Abstract
Background
Despite evidence to suggest significant spatial variation in out-of-hospital cardiac arrest (OHCA) and bystander cardiopulmonary resuscitation (BCPR) rates, geographic information systems (GIS) and spatial analysis have not been widely used to understand the reasons behind this variation. This study employs spatial statistics to identify the location and extent of clusters of bystander CPR in Houston and Travis County, TX.
Methods
Data were extracted from the Cardiac Arrest Registry to Enhance Survival for two U.S. sites –Austin-Travis County EMS and the Houston Fire Department – between October 1, 2006 and December 31, 2009. Hierarchical logistic regression models were used to assess the relationship between income and racial/ethnic composition of a neighborhood and BCPR for OHCA and to adjust expected counts of BCPR for spatial cluster analysis. The spatial scan statistic was used to find the geographic extent of clusters of high and low BCPR.
Results
Results indicate spatial clusters of lower than expected BCPR rates in Houston. Compared to BCPR rates in the rest of the community, there was a circular area of 4.2 km radius where BCPR rates were lower than expected (RR = 0.62; p < 0.0001 and RR = 0.55; p = 0.037) which persist when adjusted for individual-level patient characteristics (RR = 0.34; p = 0.027) and neighborhood-level race (RR = 0.34; p = 0.034) and household income (RR = 0.34; p = 0.046). We also find a spatial cluster of higher than expected BCPR in Austin. Compared to the rest of the community, there was a 23.8 km radius area where BCPR rates were higher than expected (RR = 1.75; p = 0.07) which disappears after controlling for individual-level characteristics.
Conclusions
A geographically targeted CPR training strategy which is tailored to individual and neighborhood population characteristics may be effective in reducing existing disparities in the provision of bystander CPR for out-of-hospital cardiac arrest.
Keywords: Bystander CPR, Out of hospital cardiac arrest, Spatial cluster analysis, Geographic information systems, CARES, Multilevel models
1. Introduction
Geographic information systems (GIS) have a well-documented history within EMS systems as a tool for optimizing service delivery by decreasing response times and defining more efficient service areas1–4. But despite evidence to suggest significant spatial variation in out-of-hospital cardiac arrest (OHCA) and bystander cardiopulmonary resuscitation (CPR) rates,5–8 GIS and spatial analysis have not been widely used to understand the reasons behind this variation. Studies conducted in Memphis,9 Chicago,10 Atlanta11 and Canada12 have demonstrated that patients who are African-American and/or of lower socioeconomic status are less likely to receive bystander CPR and survive an OHCA. These studies, however, have not taken into account the contextual, or neighborhood, factors that may influence the variation in OHCA and bystander CPR rates. It is entirely possible that a layperson’s knowledge of and willingness to provide CPR may vary based on the area in which they live. But there is limited research that examines this theory. The few studies that have been done show increased rates of OHCA incidence associated with lower income neighborhoods,13 and increased odds of receiving bystander CPR associated with higher neighborhood income or property values.11,14 Reasons for willingness to provide CPR may include a person’s perception of neighborhood safety, quality and quantity of social interactions with neighbors, fear of performing CPR incorrectly15,16 or the perceived need to breathe into a person’s mouth.17,18
Spatial cluster analysis is a statistical method that has not been used to examine bystander CPR or cardiac arrest events. While spatial cluster analysis is not new to epidemiology, its application to cardiovascular health services research has been minimal, and there are currently no published studies examining how the clustering of bystander CPR varies directly with socioeconomic characteristics. Identification of clusters of bystander CPR may uncover possible neighborhood-level socioeconomic factors that influence an individual’s willingness to perform CPR. Identification of clusters may also indicate areas or neighborhoods that should be targeted for CPR training interventions. However, researchers must be careful in applying clustering methodologies and properly adjust for underlying population distribution and known covariates so that we can accurately interpret the reasons that bystander CPR appears to cluster in space. Given that studies have shown that CPR training drastically increases a lay person’s willingness and ability to perform CPR,19–22 the identification of specific areas in a city to target such interventions may be invaluable for public health professionals.
