Abstract
Neurothekeomas are rare benign neoplasms, typically occurring in young patients with a remarkable predilection for the female population. Patients usually present with a small nodule in different anatomical sites, commonly involving the face and the upper limb. We report a case of a three-year-old boy, who presented with a nontender nodule on the left thumb. Surgical biopsy and immunostaining confirmed the diagnosis as myxoid neurothekeoma. The rarity of this unusual skin tumor in a toddler prompted the following report.
Keywords: Neurothekeoma, soft tissue tumor, toddler
INTRODUCTION
Nerve sheath myxoma (neurothekeoma) is an uncommon benign soft tissue tumor of the peripheral nerves with fairly distinctive histological features. It is commonly located on the upper extremities or the head and the neck.[1] Histologic variants of neurothekeoma include myxoid, cellular, and mixed tumors. A recent immunohistochemical pattern enables a differentiation between myxoid neurothekeoma, melanocytic tumors, and nervous system tumors.[2] We report a rare case of myxoid neurothekeoma in a three-year-old child.
CASE REPORT
A three-year-old boy presented with a nontender, left thumb swelling of four-week duration, without any history of trauma. Fine needle aspiration cytology of the mass revealed a few plump-to-oval spindle-shaped cells in a myxoid background. Subsequently, the lesion was surgically excised. Gross examination of the submitted specimen revealed a firm, elastic, tan-colored smooth nodule, measuring 10 × 8 × 6 mm with a solid homogeneous gray cut surface [Figure 1]. Histopathologic examination revealed a nonencapsulated dermal tumor, composed of multiple, closely situated medium-sized nodules with scattered spindle-shaped cells in a myxoid-rich stroma [Figure 2]. The tumor exhibited strong positivity for S-100 immunohistochemical stain [Figure 3], and focal positivity for neuron-specific enolase (NSE). Based on the histopathologic and immunohistochemical results, the case was diagnosed as nerve sheath myxoma of classical type. The patient was followed up for 10 months with no reports of recurrence.
Figure 1.

Neurothekeoma: Cut section shows solid homogeneous soft, yellowish gray tissue
Figure 2.
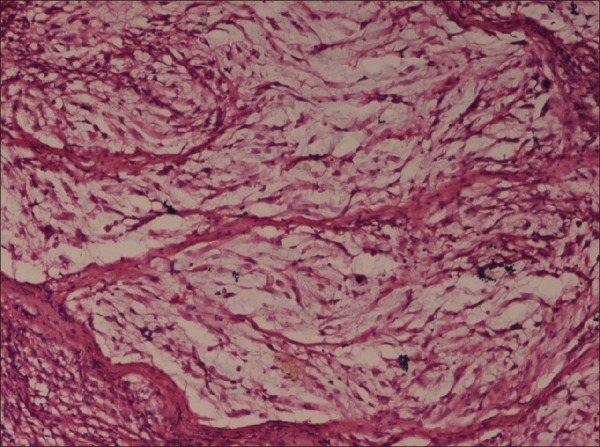
Neurothekeoma: Tissue section shows a nonencapsulated dermal tumor, composed of multiple, medium-sized nodules composed of few oval-to-plump spindle cells, in a myxoid-rich stroma (H and E, ×10)
Figure 3.
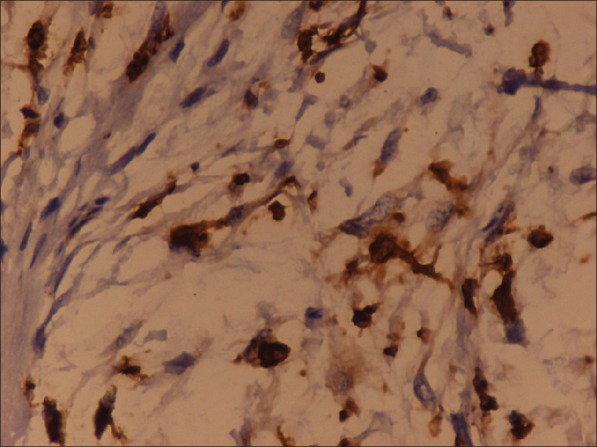
Neurothekeoma: The tumor cells show strong positivity for S-100 immunohistochemical stain
DISCUSSION
Neurothekeomas commonly present as small solitary erythematous nodules on the face and the upper limb. However, other anatomic sites have been reported in the literature, such as oral cavity, cauda equina, lower limb, shoulder, and neck.[3] Clinically, neurothekeomas are slow-growing asymptomatic lesions. They are commonly dermal, but mucosal and submucosal lesions have been described.[3] It is a tumor of the adolescent and young adult, with a female predilection, but is extremely rare in infancy.[4]
Neurothekeoma is a rare benign tumor of the nerve sheath, with a distinct histological presentation. It was described initially by Hakin and Reed, in 1969, as nerve sheath myxoma but the term ’neurothekeoma’ was given by Gallager and Helwing.[5]
There are three histologic variants of neurothekeoma: Myxoid (classical or hypocellular), cellular, and mixed type.[6] The myxoid type is characterized by a high degree of myxomatous changes, low cellularity with scattered spindle cells, and is well circumscribed. There may also be multinucleated giant cells and the lesions characteristically stain positively for S-100, collagen type IV, and nerve growth factor receptor but are negative for epithelial membrane antigen or markers of histiocytic differentiation. In contrast, the cellular types of neurothekeoma are not encapsulated and the mixed type shows areas of varied cellularity with focal myxoid regions. Our case is a typical example of a myxoid type of neurothekeoma.
