Abstract
Lichen planus (LP) is one of the most distinct mucocutaneous diseases. It is common with the middle aged and elderly population but has rarely been described in children. Incidences of oral LP in children is most commonly reported amongst Asians. We present a 10-year-old Indian girl with the documented clinical aspects and histopathological studies.
Background
Lichen planus (LP) is a common chronic inflammatory disease of skin and mucous membranes.1 British physician Erasmus Wilson first described the condition LP in 1869 and reported 6% of prevalence in the general population. Lichens are primitive plants composed of symbiotic algae and fungi. The term planus is Latin, for flat. Wickham in 1895 described the characteristic appearance of white straie that develop atop the flat surfaced papules. LP is predominantly a disease of the middle aged and the elderly population.2 Oral LP is rare in childhood, and few reports on this subject have appeared in the literature.
Though the clinical features of oral LP are similar in adults and children, yet the prognosis seems to be more favourable in children.3 4 Up to six clinical appearances of oral LP have been described including reticular, atrophic, plaque-like, popular, erosive and bullous types.5 The characteristic sites involved are the buccal mucosa dorsum of the tongue and less frequently the gingival.
The aetiology of the condition remains obscure, but it appears to be complex and multi-factorial. In some patients it may be idiopathic but in most of the cases the condition is exacerbated or even provoked by a variety of drugs and dental materials.1 2 Viruses, genetic factors and lifestyle also play a significant aetiological role. An inborn error of metabolism has been sited, such as glucose-6-phosphate dehydrogenase deficiency, and long lasting abnormal glucose metabolism with glucose intolerance. An association between oral LP and hepatitis C virus infection has been reported in the literature.5 More recent studies suggest that at least 50% of the cases reported, had familial histories of LP. It is unusual for children to use those drugs known to be associated with lichenoid reactions. There are reports of childhood lichenoid eruptions following the administration of hepatitis B vaccine.6
Whatever the aetiology is, the primary event starts with the damage of the basal layer of the epithelium. An unidentified allergen may have an originating effect on this immunological-based process. This mechanism of basal cell damage is related to a cell-mediated immune response involving Langerhan's cells, T-lymphocytes and macrophages. Histochemical studies have identified a T-cell origin with CD4 and CD8 subsets in oral LP.
There is little literature on oral LP occurring in childhood.6 This paper reports a case of oral LP in childhood.
Case presentation
A 10-year-old girl was referred to the department of paedodontics, with a burning sensation in the mouth for the past 1 month while consuming spicy food and bilateral pigmentation on the inner part of her cheek. Medical and family history was not significant.
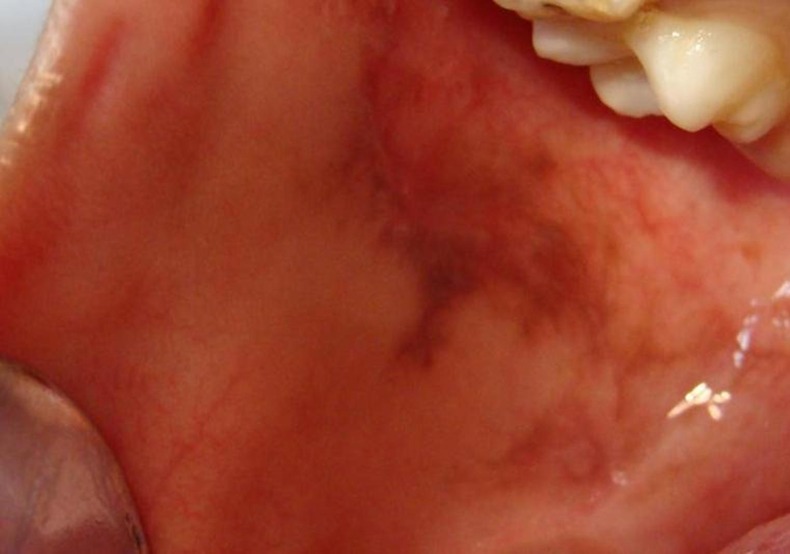
On examination she appeared to be a healthy 12-year-old girl with no skin lesion. On intraoral examination a greyish brown patch with white striae were observed bilaterally in the posterior buccal mucosa extending into the retromolar fossae (figures 1 and 2). These lesions were non-tender on palpation. No other mucosal or skin surfaces showed lesional changes. A provisional diagnosis of reticular LP was made based on clinical examination. The patient was referred to the dermatologist for ruling out cutaneous association. The patient is currently on topical application of 0.05% Tretinoin cream and under weekly review for the first month. Based on the prognosis a decision will be made after a month, whether to start the patient on systemic steroid therapy.
Figure 1.

Left buccal mucosa.
Figure 2.
Right buccal mucosa.
Investigations
Routine haematology, biochemistry and immunology screen were normal except, haemoglobin which was 10.2 g (normal range 12–14%). Histologically, microscopic features showed hyperorthokeratosis/hyperparakeratosis, subepithelially and liquefactive degeneration of the basal cell zone, basal cell degeneration and subepithelial band of lymphocytes. The rete ridges having a saw tooth shape and fibrin deposition with a characteristic fibrillar pattern extending as irregular strands into the superficial lamina propria confirmed the diagnosis of the lesion to be LP (figure 3).
Figure 3.