In this study we use the spatial scan statistic, a statistical method for detecting events that cluster in space,23 to identify the location and geographic size of clusters of bystander CPR in Houston and Travis County, TX. We sought to answer two main study questions: (1) Do significant clusters of bystander CPR occur in these communities and, if so, what are the approximate locations of these clusters? (2) If these clusters are adjusted for neighborhood-level risk factors (income and race) do they persist or disappear?
2. Methods
2.1. Data collection and analysis
This is a secondary analysis of the out-of-hospital cardiac arrest surveillance registry CARES (Cardiac Arrest Registry to Enhance Survival). CARES is an emergency medical services (EMS) web-based registry for out-of-hospital cardiac arrest, in which review of EMS logs is coupled with selected, anonymized extraction of hospital information. Detailed information about this registry is published elsewhere.24 From January 1, 2007 to December 31, 2009 in Houston, TX and from October 1, 2006 to December 31, 2009 in Travis County, TX, CARES captured all 911-activated cardiac arrest events in which resuscitation was attempted and the cause of arrest was presumed to be cardiac. During the data review process, analysts from CARES confirmed the capture of all cardiac arrests by the city’s 911 center. The EMS agencies prospectively submitted data in accordance with the CARES user agreement. Further details on case ascertainment, data collection and coding can be found in McNally et al.25
All cases submitted to the registry during the study interval (Houston: n = 3811, Travis: n = 1410) were eligible for inclusion in the study. A case was excluded if: (1) the patient was not eligible for bystander CPR by a non-health care professional because of the ready availability of health care professionals (e.g., patient’s arrest occurred in a medical facility such as a hospital, nursing home or physician’s office) or the event was witnessed by EMS (Houston: n = 1106, Travis: n = 358); (2) data documenting the patient’s clinical outcome was missing (Houston: n = 42, Travis: n = 2), (3) the patient’s cardiac arrest location address could not be mapped (Houston: n = 13, Travis: n = 0), or (4) the event occurred in an airport (Houston: n = 15, Travis: n = 3).
The CARES dataset was geocoded based upon the address of the cardiac arrest event using ArcGIS (ESRI, Redlands, CA). Census block group variables were linked to each geocoded address in ArcGIS using the 2000 Census Cartographic Boundary files and Summary File 3.26 Patient-level factors were obtained from the CARES registry. They included: race (white, black, Hispanic, other/unknown), location of arrest (public location vs. private residence), witnessed arrest (arrest witnessed by someone other than the first responder/EMS provider) and who initiated CPR (as coded by the EMS provider). Any bystander, who was not part of the medical or 911 response team, was considered eligible to initiate bystander CPR. Census block group variables included: median household income, percent of the population living below the federal poverty line, percent of the population with less than a high school education and percent of the population in different racial/ethnic categories (white, black, Asian and Hispanic).
This study was approved by the Emory University institutional review board, which waived the requirement for informed consent because the analysis included only de-identified data.
2.2. Cluster detection methods
In order to explore geographic clustering of bystander CPR, we used the spatial scan statistic23,27 in the SaTScan software28 to detect the location of and evaluate the statistical significance of high and low geographic clusters of bystander CPR events. Houston and Travis County were examined in separate analyses. The spatial scan statistic imposes a circular window on the study area and moves the center of this window across the area. The center of the window is located at each block group centroid, and the radius of the circular window is allowed to vary so that the circle includes from zero up to 50 percent of the total number of OHCA cases. This method creates a very large number of distinct but overlapping circular windows, each with a different set of neighboring census blocks in it, and each a possible cluster of bystander CPR. The number of observed and expected cases of bystander CPR inside and outside each circle is tabulated and used to calculate a likelihood ratio test statistic. The circle with the maximum likelihood is the most likely or primary cluster, that is, the cluster with a statistically higher number of observed cases than the number of cases expected given the underlying population of OHCAs. P-values were derived from 9999 simulated Monte Carlo replications under the null hypothesis of spatial randomness of cardiac arrest events. The circular clusters displayed on the maps represent the approximate boundaries of the cluster, that is, the geographic extent of the block groups included in the circular window with the highest log likelihood ratio.
