Abstract
Background: More than half of myocardial infracted (MI) patients have no conventional risk factors. Regarding the belief that opium addiction has a protective effect on heart diseases, addiction prevalence has unfortunately increased in recent years. This study was conducted to investigate the effect of opium addiction on patients with acute myocardial infarction.
Methods: This case-control study was performed on 118 patients with acute myocardial infarction admitted to CCU ward (case group), and 118 patients with no history of MI to other wards (control group) of Shahid Beheshti Hospital in Babol, Iran. Opium addiction conventional risk factors were evaluated for both groups, and the data were analyzed using chi-square test and logistic regression model was used to adjust the conventional risk factor effects. Moreover, demographic variables as well as the extent of MI (extensive or non-extensive), and infarction type (ST-elevated or non-ST elevated) also were evaluated.
Results: Sixty-seven patients in MI and 6 subjects in control group had a history of opium consumption (p<0.0001, OR=24.5). Blood pressure, hyperlipidemia, and smoking showed a significant difference between the two groups (p<0.05), whereas, no significant difference was observed for diabetes and family history. The results of adjusted model report a significant effect of opium consumption with the development of MI (OR=26.3). No significant difference was found in terms of infarction type and the extent between the addicts and non addicts in MI group.
Conclusion: The results show that opium addiction is a strong risk factor for myocardial infarction.
Key Words: Ischemic heart diseases, Myocardial infarction, Opium addiction, Conventional risk factor
Ischemic heart disease (IHD) is the most common cause of disability and mortality in underdeveloped countries and the main leading cause of morbidity in the developed countries, exerting the most financial costs compared to other diseases. Myocardial infarction (MI) is one of the most prevalent diagnoses in hospitalized patients causing extensive financial and life damages to human societies (1). Hence, the identification of the associated risk factors is a matter of high importance for diagnosis, treatment and prognosis of the disease. Myocardial infarction is developed by the complete blockage of coronary arteries narrowed by atherosclerotic plaque, therefore, the factors leading to the coronary heart disease (CHD) are considered as MI-causing risk factors (2,3). Hypertension, hyperlipidemia, diabetes and smoking have been investigated and confirmed by many studies as four conventional risk factors associated to CHD (4). However, findings of some studies showed that almost more than half of the patients with CHD have none of these conventional risk factors, and other parameters such as genetic predisposition, inflammatory, hormonal and many other unknown factors can be discussed as IHD-associated risk factors (5-8). In 1975, endogenous ligands called opioid peptides were identified for opioid receptors (9).
Studies performed on these ligands showed that opioid peptides play a significant role in some physiological functions and cardiovascular pathological conditions such as heart development, bradycardia, tachycardia, myocardial hypertrophy, hypertension, hypotension, peripheral vasodilatation, heart failure and ischemic preconditioning (IPC), all of which are dependent to dose as well as the type of the stimulated receptor in the different regions (-). Cardiovascular regulatory effects of endogenous opioids originated from central nervous system through the facilitation of neurotransmitter regulatory effect. Besides, recent studies have demonstrated that opioid peptides, arising from the myocardium itself, play a major role in the local regulation of cardiovascular functions (10).
Drug addiction is one of the fundamental problems of any society, including Iran. It has been estimated that drug addiction has become three-fold in this country during the past 20 years. One reason behind the high incidence of addiction in Iran is the people’s erroneous belief about opium effectiveness on blood pressure and diabetes and prevention of cardiovascular events (14).
Therefore, considering that more than half of the patients with CHD have none of the conventional risk factors, and regarding relationships between opioid peptides and some cardiovascular pathophysiological conditions, the present study was performed to determine the association between addiction and myocardial infarction.
