Abstract
Background
Dysregulated emotional functioning has been linked with higher cardiovascular disease (CVD) risk among adults. Early life experiences may influence the development of adulthood CVD, but few studies have examined whether potential damaging effects of dysregulated emotional function begin earlier in life. Therefore, we examined associations of child emotional functioning and the 10-year risk of developing CVD in midlife.
Methods
We studied 377 adult offspring (mean age=42.2) of Collaborative Perinatal Project participants, a U.S. cohort of pregnant women enrolled in 1959–1966. Three measures of child emotional functioning derived from psychologist ratings of behavior at 7 years of age were examined: distress proneness, attention, and inappropriate self-regulation. Adulthood 10-year CVD risk was calculated with the validated Framingham general CVD risk algorithm. Gender-specific multiple regression models assessed associations of childhood emotion and adulthood CVD risk independent of covariates measured across the life course. Potential mediators of the associations were also examined.
Results
Women had 31% higher CVD risk per standard deviation increase in childhood distress proneness (p=0.03), and 8% reduced risk per standard deviation increase in attention (p=0.09). For men, each standard deviation increase in childhood distress proneness was associated with 17% higher CVD risk (p=0.02). Associations were partly explained by adulthood body mass index and depressive symptoms in women but not in men. Inappropriate self-regulation was not associated with CVD risk.
Conclusion
Several aspects of childhood emotional functioning was associated with adulthood CVD risk, particularly for women. As such, primary prevention of CVD may be associated with addressing early life emotional functioning.
Keywords: childhood emotional functioning, life course, cardiovascular disease, New England Family Study
INTRODUCTION
Evidence is accumulating that childhood adversity and poor emotional functioning may have life-long consequences for health[1]. A life course perspective is particularly useful for identifying the origins of cardiovascular disease (CVD) as subclinical elevations of risk factors are identifiable years before the full manifestation of disease, and thus risk may be detected and addressed earlier[2]. Among adults, emotional functioning is associated with CVD morbidity and mortality[3]. As child emotional functioning provides the foundation for adult emotional functioning[4, 5], CVD risk may be attributable in part to poor emotional functioning that began early in life. However, few studies have assessed this possibility directly. Therefore, we examined the prospective association of child emotional functioning with the 10-year risk of CVD in midlife.
Recent work suggests a developmental origin of CVD risk attributable in part to childhood psychosocial adversity[6–10]. For example, among participants in the Dunedin Study (n=1037), social isolation and maltreatment experienced during childhood at ages 3–11 years were associated with CVD risk factor clustering and elevated inflammation in adulthood[8]. Though maltreatment and social isolation may induce significant distress, child emotional functioning was not assessed and may be a key pathway through which early adversity affects later CVD risk. In one of the few studies to directly assess child emotional functioning, significant associations were observed for multiple domains of emotional problems at age 7 years with inflammation and body mass index 35 years later[6]. However, another study among Dunedin men found no association of conduct problems assessed in childhood and adulthood with adult CVD risk factor clustering[11]. While the research is suggestive, whether child emotional functioning is in fact associated with adult CVD risk has not yet been determined.
Among adults, gender-specific associations for emotional functioning and CVD have been observed, suggesting women may be particularly vulnerable to deleterious effects of poor emotional functioning[12]. A recent review among adults found higher comorbidity of depression and CVD, and stronger associations of depression and psychosocial stressors with CVD for women than men[13]. However, differential gender associations have not been considered in studies examining associations of child psychosocial adversity or child emotion with adult health[8, 11, 14–16]. Therefore, it is not known whether child emotion and adult CVD associations would also differ by gender.
In this study, we examined whether child emotional functioning at 7 years was associated with adult CVD risk independent of life course demographic, socioeconomic and health factors. Where other work examined specific childhood adversities[8, 17], we focus on child emotional functioning, which may be a mechanism through which early adversity affects CVD. Also, we examined positive and negative domains of emotional functioning as we were interested in early life factors that may protect or impair cardiovascular health. We hypothesized that divergent associations for poor and adaptive child emotional functioning with adult CVD risk would be observed and associations would be stronger for women. Additionally, we hypothesized adult factors may partly explain the associations.
