Philadelphia PA: JB Lippincott; 1989. pp. 481–6. [Google Scholar]
- 5.Singh RR, Warren P, Smith P, Wilson W. Image of the month. Paraduodenal Hernia. Arch Surg. 2006;141:711–2. doi: 10.1001/archsurg.141.7.711. [DOI] [PubMed] [Google Scholar]
- 6.SocasMacías M, Alamo Martín JM, Suárez Grau JM, Suárez Artacho G, Tejada A, Martín Cartes J, et al. A typical left paraduodenal hernia. Rev Esp Enferm Dig. 2006;98:473–5. doi: 10.4321/s1130-01082006000600008. [DOI] [PubMed] [Google Scholar]
- 7.Cingi A, Demirkalem P, Manukyan MN, Tuney D, Yegen Left-sided paraduodenal hernia: Report of a case. Surg Today. 2006;36:651–4. doi: 10.1007/s00595-006-3205-x. [DOI] [PubMed] [Google Scholar]
- 8.Dritsas ER, Ruiz OR, Kennedy GM, Blackford J, Hasl D. Paraduodenal hernia: A report of two cases. Am Surg. 2001;67:733–6. [PubMed] [Google Scholar]
- 9.Blachar A, Federle MP, Dodson SF. Internal hernia: Clinical and imaging findings in 17 patients with emphasis on CT criteria. Radiology. 2001;218:68–74. doi: 10.1148/radiology.218.1.r01ja5368. [DOI] [PubMed] [Google Scholar]
- 10.Uematsu T, Kitamura H, Iwase M, Yamashita K, Ogura H, Nakamuka T, et al. Laparoscopic repair of a paraduodenal hernia. Surg Endosc. 1998;12:50–2. doi: 10.1007/s004649900591. [DOI] [PubMed] [Google Scholar]