The cell of origin of neurothekeoma is controversial with theories proposing a proliferation of Schwann cells or other perineural cells.[7] Dual immunoreactivity for NSE and S-100 protein in a myxoid background supports Schwann cell origin, whereas the absence of S-100 protein and positive epithelial membrane antigen in the cellular type suggests perineural cell lineage.[7] Fetsch, et al.[8] postulated a tendency of neurothekeoma to recruit histiocytic cells and to differentiate into myofibroblasts. Smooth muscle actin (SMA) positivity suggests some similarity to the epithelioid variant of leiomyoma or myofibroblastic proliferations.[9] Glial fibrillary acidic protein (GFAP) positivity is rare in neurothekeoma; however, its positivity further supports a peripheral nerve sheath origin, as occasional peripheral nerve sheath tumors may coexpress GFAP and S-100.[10]
Nerve sheath myxoma and neurothekeoma are recently identified as different entities in gene expression profiling, although they might share some morphologic similarities. Gene expression array data strongly supports that nerve sheath myxomas are of peripheral nerve sheath origin and are distinct neoplasms from neurothekeomas. Furthermore, data shows many similarities in gene expression between neurothekeomas and cellular fibrous histiocytomas, supporting recent arguments that these entities may in fact be related.[2,11]
There is an overlapping feature with other neural tissue tumors such as schwannoma, nerve sheath myxoma, and neurofibroma, leading to difficulties in diagnosis. Differential diagnosis of dermal nodule in infancy and young adulthood should include fibrous tumors, histiocytic tumors, lymphocytic tumors, melanocytic tumors, and neural tumors.[12] Complete excision is the mainstay of treatment for neurothekeoma. Recurrence of the tumor maybe due to incomplete removal of the original lesion.[1] Our patient was followed up for 10 months with no reports of recurrence.
CONCLUSION
Neurothekeoma is extremely rare in a toddler. Myxoid neurothekeoma may present as a dermal lesion in the finger. Reporting such a case will increase awareness about this disease, as it should be included in the differential diagnosis of dermal lesions in young children.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Papadopoulos EJ, Cohen PR, Hebert AA. Neurothekeoma: Report of case in an infant with a review of literature. J Am Acad Dermatol. 2004;50:129–34. doi: 10.1016/s0190-9622(03)00886-7. [DOI] [PubMed] [Google Scholar]
- 2.Sachiv S, Xinmin L, Scott B, Sarah MD. Differential gene expression profiles of neurothekeomas and nerve sheath myxomas by microarray analysis. Modern Pathol. 2011;24:343–54. doi: 10.1038/modpathol.2010.203. [DOI] [PubMed] [Google Scholar]
- 3.Hurwitz S. Clinical pediatric dermatology: A textbook of skin disorders of childhood and adolescence. 2nd ed. Philadelphia: Saunders; 1993. Cutaneous tumors in childhood; pp. 198–241. [Google Scholar]
- 4.Al-Buainain H, Pal K, El Shafie H, Mitra DK, Shawarby MA. Myxoid neurothekeoma: A rare soft tissue tumor of hand in a 5 month old infant. Indian J Dermatol. 2009;54:59–61. doi: 10.4103/0019-5154.48990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gallager RL, Helwig EB. Neurothekeoma a benign cutaneous tumour of neural origin. Am J Clin Pathol. 1980;74:759–64. doi: 10.1093/ajcp/74.6.759. [DOI] [PubMed] [Google Scholar]
- 6.Bhaskar A, Kanvinde R. Neurothekeoma of the hand. J Hand Surg Br. 1999;24:631–3. doi: 10.1054/jhsb.1999.0249. [DOI] [PubMed] [Google Scholar]
- 7.Schortinghuis J, Hille JJ, Singh S. Intraoral myxoid nerve sheath tumour. Oral Dis. 2001;7:196–9. [PubMed] [Google Scholar]
- 8.Fetsch JF, Laskin WB, Hallman JR, Lupton GP, Miettinen M. Neurothekeoma: An analysis of 178 tumors with detailed immunohistochemical data and long-term patient follow-up information. Am J Surg Pathol. 2007;31:1103–4. doi: 10.1097/PAS.0b013e31802d96af. [DOI] [PubMed] [Google Scholar]
- 9.Calonje E, Wilson-Jones E, Smith NP, Fletcher CD. Cellular ’neurothekeoma’: An epithelioid variant of pilar leiomyoma. Morphological and immunohistochemical analysis of a series. Histopathology. 1992;20:397–404. doi: 10.1111/j.1365-2559.1992.tb01009.x. [DOI] [PubMed] [Google Scholar]
- 10.Katsourakis M, Kapranos N, Papanicolaou SI, Patrikiou A. Nerve-sheath myxoma (neurothekeoma) of the oral cavity: A case report and review of the literature. J Oral Maxillofac Surg. 1996;54:904–6. doi: 10.1016/s0278-2391(96)90545-5. [DOI] [PubMed] [Google Scholar]
- 11.Barnhill RL, Mihm MC., Jr Cellular neurothekeoma: A distinctive variant of neurothekeoma mimicking nevomelanocytic tumors. Am J Surg Pathol. 1990;14:113–20. doi: 10.1097/00000478-199002000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Yamashaita N, Minami S, Yu M. Dermal nerve-sheath myxoma. J Dermatol. 1990;17:564–8. doi: 10.1111/j.1346-8138.1990.tb01696.x. [DOI] [PubMed] [Google Scholar]