We conducted two separate cluster detection analyses in each study area. In the unadjusted analysis, under the null hypothesis, the expected number of bystander CPR events in a block group was calculated by multiplying the total number of OHCA events in the block group by the city-wide rate of bystander CPR. Thus, each block group is expected to have the same rate of bystander CPR as the city as a whole. In the two adjusted analyses, the expected number of bystander CPR events was calculated using the predicted probabilities of bystander CPR derived from a regression model containing individual case characteristics and from a second hierarchical regression model which included both individual- and neighborhood-level covariates. The hierarchical regression methods used to develop these adjusted counts are described below and in more detail in the supplementary material. The number of bystander CPR events in each block group was modeled as a Poisson distribution.
For each cluster identified, we list the radius, number of block groups in the cluster, the observed vs. expected number of bystander CPR events, the relative risk and the p-value. The relative risk is the risk of the respective outcome within the cluster, compared to the population’s risk. We report the primary cluster for each analysis, regardless of statistical significance, and any secondary clusters with p < 0.05. We only considered clusters with p < 0.05 statistically significant.
2.3. Hierarchical linear models (HLMs) used to adjust cluster models
We used the predicted probabilities derived from hierarchical logistic regression models to calculate the expected count of bystander CPR events in each block group (see supplementary material for detailed methodology). We used a 2-level model to account for the nesting of patients (level 1) within neighborhoods (defined as census block group) (level 2). Individual-level characteristics and neighborhood-level characteristics (models C and D in Table 2) were added as fixed effects and included a random effect of neighborhood to the model to examine their independent contributions. Race, income, educational attainment and poverty were initially used to explore the effect of neighborhood context on bystander CPR. The final models included race and median household income and were chosen based on the greatest proportion of variance explained by individual and neighborhood variables across both study sites. Hierarchical modeling was conducted using SAS v9.2 software.
Table 2.
Final hierarchical logistic regression model results for provision of bystander cardiopulmonary resuscitation (CPR) used to adjust geographic clusters. Model C includes individual-level characteristics and neighborhood-level percent white. Model D includes individual-level characteristics and neighborhood-level median household income.
| Houston
|
Austin-Travis County
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Model C: Neighborhood % white
|
Model D: Neighborhood median household income
|
Model C: Neighborhood % white
|
Model D: Neighborhood median household income
|
|||||
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| Individual-level variables | ||||||||
| Age (decades) | 0.92 | (0.88–0.97) | 0.92 | (0.88–0.97) | 0.94 | (0.87–1.02) | 0.94 | (0.87–1.03) |
| Female sex | 0.94 | (0.78–1.13) | 0.94 | (0.78–1.13) | 1.25 | (0.92–1.71) | 1.26 | (0.92–1.73) |
| Race/ethnicity | ||||||||
| White | Ref | Ref | Ref | Ref | ||||
| Black | 0.67 | (0.51–0.87) | 0.64 | (0.51–0.79) | 1.02 | (0.52–1.99) | 0.86 | (0.44–1.65) |
| Hispanic/Latino | 0.62 | (0.48–0.81) | 0.63 | (0.48–0.82) | 1.13 | (0.69–1.84) | 1.12 | (0.69–1.83) |
| Other/unknown | 0.93 | (0.59–1.47) | 0.92 | (0.58–1.44) | 0.84 | (0.58–1.20) | 0.8 | (0.56–1.15) |
| Witnessed arrest | 2.12 | (1.77–2.54) | 2.11 | (1.76–2.53) | 1.63 | (1.21–2.20) | 1.63 | (1.21–2.19) |
| Public arrest | 1.32 | (1.07–1.64) | 1.34 | (1.08–1.67) | 2.2 | (2.44–9.59) | 2.5 | (1.76–3.58) |
| Neighborhood-level variables | ||||||||
| Percent white | 1.28 | (0.86–1.90) | 1.65 | (1.12–2.42) | ||||
| Median household income | 1.00 | (0.99–1.01) | 1.01 | (1.01–1.02) | ||||
3. Results
3.1. Houston
Of 2,630 eligible OHCA events in Houston, 773 (29.7%) patients received bystander CPR. The patient- and neighborhood-level characteristics of the eligible arrests stratified by performance of bystander CPR are displayed in Table 1. The final hierarchical logistic regression models with adjusted odds ratios used to derive the expected counts of bystander CPR for the cluster analysis are shown in Table 2. Patients who were black (OR 0.67; 95% CI 0.51–0.87) or Latino (OR 0.62; 95% CI 0.48–0.81) were less likely to receive bystander CPR. Arrests that were witnessed (OR 2.12; 95% CI 1.77–2.54) and occurred in a public location (OR 1.32; 95% CI 1.07–1.64) were more likely to receive bystander CPR. Census block characteristics were not significantly associated with a likelihood of receiving bystander CPR in Houston.