METHODS
Sample
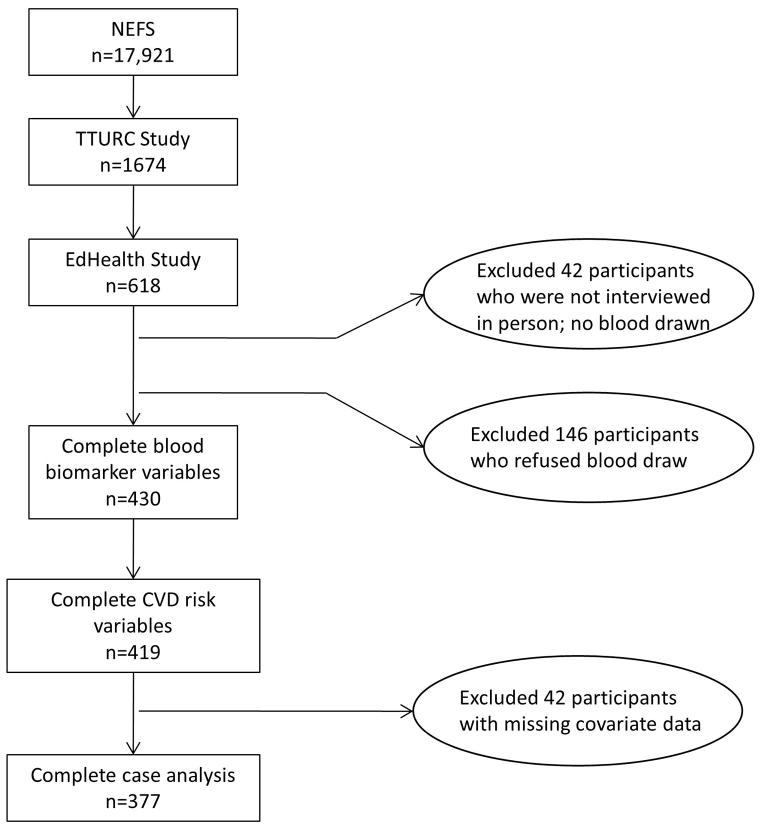
Figure 1 displays a flow chart describing how the study sample was selected. The sample comes from Collaborative Perinatal Project (CPP) offspring. Pregnant women enrolled in the CPP between 1959–1966, and their offspring were regularly assessed from birth to 7 years of age[18, 19]. The New England Family Study (NEFS) is a set of follow-up studies of the now adult offspring from the New England sites. Details on selection of the current sample is described elsewhere[16]. Briefly, our sample includes NEFS participants involved in two adult follow-up studies: the Brown-Harvard Transdisciplinary Tobacco Use Research Center (TTURC) and EdHealth. EdHealth included 618 TTURC participants, selected with preference for racial/ethnic minorities and those with low and high levels of education as required by the aims of the project. Of the 618 interviewed (69% response rate), 42 who were not interviewed in-person (and did not complete physiologic assessments) were excluded, resulting in 576 eligible participants. Of these, 430 participated in the clinical assessment, where a blood sample and anthropomorphic measurements were obtained by trained study personnel. Of these, 419 had complete outcome data. A complete case analysis was conducted among 377 individuals. There were no significant differences by gender, education, or child emotion among those who were excluded (n=241) and included in the study (n=377) (all p>0.05). Excluded individuals were older by 0.76 years (t=−5.1, p<0.001) and more likely to be white (t=4.3, p=0.04). Patterns of associations were consistent when using complete case and multiple imputation approaches, although after multiple imputation some findings become marginally significant. Given the consistency across methods, we present findings using the simpler complete case method. Human subjects committees at Brown University and Harvard School of Public Health approved this study.
Figure 1.
Flow chart of participant selection into the study.
NEFS = New England Family Study; TTURC= Transdisciplinary Tobacco Use Research Center; CVD = Cardiovascular disease
Measures
Child Emotional Functioning
Three domains of child emotional functioning identified by psychologist observations of child behavior were examined: attention, distress proneness and inappropriate self-regulation[20]. Assessments were conducted at age 7, an important developmental period when emotional functioning develops, solidifies, and can be reliably assessed[20, 21]. Past work has documented the validity of these scales against a contemporary gold standard for assessing child behavior/emotion[20, 22]. Scales are orthogonal and were selected for study as they have differentially predicted multiple domains of adult emotional functioning and health[20, 23]. Attention reflects perseverance and ability to stay focused on tasks (α=0.81). Distress proneness reflects being emotionally labile and easily frustrated (α=0.50). Inappropriate self-regulation reflects impulsivity and unrestrained behavior (α=0.71). A fourth domain (inhibition) was not examined as past work in this cohort suggests it is not associated with CVD risk[6]. Because response options for scale items were not uniform and to facilitate interpretability, scores were standardized to have mean=0, standard deviation=1. Higher scores indicate greater distress proneness, worse self-regulation and better attention. Details on scale construction and component items are described elsewhere[20]. Given the low distress proneness reliability, associations with CVD risk should be interpreted cautiously.
10-Year Calculated Risk of Cardiovascular Disease
The 10-year risk of developing a first CVD event in adulthood was calculated as a percentage using the Framingham general cardiovascular risk algorithm[24]. The algorithm has demonstrated good predictive validity in the Framingham cohorts for CVD events (c statistic=0.76 for men, 0.79 for women)[24], which include coronary death, myocardial infarction, coronary insufficiency, angina, ischemic stroke, hemorrhagic stroke, transient ischemic attack, intermittent claudication and heart failure. The algorithm uses gender-specific Cox proportional-hazard regression models that incorporate information on age, total cholesterol, HDL cholesterol, systolic blood pressure, antihypertensive medication use, smoking and diabetes.