Methods
This case-control study was performed on 118 patients with acute myocardial infarction admitted to CCU ward of Babol Shahid Beheshti Therapeutic Center less than 24 hours, as the case group, and 118 patients with no history of MI admitted to other wards of the same hospital as the control group. The sampling method was a systematic random in both groups. The inclusion criteria included the recent acute myocardial infarction and over 20 years of age in the case group, and no history of IHD in the control group. For MI diagnosis, three criteria (clinical, increased cardiac enzyme levels and ECG changes) were used, and infarction was identified if two of the three mentioned parameters were abnormal. Infarction type (ST-elevated or non-ST elevated) and lesion extent (extensive or non extensive) were assessed in both groups. All patients were asked in terms of presence or absence of addiction (at least one year of oral or smoked opium addiction). They were also examined for the presence or absence of IHD conventional risk factors (hypertension, hyperlipidemia, diabetes and smoking) in both groups. Data were analyzed using t-test and chi-square test between the two groups when appropriate. For adjustment, the confounding effect of age, gender, family history and conventional risk factors logistic regression model was used. In addition, infarction type (ST-elevated or non-ST-elevated) and lesion extent (extensive or non extensive) were assessed between the addicts and non-addicts in the case group.
Results
The mean age of patients in case and control groups was 61.4±12.8 and 47.9±5.19 years, respectively. Sixty-nine percent of patients in case group and 59.3% of patients in the control group were males. Sixty-seven (56.8%) of patients in case group and 6 (5.1%) of patients in the control group were addicts (p=0.001).
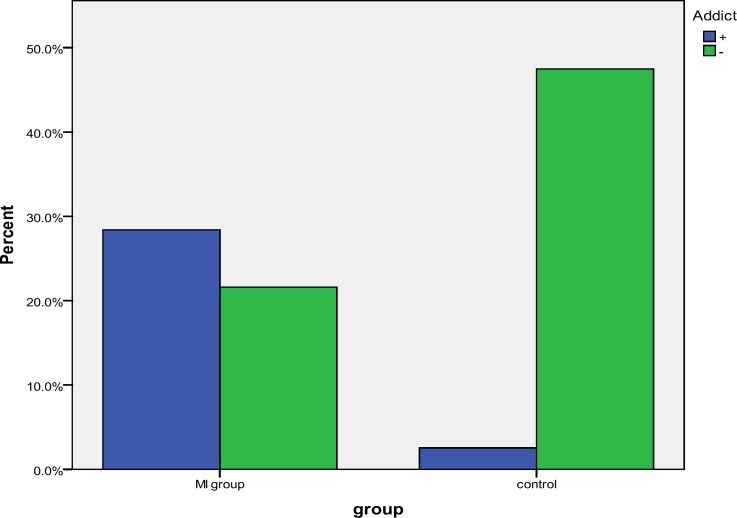
Gender frequency was reported 68.6% males and 31.4% females in case group, and 59.3% males and 40.7% females in the control group. Investigation on both groups indicated that 67 (56.8%) patients in the case group and 6 (5.1%) subjects in the control had a history of opium consumption (figure 1). The frequency distribution of conventional variables in both groups is presented in table 1.The results of crude data analysis using chi square test displayed a significant difference in opium addiction between the two groups (OR=24.5, 95%CI, 9.9−60.2, p=0.001). The relations of other conventional risk factors are shown in table 2.
Figure 1.
Opium consumption comparison between two groups (p≤0.001)
Table 1.
Frequency distribution of conventional risk factors in both groups
| Conventional risk factors |
(%)
Frequency
|
|
|---|---|---|
| Case | Control | |
| Hypertension | 25.4 | 11.9 |
| Diabetes Mellitus | 22.9 | 16.1 |
| Hyperlipidemia | 26.3 | 11.9 |
| Smoking | 39.8 | 11 |
Table 2.
Crude data analysis in association of conventional risk factors
| Odds Ratio | CI 95% | P-value | |
|---|---|---|---|
| Hypertension | 2.5 | 1.5-2 | 0.007 |
| Diabetes Mellitus | 1.5 | 0.8-2.9 | 0.18 |
| Hyperlipidemia | 2.6 | 1.3-5.2 | 0.005 |
| Smoking | 5.3 | 2.5-10.6 | 0.001 ≤ |
The results of adjusted model with logistic regression determined that age, gender, smoking and opium addiction have significant relationship with MI occurrence. These results have been described in table 3. With regard to the infarction type in the MI group, among 118 patients, 83 (70.3%) cases were identified with ST-elevated MI, 32 (27.1%) patients with non-ST-elevated MI, and 3 (2.6%) cases were uncertain.
Table 3.