Table 1.
Patient demographics and neighborhood characteristics stratified by performance of bystander cardiopulmonary resuscitation (CPR).
| Houston
|
Austin-Travis County
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Did not receive bystander CPR (N = 1830)
|
Received bystander CPR (N = 773)
|
Did not receive bystander CPR (N = 626)
|
Received bystander CPR (N = 417)
|
|||||
| N | (%) | N | (%) | N | (%) | N | (%) | |
| Individual-level variables | ||||||||
| Agea | 61.2 | 19.8 | 59.1 | 19.6 | 62.4 | 17.7 | 60.6 | 17.8 |
| Female sex | 736 | 40.2 | 274 | 35.5 | 140 | 34.0 | 213 | 33.6 |
| Race/ethnicity | ||||||||
| White | 536 | 29.3 | 310 | 40.1 | 128 | 20.5 | 104 | 24.9 |
| Black | 895 | 48.9 | 303 | 39.2 | 47 | 7.5 | 23 | 5.5 |
| Hispanic/Latino | 334 | 18.3 | 124 | 16.2 | 87 | 13.9 | 70 | 16.8 |
| Other/unknown | 65 | 3.6 | 35 | 4.5 | 364 | 58.2 | 220 | 52.8 |
| Witnessed arrest | 692 | 37.8 | 445 | 57.6 | 224 | 35.8 | 202 | 48.4 |
| Public arrest | 320 | 17.5 | 207 | 26.8 | 115 | 18.4 | 143 | 34.3 |
| Neighborhood-level variablesb | ||||||||
| Percent whitea | 39.8 | 28.9 | 46.2 | 29.2 | 62.9 | 24.8 | 71 | 21.6 |
| Median household incomea | 36,243 | 21,743 | 40,383 | 25,264 | 48,402 | 24,762 | 56,400 | 30,694 |
Numbers represent the mean and standard deviation.
Neighborhood-level variables were calculated by averaging the percent white and median HH income for all census block groups containing individuals who did not receive bystander CPR and separately for all census block groups containing individuals who did receive bystander CPR. There is some overlap (e.g., some census block groups contain both individuals who did and did not received bystander CPR, so that some census block groups may be double counted in these calculations.
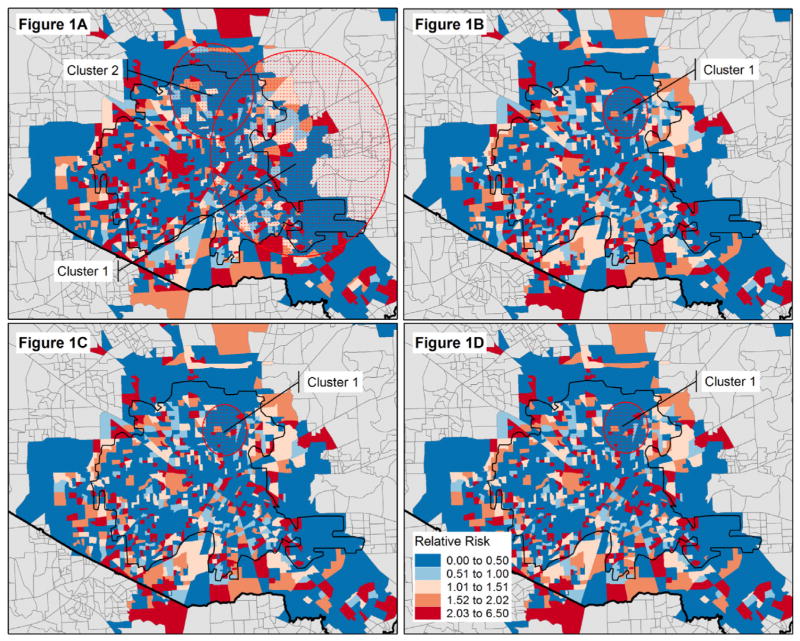
Table 3 and Fig. 1A identify two overlapping clusters with statistically significant lower rates of bystander CPR in Houston. Fig. 1B, C and D show the location of the primary cluster after each adjustment along with the location specific (block group) relative risks. The most likely cluster is the geographically larger area covering much of the eastern portion of Houston, with a relative risk of 0.62 (p < 0.001). The second most likely cluster is a smaller area in the northern portion of Houston city, with a relative risk of 0.55 (p < 0.037). Once individual-level patient characteristics are adjusted for (Fig. 1B), only one cluster is identified which encompasses a small localized area in north Houston, with a relative risk of 0.34 (p < 0.027). This cluster persists even after controlling for neighborhood-level characteristics (Fig. 1C and D). The decrease in relative risk associated with each adjustment to the underlying model demonstrates that the primary cluster is not due to the underlying spatial distribution of OHCA or covariates. There is some other risk factor not accounted for that is contributing to the cluster.