Total and HDL cholesterol were measured in non-fasting plasma samples at CERLab (Harvard Medical School; Boston, MA) using a Hitachi 911 analyzer (Roche; Basel, Switzerland). Total cholesterol was measured enzymatically (CV=1.7%)[25]. HDL cholesterol was determined using a direct enzymatic colorimetric assay (CV=3.3%)[26]. Blood pressure was measured in seated subjects, using automated blood pressure monitors (VSMedTech BpTru, Coquitlam, BC, Canada)[27]. Physician prescribed antihypertensive medication use, physician diagnosed diabetes and current smoking were self-reported.
Covariates
Demographic, child and adult factors were considered to determine whether associations were maintained independent of life course factors, or whether associations were explained by adult factors. Demographics included age, race (white/not white) and site (Boston/Providence). Small for gestational age was determined as whether the child’s birthweight was ≤ the 10th percentile for gestational age at delivery. Body mass index (BMI; age 7) was calculated as kg/m2 using height and weight obtained by study personnel. Child IQ (age 7) was assessed using the Wechsler Intelligence Scale for Children[28]. Child health was assessed as whether the child experienced one or more chronic physical health conditions (birth-7 years) identified by study pediatricians or maternal report. Socioeconomic status (SES) was assessed with an index adapted from the U.S. Census Bureau which reflects the education, occupation and income of the head of household when the child was age 7[29] (0/low–100/high).
Adult factors were self-reported
Depressive symptoms were assessed with a Center for Epidemiologic Studies of Depression scale[30] (α=0.88). Education was assessed as total years of schooling. Physical activity was assessed with a single item regarding vigorous activity. Western and prudent dietary patterns were assessed via factor analysis from a 25-item Food Frequency Questionnaire[31, 32]. Heavy alcohol consumption was assessed as ≥2 drinks three or more times a week during the past year. Adult BMI (kg/m2) was calculated using height and weight obtained by study personnel.
Statistical Analyses
Bivariate associations for participant characteristics according to gender and child emotion were evaluated with correlations and independent t-tests. Differential gender effects of emotional functioning on CVD risk were assessed via gender stratified regression analyses and interaction terms. Multiple linear regression models assessed the associations of child emotional functioning and adult CVD risk. The distribution of CVD risk was skewed and therefore log (natural) transformed. To maintain the original units of the outcome, regression coefficients were exponentiated. Thus, β may be interpreted as percent change in CVD risk per one standard deviation increase in child emotion score[33]. Demographic and child covariates were considered potential confounders, and adult covariates were considered possible pathways by which child emotion might influence CVD. Additional analyses examined mediation by adult factors via product of coefficients[34]. Coefficients for child emotion predicting the potential mediator and the potential mediator predicting the outcome (adjusted for child emotion) were estimated and multiplied. The resulting product was divided by its standard error and that ratio was compared to a standard normal distribution to determine significance of the observed mediated effect. To evaluate which components of the CVD algorithm were most strongly related to child emotion, regression models were fit for these variables as outcomes.
RESULTS
Descriptive statistics
Participants were in their early 40’s at follow-up. Men had significantly higher CVD risk than women (Table 1). There were no significant gender differences in attention or distress proneness scores, and child emotion scores were correlated (r’s: −0.32 to 0.17; all p’s<0.05). Attention was correlated with child SES, IQ, and adult depressive symptoms (r’s: −0.11 to 0.35, all p’s<0.05). Inappropriate self-regulation was correlated with IQ, education, adulthood BMI and western diet (r’s: 0.11 to 0.18, all p’s<0.05).
Table 1.
Characteristics of study participants according to gendera
| Characteristic | Women (n=219) | Men (n=158) | pb |
|---|---|---|---|
| 10-year CVD-risk (percent), mean (SD) | 3.2 (3.5) | 7.3 (4.5) | <0.001 |
| Demographics | |||
| Age (years), mean (SD) | 42.0 (1.7) | 42.4 (1.7) | 0.01 |
| Race, not white, % | 16.4 | 20.9 | 0.27 |
| Childhood factors | |||
| Born small for gestational age, % | 12.8 | 7.6 | 0.11 |
| Socioeconomic status index, mean (SD) | 54.8 (23.0) | 53.3 (22.8) | 0.52 |
| Chronic condition, % | 17.8 | 18.4 | 0.89 |
| Intelligence quotient, mean (SD) | 100.7 (13.0) | 104.0 (13.9) | 0.02 |
| Body mass index at age 7 (kg/m2), mean (SD) | 16.1 (1.7) | 16.1 (1.4) | 0.99 |
| Adulthood factors | |||
| Depressive symptoms, mean (SD) | 1.6 (0.58) | 1.5 (0.54) | 0.16 |
| Education attainment (years), mean (SD) | 13.5 (2.4) | 13.5 (2.7) | 0.95 |
| Vigorous physical activity, % | 66.2 | 82.3 | <0.001 |
| Western diet score (z), mean (SD) | −0.02 (1.4) | 0.08 (0.48) | 0.35 |
| Prudent diet score (z), mean (SD) | 0.07 (0.69) | −0.12 (0.63) | 0.01 |
| Heavy alcohol consumptionc, % | 5.9 | 17.7 | <0.001 |
| Adult body mass index (kg/m2), mean (SD) | 28.1 (7.7) | 30.8 (7.7) | <0.001 |
Cell entries are % (n)/means (SD) for categorical/continuous variables
p-value corresponds to chi-square/independent t-tests for categorical/continuous variables
Heavy alcohol consumption reflects having more than two drinks three or more times a week during the past year.