Adjusted data analysis between two groups
| Odds Ratio | CI 95% | P-value | |
|---|---|---|---|
| Opium addiction | 26.3 | 7.5-92.4 | 0.001≤ |
| Smoking | 4.2 | 1.4-12.1 | 0.008 |
| Gender | 13.3 | 4.2-40.8 | 0.001≤ |
| Age | 0.9 | 0.8-0.9 | 0.001≤ |
In ST-elevated MI patients, 44 (53%) cases and in non ST-elevated MI subjects, 21 (6.65%) were opium-addicted (p=0.221, odds ratio=0.59). In terms of infarction extent, 21 (17.8%) patients were found with extensive infarction, among whom 10 (6.5%) cases were addicted, and 93 (78.8%) patients were observed with non-extensive infarction, among whom 54 (58.1%) subjects were addicts, and 4 patients were uncertain for the extent of infarction (p=0.348, OR=0.6).
Discussion
In this study, we found a significant association between opium addiction and MI. However, there was no association between opium addiction and extent of MI. This finding is consistent with the results of earlier studies (14). In a study of 556 patients with MI, opium addiction was found in 19% of the patients versus 2.8% in the general population (14). In another study of patients with coronary artery diseases confirmed by angiography, opium addiction was associated with CAD development in the male patients (15). In another angiographic study of 2405 patients, the prevalence of vascular involvement in addicts was higher than in non-addict individuals (16).
In contrast to the results of our study, Najafi et al, on 275 patients undergoing GABG surgery showed that there was no difference between the addict and non-addict with regard to postoperative quality of life, but only the females and those with history of previous MI were remarkably affected (17). Similarly Sadeghian et al, also found no significant differences between the addicts and non-addicts in terms of preoperative risk factors (18). The results of the present study demonstrated a significant relationship between acute myocardial infarction and opium addiction. Several interventional studies on animals have shown the effectiveness of myocardial opioid receptor stimulation by endogenous opioids such as enkephalin on the regulation of cardiac function and their important role in a number of physiological and pathological cardiac events such as hypertrophy, aging, evolution, hypertension, ischemic preconditioning and heart failure (10).
Signal transduction mechanisms by these receptors may lead to such diverse processes and are not precisely known and require further investigation. Another study showed that long-term consumption of low-to-moderate dose of opioids in reducing chronic pain indicated no complications or slight complications by therapeutic dose of opioids (19). Although they did not examine long-term consumption of high-dose opioids (abuse and addiction). However, studies conducted in the past exhibited complications such as tolerance, abuse, addiction, hyperalgesia, hormonal effects and immune suppression due to the effect of prescribed high therapeutic dose of opioids (20). In another study by Harris in 2008, the complications of long-term opioid use were evaluated on body systems, and it was found that these complications include delirium, drowsiness, headaches and seizures in the neurological system, respiratory suppression, bradycardia, hypotension and cardiac arrhythmias in cardiorespiratory system, nausea, vomiting, constipation, dry mouth and gastroesophagial reflux in digestive system, decreased renal function, peripheral edema, and urinary retention in urologic system, hypogonadism, sexual dysfunction and osteoporosis in endocrine system, itchy skin and diaphoresis and eventually immune suppression (21).
He also showed that these complications are dose dependent, and can be moderated through changing the administration mode and using opioid antagonists. A study on MI developed rats showed that simultaneous administration of opioids and GSK ß (Glycogen Synthase Kinase ß) inhibitor exactly before reperfusion can contribute to reduce infarct region (22). One of the main reasons of the individuals' false belief that consumption of opium and its derivatives can help prevent the incidence of IHD in middle age is the supposition that opium use may reduce plasma lipid levels. Fatemi et al, in two groups, the addicts and non addicts showed no significant relationship regarding triglycerides, LDL and HDL levels between them, and only plasma total cholesterol level showed remarkable difference, which was on average, 20 mg/dl lower in the addict group (23). Such a difference cannot justify opium influence on plasma lipid profile and its effect on prevention of IHD development. Moreover, in a study by Maccari et al. on the plasma level of triglycerides and cholesterol, the levels of total cholesterol and HDL were significantly lower while the triglyceride level was remarkably higher among the heroin addicts (24).