Table 3.
Cluster analysis of bystander CPR events, Houston, TX.
| Radius | # Block groups in cluster | # BCPR cases expected | # BCPR cases observed | RR | p-Value | |
|---|---|---|---|---|---|---|
| Map A: unadjusted analysis | ||||||
| Primary cluster | 17.2 km | 360 | 311.5 | 229 | 0.62 | <0.0001 |
| Secondary cluster | 7.7 km | 112 | 93.8 | 55 | 0.55 | 0.037 |
| Map B: adjusted analysisa | ||||||
| Primary cluster | 4.2 km | 52 | 37.5 | 13 | 0.34 | 0.027 |
| Map C: adjusted analysisb | ||||||
| Primary cluster | 4.1 km | 52 | 37.4 | 13 | 0.34 | 0.034 |
| Map D: adjusted analysisc | ||||||
| Primary cluster | 4.2 km | 52 | 36.6 | 13 | 0.34 | 0.046 |
Note: The primary cluster for each analysis is presented regardless of whether the p-value is statistically significant. Only secondary clusters with p < 0.05 are included.
Adjusted for age, sex, race, witnessed, public vs. private.
Adjusted for age, sex, race, witnessed, public vs. private, and census block percent white population.
Adjusted for age, sex, race, witnessed, public vs. private, and census block median household income.
Fig. 1.
Location of unadjusted (A), individually-adjusted (B) and neighborhood-adjusted (C and D) spatial clusters of bystander CPR for OHCA, Houston, TX. The approximate boundaries of the cluster, which include the census block groups included within the circular window, are shown in red dotted circles. The red/blue coloring indicates the block group specific relative risks. Changes in the relative risk occur when the expected counts of bystander CPR events are adjusted for individual (2B) and neighborhood (2C and D) risk factors. (For interpretation of the references to color in this sentence, the reader is referred to the web version of the article.)
3.2. Austin
Of 1043 eligible OHCA events in Travis County, 417 (39.9%) patients received bystander CPR. The patient and neighborhood level characteristics of the eligible arrests are displayed in Table 1. The hierarchical logistic regression models (Table 2) indicate that the individual-level characteristics of age, sex and race/ethnicity did not impact the odds of receiving bystander CPR in Austin. The location of the arrest, however, both whether it was witnessed (OR 1.63; 95% CI 1.21–2.19) and occurred in a public location (OR 2.20; 95% CI 2.44–9.59), significantly increased the odds of receiving bystander CPR. Results in Table 2 also indicate that arrest victims in higher-income Austin neighborhoods (OR 1.01; 95% CI 1.01–1.02) and predominantly white neighborhoods (OR 1.65; 95% CI 1.12–2.42) were more likely to receive bystander CPR.