Child emotional functioning and adult 10-year CVD risk
Controlling for demographic and child factors, a one standard deviation increase in distress proneness resulted in a 31% increase in 10-year CVD risk among women and 17% increase in 10-year CVD risk among men (Table 2). As shown in Table 1, the average likelihood of developing a first CVD event in the next ten years for women and men was 3.2% and 7.3%, respectively. Our models suggest that a one standard deviation increase in distress proneness increases this risk by 31% (women) and 17% (men), thereby increasing the likelihood of a CVD event in the next 10 years to 4.2% for women (3.2+[.31*3.2]=4.2) and 8.5% for men (7.3+[.17*7.3]=8.5). As CVD remains the leading cause of death world-wide[35], this level of increased risk is considered to be potentially clinically relevant at a population level. The interaction between distress proneness and gender was not significant (β=0.09, se=0.16, p=0.57). Furthermore, a one standard deviation increase in attention was marginally associated with a 7.8% decreased 10-year CVD risk for women (p=0.09). This suggests that among women, the ten year likelihood of developing a first CVD event may be reduced from 3.2% (Table 1) to 2.9% per standard deviation increase in child attention (3.2− [.078*3.2]=2.9). Attention was not associated with CVD risk for men. The interaction between gender and attention was not significant (β= −0.09, se=0.07, p=0.20). Inappropriate self-regulation was not associated with CVD risk in any model.
Table 2.
Multiple linear regression coefficients (standard error) representing change in adult 10-year CVD risk per one standard deviation change in child emotional functioninga
| Unadjusted | Demographicb | Childhoodc | Pathwaysd | |
|---|---|---|---|---|
| Distress Proneness | ||||
| Women | 24.4 (1.1) 0.11 |
33.9 (1.1) 0.02 |
31.1 (1.1) 0.03 |
11.3 (1.1) 0.30 |
| Men | 14.0 (1.1) 0.04 |
16.1 (1.1) 0.04 |
17.1 (1.1) 0.02 |
16.7 (1.1) 0.002 |
| Attention | ||||
| Women | −11.1 (1.1) 0.03 |
−10.1 (1.1) 0.03 |
−7.8 (1.1) 0.09 |
−4.6 (1.0) 0.30 |
| Men | −2.9 (1.0) 0.53 |
−4.7 (1.0) 0.30 |
−3.8 (1.0) 0.39 |
−2.8 (1.0) 0.44 |
| Inappropriate Self Reg. | ||||
| Women | 1.0 (1.1) 0.86 |
1.0 (1.1) 0.41 |
1.1 (1.1) 0.19 |
1.0 (1.1) 0.99 |
| Men | 1.0 (1.1) 0.47 |
1.0 (1.1) 0.52 |
1.0 (1.1) 0.62 |
1.0 (1.1) 0.89 |
Top cell entries are β(SE); bottom cell entries p-values
Demographic model adjusts for site, age and race
Childhood model adjusts for demographic and childhood factors (born small for gestational age, SES, health, IQ, body mass index)
Pathways model adjusts for demographic, child and adulthood factors (education, depressive symptoms, physical activity, body mass index, alcohol use, diet)
Adulthood pathways between child emotion and adult CVD risk
Given the attenuated distress proneness and attention coefficients in pathways models among women, we examined which adult factor might explain the association (Table 3). For women, a one standard deviation increase in distress proneness was associated with a 2.92 kg/m2 higher adult BMI (p<0.001). Adult BMI was associated with CVD risk (β=1.0, se=1.0, p<0.001) when controlling for distress proneness and other study covariates. The mediated effect was significant (product of coefficients=2.92, 95%CI: 2.85, 2.99; p<0.001) indicating that adult BMI may be on the pathway between child distress proneness and adult CVD risk for women. Also among women, greater child attention was associated with fewer depressive symptoms (p=0.03). The association for adult depressive symptoms and CVD risk was not significant (β=1.1, se=1.0, p=0.10). The mediated effect was not significant (product of coefficients=−0.01, 95%CI: −0.02, 0.005; p=0.19) indicating adult depressive symptoms do not significantly mediate the association child attention and adult CVD risk for women.
