Abstract
Sirenomelia also known as the mermaid syndrome, is a rare congenital malformation of uncertain etiology. It is characterized by fusion of the lower limbs and commonly associated with severe urogenital and gastrointestinal malformations. There are approximately 300 cases reported in the literature, 15% of which are associated with twinning, most often monozygotic. The syndrome of caudal regression is thought to be the result of injury to the caudal mesoderm early in gestation.
Keywords: Caudal regression, mermaid syndrome, sirenomelia
INTRODUCTION
Sirenomelia is a rare and fatal congenital anomaly characterized by single fused lower limbs with multiple urogenital and anorectal malformations with an incidence of 0.8-1 case /100000 births, with male to female ratio being 3:1.[1] The sequence was originally described by Rocheus in 1542 and Palfyn in 1953 and named after the mythical Greek sirens. Duhamal in 1961 defined the anomalies of mermaid syndrome and described it as the most severe form of caudal regression syndrome.[2,3] This syndrome has a strong association with maternal diabetes where the relative risk is 1:200 to 1:250 and 22% of fetuses with this anomaly will have diabetic mothers.[4,5] Most of the cases of sirenomelia results in still birth or die within in a day or two due to congenital complications.
CASE REPORT
A 34-week, 1400-g preterm infant of unidentified sex was born to a 23-year-old primigravida mother with no significant past medical history. The infant was delivered by assisted breech vaginal delivery with an APGAR's score of 3 and 5 at 1 and 5 minutes, respectively. On physical examination of the infant showed single umbilical artery with multiple external deformities including a single lower tapering web like lower extremity with no feet and absence of external genitalia and anus. Additionally, Potter's facies i.e., prominent infraorbital folds, small slit like mouth, receding chin, downward curved nose, and low set soft dysplastic ears were seen [Figures 1 and 2]. Radiographic picture revealed single distal limb [Figures 3 and 4]. The infant expired after four hours due to severe respiratory distress. An autopsy was performed which showed severe bilateral lung hypoplasia, absence of the bladder, ureters, and bilateral kidneys. Uterus and vagina were atretic but ovaries and fallopian tubes were normal, rectum and anus were atretic. Death was attributed to pulmonary hypoplasia along with renal anomalies, and a diagnosis of sirenomelia was given.
Figure 1.

Potter's facies i.e., prominent infraorbital folds, small slit-like mouth, receding chin, downward curved nose, and low set soft dysplastic ears including a single lower tapering web like lower extremity with no feet
Figure 2.
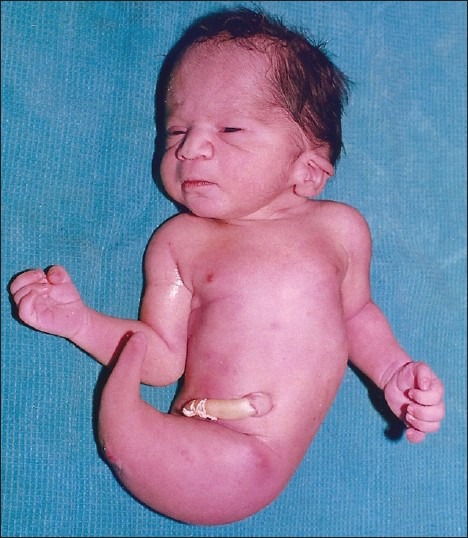
Potter's facies i.e., prominent infraorbital folds, small slit-like mouth, receding chin, downward curved nose, and low set soft dysplastic ears including a single lower tapering web like lower extremity with no feet
Figure 3.

Antero-posterior view showing single femur and tibia
Figure 4.