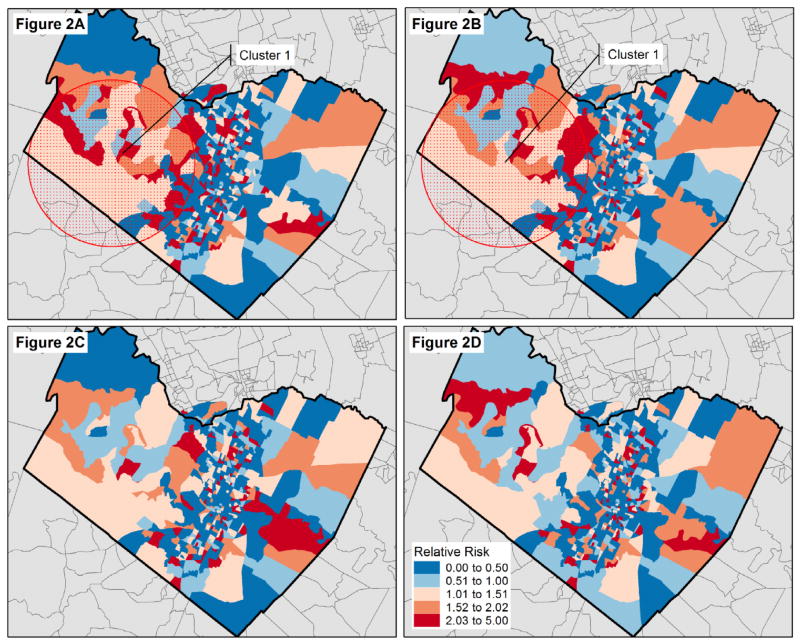
Table 3 and Fig. 2A identify one cluster with borderline statistically significant higher rate of bystander CPR in Austin. The cluster is located to the west of downtown Austin in a more affluent suburban part of the city, with a relative risk (RR) of 1.75 (p = 0.07). After adjusting for individual-level covariates (Fig. 2B), the p-value for the cluster increases (p = 0.11), and after adjusting of neighborhood-level median household income and percent white, the cluster disappears entirely (Fig. 2C and D). The inability to identify any statistically significant cluster after adjustment implies that the higher rates of BCPR identified in the unadjusted analysis are due to the underlying spatial distribution of individual-level and neighborhood-level covariates (Table 4).
Fig. 2.
Location of unadjusted (A), individually-adjusted (B) and neighborhood-adjusted (C and D) spatial clusters of bystander CPR for OHCA, Austin-Travis County, TX. The approximate boundaries of the cluster, which include the census block groups included within the circular window, are shown in red dotted circles. The red/blue coloring indicates the block group specific relative risks. Changes in the relative risk occur when the expected counts of bystander CPR events are adjusted for individual (3B) and neighborhood (3C and D) risk factors. (For interpretation of the references to color in this sentence, the reader is referred to the web version of the article.)
Table 4.
Cluster analysis of bystander CPR events, Austin-Travis County, TX.
| Radius | # Block groups in cluster | # BCPR cases expected | # BCPR cases observed | RR | p-Value | |
|---|---|---|---|---|---|---|
| Map A: unadjusted analysis | ||||||
| Primary cluster | 23.8 km | 37 | 51.2 | 82 | 1.75 | 0.070 |
| Map B: adjusted analysisa | ||||||
| Primary cluster | 23.8 km | 37 | 52.2 | 82 | 1.71 | 0.110 |
| Map C: adjusted analysisb | ||||||
| Primary cluster | <1 km | 1 | 5.16 | 0 | 0 | 0.960 |
| Map D: adjusted analysisc | ||||||
| Primary cluster | <1 km | 1 | 5.21 | 0 | 0 | 0.910 |
Note: The primary cluster for each analysis is presented regardless of whether the p-value is statistically significant. Only secondary clusters with p < 0.05 are included.
Adjusted for age, sex, race, witnessed, public vs. private.
Adjusted for age, sex, race, witnessed, public vs. private, and census block percent white population.
Adjusted for age, sex, race, witnessed, public vs. private, and census block median household income.