Table 3.
Linear and logistic regression analyses for the association of childhood emotional functioning and potential adulthood pathway factorsa
| Potential pathway variable | Distress Proneness | Attention | ||
|---|---|---|---|---|
| B(SE) | p | B(SE) | p | |
| Education attainment | ||||
| Women | −0.27 (0.37) | 0.46 | −0.06 (0.18) | 0.74 |
| Men | 0.09 (0.29) | 0.77 | 0.10 (0.20) | 0.62 |
| Depressive symptoms | ||||
| Women | 0.03 (0.07) | 0.72 | −0.09 (0.04) | 0.03 |
| Men | −0.03 (0.05) | 0.59 | −0.005 (0.04) | 0.90 |
| Body mass index | ||||
| Women | 2.92 (0.75) | <0.001 | 0.02 (0.64) | 0.98 |
| Men | 0.28 (0.55) | 0.61 | −0.45 (0.73) | 0.53 |
| Western diet | ||||
| Women | −0.14 (0.14) | 0.31 | 0.02 (0.06) | 0.67 |
| Men | 0.08 (0.06) | 0.22 | −0.01 (0.04) | 0.85 |
| Prudent diet | ||||
| Women | 0.01 (0.06) | 0.82 | 0.05 (0.04) | 0.41 |
| Men | 0.05 (0.05) | 0.27 | −0.06 (0.07) | 0.38 |
|
| ||||
| OR | 95% CI | OR | 95% CI | |
|
| ||||
| Vigorous physical activity | ||||
| Women | 1.77 | 0.80, 3.93 | 1.22 | 0.87, 1.73 |
| Men | 1.01 | 0.47, 2.17 | 1.15 | 0.77, 1.71 |
| Heavy drinking | ||||
| Women | 1.95 | 0.86, 4.45 | 1.15 | 0.39, 3.38 |
| Men | 0.87 | 0.40, 1.89 | 1.09 | 0.61, 1.92 |
Models are adjusted for demographic, childhood and adulthood covariates. Significant associations (p<0.05) are shown in bold.
Childhood emotional functioning and components of the CVD-risk algorithm
To evaluate which algorithm components were most strongly related to distress and attention, separate models were fit with the components as outcomes (Table 4). Distress proneness was associated with systolic blood pressure in men (β=6.95, SE=2.24), diabetes (OR=4.07, 95%CI: 1.21, 13.74) and antihypertensive medication use (OR=3.31, 95%CI: 1.56, 7.02) among women. Attention was not associated with any algorithm component for either gender.
Table 4.
Linear and logistic regression analyses for the association of childhood emotional functioning and modifiable components of the 10-year CVD risk algorithm
| Algorithm component | Overall M(SD) | Distress Proneness | Attention | ||
|---|---|---|---|---|---|
| β(SE) | p | β(SE) | p | ||
| Total cholesterol, mg/dL | |||||
| Women | 192.07 (38.69) | −0.25 (6.28) | 0.97 | −1.99 (2.56) | 0.44 |
| Men | 202.04 (40.65) | 5.41 (4.55) | 0.23 | −4.89 (3.78) | 0.20 |
| HDL cholesterol, mg/dL | |||||
| Women | 54.66 (17.34) | −3.29 (1.96) | 0.08 | 0.73 (1.14) | 0.52 |
| Men | 42.24 (12.23) | −0.40 (1.05) | 0.75 | −0.12 (1.03) | 0.91 |
| Systolic blood pressure, mmHg | |||||
| Women | 110.98 (15.40) | 1.58 (2.54) | 0.53 | −0.69 (1.14) | 0.55 |
| Men | 119.43 (14.61) | 6.95 (2.24) | 0.002 | 0.42 (1.34) | 0.75 |
|
| |||||
| % | OR | 95% CI | OR | 95% CI | |
|
| |||||
| Antihypertensive medication use | |||||
| Women | 10.96 | 3.31 | 1.56, 7.02 | 0.75 | 0.51, 1.11 |
| Men | 11.39 | 0.64 | 0.22, 1.93 | 0.69 | 0.41, 1.16 |
| Smoker | |||||
| Women | 31.51 | 1.46 | 0.75, 2.87 | 0.88 | 0.62, 1.25 |
| Men | 22.78 | 1.48 | 0.83, 2.67 | 0.90 | 0.61, 1.31 |
| Diabetes | |||||
| Women | 4.57 | 4.07 | 1.21, 13.74 | 0.61 | 0.31, 1.17 |
| Menb | 3.80 | -- | -- | -- | -- |
Models are adjusted for demographics and childhood covariates. Significant associations (p<0.05) are shown in bold.
Associations with diabetes for men could not be reliably estimated due to low n.