In Sadr Bafghi et al, an investigation in Yazd on 556 male patients with MIshowed the prevalence of opium addiction reported to be 19 percent; regarding the opium addiction prevalence in general population (2-2.8%), the authors considered a strong probability for opium addiction as a risk factor. In addition, conventional risk factors in addicts and non-addicts were assessed with and without data matching and no remarkable difference were seen (14). In evaluating the odds ratios of various risk factors, it has been realized that diabetes mellitus in females and opium addiction in males are the major influential factors on probability of CAD development a finding like similar that our results (15,16).
Therefore, considering such pieces of evidence, it can be stated that long-term use of opioid increases the susceptibility to IHD and can be considered as a risk factor for acute myocardial infarction.
This study had some limitations .The mean age in case group was higher than control group and using opium is more frequent in older population. It was possible that a number of patients with noncardiac diseases did not report their state of addiction and the real value of prevalence rate might be higher than that reported in this study. We have also not provided data for the duration of opium addiction that may be another limitation of our study.
It was possible that some patients started opium consumption after development of coronary artery disease to suppress angina symptom and so opium addiction might be a consequence of coronary artery disease development but not a risk factor. However, the contributive role of age, and history of coronary diseases have been controlled by regression analysis.
In conclusion, based on our results, it can be concluded that unlike the population erroneous belief, opioid consumption not only prevent cardiovascular disease, but also is the likely risk factor itself. However, the type and extent of the lesion appear not to be affected by opioid consumption. Nonetheless, long-term use of opioids along with other conventional risk factors can augment the incidence of acute myocardial infarction.
Acknowledgments
The authors wish to express their gratitude to Dr.Heidari for his utmost assistance and the Nursing staff of CCU Ward of Shahid Beheshti Hospital of Babol University of Medical Sciences.
Funding: This project was supported by Vice Chancellory for Reaserch of Babol University of Medical Sciences(No: 65483) and this was an MD thesis of Fatemeh Farshidi (No: 253).
Conflict of Interest: None declared.
References
- 1.Kasper LD, Fauci A, Braunwald E. Harrison's principle of internal medicine. 17 ed. newyork: Mac Grow-Hill ; 2008. [Google Scholar]
- 2.Bannet J, Freed P. Cecil text book of medicine. 22 ed. Philadelphia: WB Saunders; 2007. [Google Scholar]
- 3.Zipes Douglas P, Libby P, Bonow R, Braunwald E. Braunwald's heart disease: a text book of cardiovascular medicine. 8 ed. Philadelphia: WB Saunders; 2008. [Google Scholar]
- 4.Khot UN, Khot MB, Bajzer CT, et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003;290:898–904. doi: 10.1001/jama.290.7.898. [DOI] [PubMed] [Google Scholar]
- 5.Futterman LG, Lemberg L. Fifty percent of patients with coronary artery disease do not have any of the conventional risk factors. Am J Crit Care. 1998;7:240–4. [PubMed] [Google Scholar]
- 6.Tymchuk CN, Hartiala J, Patel PI, Mehrabian M, Allayee H. Nonconventional genetic risk factors for cardiovascular disease. Curr Atheroscler Rep. 2006;8:184–92. doi: 10.1007/s11883-006-0072-2. [DOI] [PubMed] [Google Scholar]