4. Discussion
This geographic analysis provides information on both the individual- and neighborhood-level factors that affect bystander CPR rates. Our initial unadjusted analysis found two statistically significant clusters of bystander CPR in Houston and one borderline statistically significant cluster in Austin. Individual patient characteristics change this picture dramatically, but do not “explain away” all geographic variation, especially in Houston. For example, black race is an important risk factor for not receiving bystander CPR in Houston (as shown by the HLM results) therefore it is reasonable to speculate that area differences in the proportion of African-Americans in the case population may have accounted for some of the clustering in Fig. 1A. Once race is adjusted for, the large cluster to the east, which encompasses a predominantly African-American area of the city, is no longer statistically significant. Public health officials could use this information to target CPR interventions among African-American individuals in this area of the city.
Figs. 1C, D and 2C, D show the impact of further adjustment for neighborhood-level race and income characteristics. For Austin, the cluster entirely disappears but in Houston one cluster persists. These findings suggest that not only do rates of bystander CPR and OHCA differ across these two cities, but the individual- and neighborhood-level characteristics that influence bystander CPR also differ across cities. In Austin, this information could be used to target specific neighborhoods for intervention since these factors appear to affect the clustering of bystander CPR in the city.
Our results support prior research that has found that low-income neighborhoods have markedly lower rates of bystander CPR than high-income neighborhoods.11,14 However, this is the first study to explicitly examine the geographic location of areas with low and high rates of bystander CPR. The ability to pinpoint geographic regions of a city with low bystander CPR rates, and understanding the underlying socioeconomic characteristics that drive those rates, has important implications for CPR and OHCA survival. Targeted CPR training to localized areas of low bystander CPR may be an evidence-based approach for public health planning.
We were able to find both high and low clusters of bystander CPR in our study. Although most efforts have been targeted at those neighborhoods which are doing poorly, it is also possible to more closely examine why certain neighborhoods are doing better than expected at providing bystander CPR. This idea of “positive deviance” has been used to identify successful strategies for reducing door-to-balloon time initiatives for myocardial infarction,29,30 but could also be explored for neighborhoods that are successfully increasing bystander CPR in their own communities. Further research will need to be conducted in Austin to determine what factors or strategies may be leading to this significant high cluster of cardiac arrest victims receiving bystander CPR.
There may be several explanations for our results which show a correlation between neighborhood characteristics and likelihood of not receiving bystander CPR. This may include, a lack of CPR training classes in low-income areas, a relative lack of social capital31,32 (distrust of neighbors, social isolation), and perhaps fear of acquiring a communicable disease from mouth-to-mouth ventilation (perceived as a higher probability in low-income areas).17,18 Neighborhood factors undoubtedly pay a role in determining the provision of bystander CPR and may be important targets for focused community-based educational interventions and improving OHCA survival.5,11 In addition, rather that widely blanketing a city with CPR training, which can be difficult and costly, a targeted, tailored approach in neighborhoods or areas considered “high risk” may be more efficient. It is important to note that individual-level characteristics were important in determining the location of clusters of bystander CPR in Austin and Houston. This suggests that both neighborhood-level and individual-level characteristics should be considered when developing and targeting intervention. The difference in importance of individual vs. neighborhood characteristics between Austin and Houston also suggests that a “one size fits all” approach to the implementation of CPR interventions may be ineffective, since different geographic areas had different underlying reasons for spatial patterns of bystander CPR.
There are several important limitations to our study. First, we cannot say that the whole population living within the cluster area is at the same “risk” of bystander CPR. There are various reasons why an individual experiencing OHCA may receive bystander CPR, which depends on their individual characteristics and behaviors, and the behaviors of family and friends. However, the presence of clusters of bystander CPR, which disappear when neighborhood-level socioeconomic factors are controlled for, suggests that neighborhood environment is an added risk factor that should be considered. Second, there are a number of unmeasured confounders that may impact the variation in CPR performance across the city which we could not measure include: large-scale public education campaigns for CPR, funding of EMS system, and variations in neighborhood cohesiveness or collective efficacy. Finally, we chose to use census block group as a proxy for neighborhood. This methodology has been validated as a feasible and acceptable alternative approach to examining the contextual effects of neighborhood on health outcomes.33,34 At the same time, using census block group data, which records the characteristics of the people living in that area, may not match the characteristics of the people who work in this area. This could potentially affect OHCAs that occur during work hours, when an individual is away from their home.