DISCUSSION
This study provides evidence that child emotional functioning is associated with adult CVD risk. Gender-specific pathways were identified and associations were particularly robust for women. Specifically, child distress proneness was associated with adult CVD risk more strongly among women than men, and adult BMI significantly mediated the association for women. Also among women, better child attention was associated with lower adult CVD risk, with some suggestion that adult depressive symptoms may help explain the association. For men, distress proneness, but not attention, was associated with adult CVD risk. These findings are particularly novel as this study is among the first to consider CVD risk as having some developmental origins in child emotional functioning.
Child inappropriate self-regulation was not associated with CVD risk. This was surprising given previously reported associations with other cardiovascular risk markers including C-reactive protein and BMI[6]. However, neither BMI nor inflammation was a component of the algorithm. Moreover, the child emotion measures are orthogonal and associate with different domains of adult emotional functioning[20]. Therefore, different emotion measures may not necessarily associate with the same outcomes.
Among women, CVD risk attributable to distress proneness was driven in part by hypertension (indexed by medication use) and diabetes, which are consequences of having high BMI. Attention was not associated with algorithm components, suggesting that lower CVD risk attributable to better child attention may involve a complex interaction of multiple factors. Among men, systolic blood pressure was associated with distress proneness, suggesting untreated hypertension may help explain the association.
The stronger associations between child emotional functioning and CVD risk among women may suggest that women may be more vulnerable to childhood distress than men, while also being more influenced by the protective effects of attention. This is congruent with what has been observed among adults[13]. Moreover, adult BMI mediated the association of distress proneness and CVD risk for women but not men. This is also consistent with recent adult weight status studies that find women to be more vulnerable to the deleterious effects of poor emotional functioning than men[12, 36]. As this is an emerging area of research, findings to date have been largely descriptive. We do not know why poor emotional functioning may contribute to higher risks for women. It may be that distress is associated with gender-patterned risk behaviors that contribute differentially to BMI and CVD[37]. We encourage future work to explore causes of gender patterning in emotion, BMI and CVD risk associations.
Latency and accumulation of risk models[1, 38] may help explain child emotion and adult CVD risk associations. Persistent distress is associated with hypothalamic-pituitary-adrenal axis[39] dysregulation, which is related to a range of CVD risk markers including inhibited glucocorticoid processes (which promote weight gain over time)[39] and systemic inflammation[3, 40]. A latency explanation would suggest that poor child emotional functioning may alter such body systems during sensitive periods of development and shape later risk. Distress is also associated with CVD risk behaviors[3, 37]. An accumulation explanation would suggest that child emotional functioning sets in motion a series of behaviors that cumulatively determine CVD risk. As we measured child emotion once during this study, we encourage future work to examine latency and accumulation of risk hypotheses using multiple measures of emotion and CVD risk to better evaluate how these factors are associated over time.
This study has a number of strengths. We used a validated algorithm that incorporated biomarkers to estimate CVD risk. Also, child emotion was directly assessed by a psychologist and temporally precedes the outcome. Moreover, a broad representation of life course covariates were addressed and measured in several ways. This study also has limitations. First, contemporary measures of child emotional functioning may be more accurate. Use of imprecise measures could yield null or weak associations. Also, outcome and pathway variables were assessed concurrently making tests of mediation less robust. Additionally, generalizability may be limited as participant selection was based on certain characteristics per the project aims. Also, associations may appear stronger than the true effect due to multiple testing. Finally, distress proneness findings should be interpreted cautiously due to low scale reliability. These limitations notwithstanding, this study adds to the literature in several ways. It is among the first to link prospectively assessed positive and negative child emotion domains to adult CVD risk using a validated prediction algorithm. Where previous work has focused on severe forms of adversity[8] or psychiatric morbidity[7], we examine functioning that is likely to be more common in the general population. Also, this study is among the first to examine gender-specific associations of child emotional functioning and adult CVD risk and pathways though which emotion influences cardiovascular health.
Evidence is accumulating that several adult diseases have developmental origins in child psychosocial adversity[1]. This study adds to this emerging literature and demonstrates that child emotional functioning is associated with midlife CVD risk, particularly for women. It further suggests that identification of risk is possible much earlier in life than has previously been considered. While cardiovascular experts acknowledge that childhood is a life stage likely to be particularly amenable to CVD prevention[41], public health and biomedicine have not focused on the sensitivity of child emotion development as a prevention or intervention target. This study suggests that doing so may not only enhance child emotional development, but may also protect cardiovascular health for a lifetime.
What is already known
Childhood adversity, which is hypothesized to induce significant emotional distress, is associated with CVD risk in adulthood.
Among adults, emotional functioning is associated with CVD, with associations being more robust for women than men.
It is not known whether childhood emotional functioning would be associated with CVD risk in adulthood, or whether such associations would be differentially patterned by gender.
What this study adds
This study is among the first to examine the gender-specific associations and pathways linking childhood emotional functioning and adulthood CVD risk.