- 7.Sethi AA, Sampson M, Warnick R, et al. High pre-beta1 HDL concentrations and low lecithin: cholesterol acyltransferase activities are strong positive risk markers for ischemic heart disease and independent of HDL-cholesterol. Clin Chem. 2010;56:1128–37. doi: 10.1373/clinchem.2009.139931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Niccoli G, Iacoviello L, Cianflone D, Crea F. Coronary risk factors: new perspectives. Int J Epidemiol. 2001;30:S41–7. doi: 10.1093/ije/30.suppl_1.s41. [DOI] [PubMed] [Google Scholar]
- 9.Kosterlitz H, Hughes J. Some thoughts on the significance of enkephalin, the endogenous ligand. Life Sci. 1975;17:91–6. doi: 10.1016/0024-3205(75)90243-x. [DOI] [PubMed] [Google Scholar]
- 10.Van den Brink OW, Delbridge LM, Rosenfeldt FL, et al. Endogenous cardiac opioids: enkephalins in adaptation and protection of the heart. Heart Lung Circ. 2003;12:178–87. doi: 10.1046/j.1444-2892.2003.00240.x. [DOI] [PubMed] [Google Scholar]
- 11.Weil J, Eschenhagen T, Fleige G, et al. Localization of preproenkephalin mRNA in rat heart: selective gene expression in left ventricular myocardium. Am J Physiol. 1998;275:378–84. doi: 10.1152/ajpheart.1998.275.2.H378. [DOI] [PubMed] [Google Scholar]
- 12.Dumont M, Ouellette M, Brakier-Gingras L, Lemaire S. Circadian regulation of the biosynthesis of cardiac Met-enkephalin and precursors in normotensive and spontaneously hypertensive rats. Life Sci. 1991;48:1895–902. doi: 10.1016/0024-3205(91)90221-v. [DOI] [PubMed] [Google Scholar]
- 13.Lowe H. Role of endogenous opioids in heart failure. Z Cardiol. 1991;80:47–51. [PubMed] [Google Scholar]
- 14.SadrBafghi SM, Rafiei M, Bahadorzadeh L, et al. Is opium addiction a risk factor for acute myocardial infarction? Acta Med Iran. 2005;43:218–22. [Google Scholar]
- 15.Sadeghian S, Graili P, Salarifar M, et al. Opium consumption in men and diabetes mellitus in women are the most important risk factors of premature coronary artery disease in Iran. Int J Cardiol. 2010;141:116–8. doi: 10.1016/j.ijcard.2008.11.063. [DOI] [PubMed] [Google Scholar]
- 16.Sadeghian S, Darvish S, Davoodi G, et al. The association of opium with coronary artery disease. Eur J Cardiovasc Prev Rehabil. 2007;14:715–7. doi: 10.1097/HJR.0b013e328045c4e9. [DOI] [PubMed] [Google Scholar]
- 17.Najafi M, Sheikhvatan M, Montazeri A, et al. Quality of life in opium-addicted patients with coronary artery disease as measured with WHOQOL-BREF. Int J Soc Psychiatry. 2009;55:247–56. doi: 10.1177/0020764008093600. [DOI] [PubMed] [Google Scholar]
- 18.Sadeghian S, Karimi A, Dowlatshahi S, et al. The association of opium dependence and postoperative complications following coronary artery bypass graft surgery: a propensity-matched study. J Opioid Manag. 2009;5:365–72. doi: 10.5055/jom.2009.0036. [DOI] [PubMed] [Google Scholar]
- 19.Manchikanti L, Manchikanti KN, Pampati V, et al. Prevalence of side effects of prolonged low or moderate dose opioid therapy with concomitant benzodiazepine and/or antidepressant therapy in chronic non-cancer pain. Pain Physician. 2009;12:259–67. [PubMed] [Google Scholar]
- 20.Ballantyne J, Mao J. Opioid therapy for chronic pain. N Engl J Med. 2003;349:1943–53. doi: 10.1056/NEJMra025411. [DOI] [PubMed] [Google Scholar]
- 21.Harris JD. Management of expected and unexpected opiod-related side effects. Clin JPain. 2008;24:S8–S13. doi: 10.1097/AJP.0b013e31816b58eb. [DOI] [PubMed] [Google Scholar]
- 22.Gross ER, Hsu AK, Gross GJ. Opioid-induced cardioprotection occurs via glycogen synthase kinase beta inhibition during reperfusion in intact rat hearts. Circ Res. 2004;94:960–6. doi: 10.1161/01.RES.0000122392.33172.09. [DOI] [PubMed] [Google Scholar]
- 23.Fatemi S, Hasanzadeh M, Arghami M, Sargolzaee M. Lipid Profile Comparison between Opium Addicts and non-addicts. J Teh Univ Heart Ctr. 2008;3:169–72. [Google Scholar]
- 24.Maccari S, Bassi C, Zanoni P, Plancher AC. Plasma cholesterol and triglycerides in heroin addicts. Drug Alcohol Depend. 1991;29:183–7. doi: 10.1016/0376-8716(91)90047-3. [DOI] [PubMed] [Google Scholar]