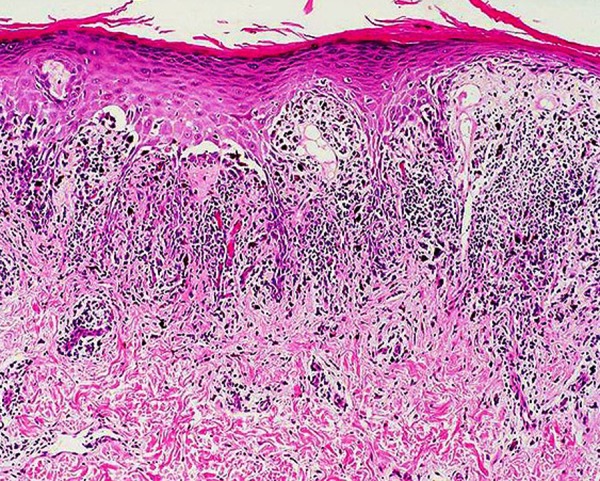
Histopathological picture.
Treatment
The patient is currently on topical application of 0.05% Tretinoin cream and under weekly review for the first month. Based on the prognosis a decision will be made after a month, whether to start the patient on systemic steroid therapy.
Discussion
Oral LP is rare in childhood and only a few reports on this subject have appeared in the literature.5–12 Cutaneous LP in childhood is an uncommonly encountered dermatosis5 8 10 11 and is extremely rare in infancy.12 Studies of children with mucocutaneous LP have still shown a very low incidence of oral involvement.4 8 9 Familial LP has been reported as being uncommon.5 10 13 Childhood familial LP is said to occur at an early age and with greater severity.10 It has been documented that childhood LP is more common in the tropics9 and that children of Asian origin may be prone to the condition.6 10 14
Usually LP tends to occur most commonly in women. Sharma et al15 found the male to female ratio as 2:1. The clinical presentation of oral LP are diverse, ranging from the classical white bilaterally symmetrical reticular network found characteristically on the buccal mucosae, to widespread and debilitating ulcerative lesions. Usually LP lesions are asymptomatic but a burning sensation may be associated with few cases.1 The clinical presentation and site predilection in our case are consistent with the classical description of LP.
While oral LP is considered rare in childhood and the presence of often asymptomatic, oral lesions should alert the clinician to such a diagnosis. This condition should be considered in the differential diagnosis of other white lesions of the oral mucosa. Such a diagnosis followed by early treatment will help the dental clinician to avoid the complications arising due to this disorder, thereby presenting the patients with a better quality of life.
Learning points.
Oral lichen planus (LP) is rare in childhood.
Oral LP lesions are asymptomatic but a burning sensation may be associated.
LP is not a life-threatening disease, but, is known to be an intense pruritic disorder. It may cause irreversible scarring, which may not be acceptable cosmetically. This, then results in a low quality of life.
Early treatment will help the dentist to avoid the complications arising due to this disorder, thereby presenting the patients with a better quality of life.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Patel S, Yeoman CM, Murphy R. Oral lichen planus in childhood: a report of three cases. Int J Paediatr Dent 2005;2013:118–22 [DOI] [PubMed] [Google Scholar]
- 2.Silverman S, Jr, Griffith M. Studies on oral lichen planus II. Follow-up on 200 patients, clinical characteristics, and associated malignancy. Oral Surg Oral Med Oral Pathol 1974;2013:705–10 [DOI] [PubMed] [Google Scholar]
- 3.Moliaoglu N. Oral lichen planus: a review. Br J Oral Maxillofac Surg 2000;2013:370–7 [DOI] [PubMed] [Google Scholar]
- 4.Laeijendecker R, Van Joost T, Tank B, et al. Oral lichen planus in childhood. Paediatr Dermatol 2005;2013:299–304 [DOI] [PubMed] [Google Scholar]
- 5.Scully C, Almeida OPD, Welbury R. Oral lichen planus in childhood. Br J Dermatol 1994;2013:131–3 [DOI] [PubMed] [Google Scholar]
- 6.Alam F, Hamburger J. Oral mucosal lichen planus in children. Int J Pediatr Dent 2001;2013:209–14 [DOI] [PubMed] [Google Scholar]
- 7.Cottoni F, Ena P, Tedde G, et al. Lichen planus in children: a case report. Pediatr Dermatol 1993;2013:132–5 [DOI] [PubMed] [Google Scholar]
- 8.Kanwar AJ, Handa S, Gosh S, et al. Lichen planus in childhood: a report of 17 pateints. Paediatr Dermatol 1991;2013:288–91 [DOI] [PubMed] [Google Scholar]
- 9.Kumar V, Garg BR, Baruah MC, et al. Childhood lichen planus. J Dermatol 1993;2013:175–7 [DOI] [PubMed] [Google Scholar]
- 10.Milligan A, Graham-Brown RAC. Lichen planus in children: a review of 6 cases. Clin Exp Dermatol 1990;2013:340–2 [DOI] [PubMed] [Google Scholar]
- 11.Howard R, Tsuchiya A. Adult skin disease in the pediatric patient. Dermatol Clin 1998;2013:593–608 [DOI] [PubMed] [Google Scholar]
- 12.Kanwar AJ, Kaur S, Rajagopaln M, et al. Lichen planus in an 8 month old. Pediatr Dermatol 1989;2013:358–9 [DOI] [PubMed] [Google Scholar]
- 13.Mahood JM. Familial lichen planus. A report of nine cases from four families with a brief review of the literature. Arch Dermatol 1983;2013:292–4 [DOI] [PubMed] [Google Scholar]
- 14.Handa S, Sahoo B. Childhood lichen planus: a study of 87 cases. Int J Dermatol 2002;2013:423–7 [DOI] [PubMed] [Google Scholar]
- 15.Sharma R, Maheshwari V. Childhood lichen planus: a report of fifty cases. Pediatr Dermatol 1999;2013:345–8 [DOI] [PubMed] [Google Scholar]