Findings indicate that childhood emotional functioning is associated with significant CVD risk, particularly for women.
Findings suggest that addressing poor emotional functioning during childhood may help protect cardiovascular health for a lifetime.
Acknowledgments
Funding Statement: This work is supported by National Institutes of Health (NIH) Transdisciplinary Tobacco Use Research Center (TTURC) Award (P50 CA084719) by the National Cancer Institute, the National Institute on Drug Abuse, the National Institute of Aging grant AG023397, and the Robert Wood Johnson Foundation’s Pioneer Portfolio, through a grant, “Exploring Concepts of Positive Health.” Dr. Appleton is supported by the National Heart Lung and Blood Institute Training Grant at the Harvard School of Public Health (T32HL098048) and the Quantitative Biomedical Sciences training program at Geisel School of Medicine at Dartmouth (R25CA134286).
Footnotes
Competing Interest: None to declare.
Contributorship Statement:
Allison A. Appleton: Dr. Appleton conceptualized and designed the study, performed the data analyses, drafted, reviewed and revised the final manuscript as submitted.
Eric Loucks: Dr. Loucks reviewed data analyses, provided analytic consultation, reviewed and revised the final manuscript as submitted.
Stephen Buka: Dr. Buka reviewed data analyses, reviewed and revised the final manuscript as submitted.
Eric Rimm: Dr. Rimm reviewed data analyses, reviewed and revised the final manuscript as submitted.
Laura D. Kubzansky: Dr. Kubzansky conceptualized and designed the study, reviewed data analyses, reviewed and revised the final manuscript as submitted.
References
- 1.Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities. Journal of the American Medical Association. 2009;301:2252–9. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 2.Berenson GS, Srnivasan SR. Cardiovascular risk factors in youth with implications for aging: The Bogalusa heart study. Neurobiology of Aging. 2005;26:303–7. doi: 10.1016/j.neurobiolaging.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 3.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular disease. Annual Review of Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- 4.Caspi A. The child is father of the man: Personality continuities from childhood to adulthood. Journal of Personality and Social Psychology. 2000;78:158–72. doi: 10.1037//0022-3514.78.1.158. [DOI] [PubMed] [Google Scholar]
- 5.Caspi A, Moffitt TE, Newman DL. Behavioral observations at age 3 years predict adult psychiatric disorders: longitudinal evidence from a birth cohort. Archives of General Psychiatry. 1996;53:1033–9. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]
- 6.Appleton AA, Buka SL, McCormick MC, et al. Emotional functioning at age 7 years is associated with C-reactive protein in middle adulthood. Psychosomatic Medicine. 2011;73:295–303. doi: 10.1097/PSY.0b013e31821534f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goodwin RD, Sourander A, Duarte CS, et al. Do mental health problems in childhood predict chronic physical conditions among males in early adulthood? Evidence from a community-based prospective study. Psychological Medicine. 2008;39:301–11. doi: 10.1017/S0033291708003504. [DOI] [PubMed] [Google Scholar]
- 8.Danese A, Moffitt TE, Harrington H, et al. Adverse childhood experiences and adult risk factors for age-related disease: Depression, inflammation, and metabolic risk markers. Archives of Pediatric and Adolescent Medicine. 2009;63:1135–43. doi: 10.1001/archpediatrics.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Danese A, Moffitt TE, Pariante CM, et al. Elevated inflammation levels in depressed adults with a history of childhood maltreatment. Archives of General Psychiatry. 2008;65:409–16. doi: 10.1001/archpsyc.65.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loucks EB, Almeida ND, Taylor SE, et al. Childhood family psychosocial environment and coronary heart disease risk. Psychosomatic Medicine. 2011;73:563–71. doi: 10.1097/PSY.0b013e318228c820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Odgers CL, Caspi A, Broadbent JM, et al. Prediction of differential adult health burden by conduct problem subtypes in males. Archives of General Psychiatry. 2007;64:476–83. doi: 10.1001/archpsyc.64.4.476. [DOI] [PubMed] [Google Scholar]
- 12.Thurston RC, Kubzansky LD. Multiple sources of psychosocial disadvantage and risk of coronary heart disease. Psychosomatic Medicine. 2007;69:748–55. doi: 10.1097/PSY.0b013e31815772a3. [DOI] [PubMed] [Google Scholar]
- 13.Moller-Leimkuhler A. Higher comorbidity of depression and cardiovascular disease in women: a biopsychosocial perspective. World Journal of Biological Psychiatry. 2010;11:922–33. doi: 10.3109/15622975.2010.523481. [DOI] [PubMed] [Google Scholar]