Lateral view showing single femur and tibia
DISCUSSION
Sirenomelia as a part of caudal regression syndrome has its own pathogenesis which is maternal metabolic derangement in diabetes, but evidences have shown that sirenomelia and caudal regression are two different entities.[6] The etiology of sirenomelia is unclear though it is well known that the embryological injury occurs between 28 and 32 days of life and the site is at the caudal mesoderm. Stevenson et al.[7] explains diversion of blood away from the caudal region of the embryo through the abdominal umbilical artery” vascular steal” has been proposed as the primary mechanism leading to sirenomelia.[8,9,10] Although altered oxidative metabolism from maternal diabetes may cause free oxygen radicals in the developing embryo which may be teratogenic.[11] Recent studies have shown that vascular disruption precedes caudal dysgenesis in the mouse.[12]
In our case report the clinical and anatomical features consistent with sirenomelia apus type as there is only one tibia and one femur. A single large umbilical artery was observed in direct continuation with the abdominal aorta. This type of vascular anomaly is considered a remnant of the vitelline artery complex and is almost always associated with sirenomelia.[13] Currently there is no serum marker to diagnose sirenomelia. Prenatal ultrasonography as early as 13 weeks of pregnancy can detect gross structural anomalies. So if diagnosed early the alternative of termination of pregnancy can be safely advised to the mother. Similarly proper control of blood glucose level in a diabetic mother may prevent the occurrence of sirenomelia.
ACKNOWLEDGMENT
The authors are thankful to Dr. Sanket Makadiya and Dr. Manal Ahmed for their immense help and technical support.
Informed consent was taken from parents for publication.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Reddy KR, Srinivas S, Kumar S, Reddy S, Hariprasad, Irfan GM. Sirenomelia a rare presentation. J Neonat Surg. 2012;1:7. [PMC free article] [PubMed] [Google Scholar]
- 2.Martinez-Frios ML, Garica A, Bermejo E. Cyclopia and sirenomelia in live infant. J Med Genet. 1998;35:263–4. doi: 10.1136/jmg.35.3.263-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duhamel B. From the mermaid to anal imperforation: The syndrome of caudal regression. Arch Dis Child. 1961;36:152–5. doi: 10.1136/adc.36.186.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aslan H, Yanik H, Celikaslan N, Yildirim G, Ceylan Y. Prenatal diagnosis of caudal regression syndrome: A case report. BMC Pregnancy Childbirth. 2001;1:8. doi: 10.1186/1471-2393-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gonzalez-Quintero VH, Tolaymat L, Martin D, Romaguera RL, Rodigeuz MM, Izeqiredo LA. Sonographic diagnostic of caudal regression in the first trimester of pregnancy. J Ultrasound Med. 2002;21:117–8. doi: 10.7863/jum.2002.21.10.1175. [DOI] [PubMed] [Google Scholar]
- 6.Twickler D, Budorick N, Pretorius D, Grafe M. Caudal regression verses sirenomelia. J Ultrasound Med. 1993;12:323–30. doi: 10.7863/jum.1993.12.6.323. [DOI] [PubMed] [Google Scholar]
- 7.Stevenson RE, Jones KL, Phelan MC, Jones MC, Barr M, Jr, Clericuzio C. Vascular steal: The pathogenetic mechanism producing sirenomelia and associated defects of the viscera and soft tissues. Pediatrics. 1986;78:451–7. [PubMed] [Google Scholar]
- 8.Van Keirsblick J, Cannie M, Robrechts C, de Ravel T, Dymarkowski S, Va den Bosch T, et al. First trimester diagnosis of Sirenomelia. Prenat Diagn. 2006;26:684–8. doi: 10.1002/pd.1479. [DOI] [PubMed] [Google Scholar]
- 9.Schiesser M, Holzgreve W, Lapaire O, Willi N, Luthi H, Lopez R, et al. Sirenomelia, the mermaid syndrome-detection in first trimester. Prenat Diagn. 2003;23:493–5. doi: 10.1002/pd.624. [DOI] [PubMed] [Google Scholar]
- 10.Duesterhoeft SM, Ernst LM, Siebert JR, Kapur PR. Five cases of caudal regression with an aberent abdominal umbilical artery: Futher support for a caudal regression-sirenomelia spectrum. Am J Med Genet A. 2007;143A:3175–84. doi: 10.1002/ajmg.a.32028. [DOI] [PubMed] [Google Scholar]
- 11.Kedian YS, Duhan N, Rattan KN, Rawal M. Sirenomelia (mermaid syndrome): A rare anomaly. Afr J Paediatr Surg. 2008;5:105–6. doi: 10.4103/0189-6725.44190. [DOI] [PubMed] [Google Scholar]
- 12.Padamanabhan R, Naruse I, Shiota K. Caudal regression in staged human embryos: Carnegie stages 16-23. Am J Med Genet. 1999;87:115–27. doi: 10.1002/(sici)1096-8628(19991119)87:2<115::aid-ajmg2>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 13.Das BB, Rajegowda BK, Bainbridge R, Giampietro PF. Caudal regression syndrome verses sirenomelia: A case report. J Perinatol. 2002;22:168–70. doi: 10.1038/sj.jp.7210598. [DOI] [PubMed] [Google Scholar]