- 14.Danese A, Pariante CM, Caspi A, et al. Childhood maltreatment predicts adult inflammation in a life-course study. PNAS. 2007;104:1319–24. doi: 10.1073/pnas.0610362104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goodwin RD, Sourander A, Duarte CS, et al. Do mental health problems in childhood predict chronic physical conditions among males in early adulthood? Evidence from a community-based prospective study. Psychological Medicine. 2008;39:301–11. doi: 10.1017/S0033291708003504. [DOI] [PubMed] [Google Scholar]
- 16.Almeida ND, Loucks EB, Kubzansky LD, et al. Quality of parental emotional care and calculated risk for coronary heart disease. Psychosomatic Medicine. 2010;72:148–55. doi: 10.1097/PSY.0b013e3181c925cb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caspi A, Harrington H, Moffitt TE, et al. Socially isolated children 20 years later: risk of cardiovascular disease. Archives of Pediatric and Adolescent Medicine. 2006;160:805–11. doi: 10.1001/archpedi.160.8.805. [DOI] [PubMed] [Google Scholar]
- 18.Broman SH, Nichols PI, Kennedy WA. Preschool IQ: Prenatal and Early Developmental Correlates. New York: Hallstead Press; 1975. [Google Scholar]
- 19.Niswander KR, Gordon M. The women and their pregnancies. Washington, DC: US Government Printing Office; 1972. [Google Scholar]
- 20.Kubzansky LD, Martin LT, Buka SL. Early manifestations of personality and adult emotional functioning. Emotion. 2004;4:364–77. doi: 10.1037/1528-3542.4.4.364. [DOI] [PubMed] [Google Scholar]
- 21.Rothbart MK, Ahadi SA, Hershey KL, et al. Investigations of temperament at three to seven years: The Children’s Behavior Questionnaire. Child Development. 2001;72:1394–408. doi: 10.1111/1467-8624.00355. [DOI] [PubMed] [Google Scholar]
- 22.Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 profile. Burlington: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- 23.Kubzansky LD, Martin LT, Buka SL. Early manifestations of personality and adult health: A life course perspective. Health Psychology. 2009;28:364–72. doi: 10.1037/a0014428. [DOI] [PubMed] [Google Scholar]
- 24.D’Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation. 2008;117:742–53. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 25.Allain CC, Poon LS, Chan CS, et al. Enzymatic determination of total serum cholesterol. Clinical Chemistry. 1974;20:470–5. [PubMed] [Google Scholar]
- 26.Rafai N, Cole TG, Iannotti E, et al. Assessment of interlaboratory performance in external proficiency testing programs with a direct HDL-cholesterol assay. Clinical Chemistry. 1998;44:1452–8. [PubMed] [Google Scholar]
- 27.Mattu GS, Heran BS, Wright JM. Overall accuracy of the BpTRU - an automated electronic blood pressure device. Blood Pressure Monitoring. 2004;9:47–52. doi: 10.1097/00126097-200402000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Wechsler D. Wechsler Intelligence Scale for Children. New York: The Psychological Corporation; 1949. [Google Scholar]
- 29.Myrianthopoulos N, French K. An application of the U.S. Bureau of the Census socioeconomic index to a large, diversified patient population. Social Science & Medicine. 1968;2:283–99. doi: 10.1016/0037-7856(68)90004-8. [DOI] [PubMed] [Google Scholar]
- 30.Radloff LS. CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 31.Willett WC. Nutritional Epidemiology. New York: Oxford University Press; 1998. [Google Scholar]
- 32.Michaud DS, Skinner HG, Wu K, et al. Dietary patterns and pancreatic cancer cancer risk in men and women. Journal of the National Cancer Institute. 2005;97:518–24. doi: 10.1093/jnci/dji094. [DOI] [PubMed] [Google Scholar]
- 33.UCLA Academic Technology Services Statistical Consulting Group. Introduction to SAS. 2011. [Google Scholar]
- 34.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mendis S, Puska P, Norrving B. Global atlas on cardiovascular disease prevention and control. Geneva: 2011. [Google Scholar]
- 36.de Wit L, Luppino F, van Straten A, et al. Depression and obesity: a meta analysis of community based studies. Psychiatry Research. 2010;178:230–5. doi: 10.1016/j.psychres.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 37.Blaine B. Does depression cause obesity?: A meta-analysis of longitudinal studies of depression and weight control. Journal of Health Psychology. 2008;13:1190–7. doi: 10.1177/1359105308095977. [DOI] [PubMed] [Google Scholar]
- 38.Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology. 2002;31:285–93. [PubMed] [Google Scholar]
- 39.Luppino FS, de Wit LM, Bouvy PF, et al. Obesity, overweight, and depression: a systematic review and meta-analysis of longitudinal studies. Archives of General Psychiatry. 2010;67:220–9. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 40.Deverts DJ, Cohen S, DiLillo VG, et al. Depressive symptoms, race, and circulating C-reactive protein: The coronary artery risk development in young adults (CARDIA) study. Psychosomatic Medicine. 2010;72:734–41. doi: 10.1097/PSY.0b013e3181ec4b98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]