5. Conclusions
Despite large-scale educational and public health campaigns to train the public to perform bystander CPR, marked racial/ethnic and economic differences in bystander CPR performance still exist across the U.S. Our results indicate that these disparities even exist within cities, with specific localized geographic areas in both Houston and Austin experiencing high and low rates of bystander CPR. Public health efforts, which target CPR training to specific geographic neighborhoods and are tailored to specific individual and neighborhood population characteristics, may help reduce existing disparities in the provision of bystander CPR for out-of-hospital cardiac arrest.
Supplementary Material
Acknowledgments
The Cardiac Arrest Registry to Enhance Survival was funded by a cooperative agreement (U18 PS000314) from the CDC and Emory University School of Medicine. Dr. Sasson is supported by a career development grant from the Emergency Medicine Foundation and the American Heart Association. From the Centers for Disease Control and Prevention, we would like to thank Efomo Woghiren, BSc for her assistance with geocoding and Amy Valderrama, PhD and Robert Merritt, MA for their assistance with data collection and manuscript review. We would also like to acknowledge Rachel Robb, Kimberly Vallano, Monica Mehta and Amanda Bray-Perez for their assistance with data collection. Finally, we would like to thank the CARES Surveillance Group for their data collection and continued quality improvement efforts: Mike Levy, MD (Anchorage, AK); Joseph Barger, MD (Contra Costa County, CA); James V. Dunford, MD (San Diego County, CA); Karl Sporer, MD (San Francisco County, CA); Angelo Salvucci, MD (Ventura County, CA); David Ross, MD (Colorado Springs, CO); Christopher Colwell, MD CO); Dorothy Turnbull, MD (Stamford, CT); Rob Rosenbaum, MD (New Castle County, DE); Kathleen Schrank, MD (Miami, FL); Mark Waterman, MD (Atlanta, GA); Richard Dukes, MD (Clayton County, GA); Raymond Fowler, MD (Douglas County, GA); John Lloyd, MD (Forest Park, GA); Art Yancey, MD (Atlanta, GA); Earl Grubbs, MD (Gwinnett County, GA); John Lloyd, MD (Hapeville, GA); Johnathan Morris, MD (Metro Atlanta, GA); Stephen Boyle, MD (Metro Atlanta, GA); Troy Johnson, MD (Newton County, GA); Christopher Wizner, MD (Puckett County, GA); Melissa White, MD (Metro Atlanta, GA); Sabina Braithwaite, MD (Sedgwick County, KS); Sophia Dyer, MD (Boston, MS); Gary Setnik, MD (Cambridge, MS); Bob Hassett, MD (Springfield, MS); John Santor, MD (Springfield, MS); Bob Swor, MD (Oakland County, MI); Todd Chassee, MD (Kent County, MI); Charlie Lick, MD (Hennepin County, MN); Mike Parrish (Hennepin County, MN); Darel Radde (Hennepin County, MN); Brian Mahoney, MD (Hennepin County, MN); Darell Todd (Hennepin County, MN); Joseph Salomone, MD (Kansas City, MO); Eric Ossman, MD (Durham, NC); Brent Myers, MD (Wake County, NC); Lee Garvey, MD (Charlotte, NC); James Camerson, MD (New Jersey); David Slattery, MD (Las Vegas, NV); Joseph Ryan, MD (Reno, NV); Jason McMullan, MD (Cincinnati, OH); David Keseg, MD (Columbus, OH); James Leaming, MD (Hershey, PA); BK Sherwood, MD (Hilton Head, SC); Jeff Luther, MD (Sioux Falls, SD); Corey Slovis, MD (Nashville, TN); Paul Hinchey, MD (Austin-Travis County, TX); Michael Harrington, MD (Baytown, TX); John Griswell, MD and Jeff Beeson, MD (Fort Worth, TX); David Persse, MD (Houston, TX); Mark Gamber, MD (Plano, TX); and Joe Ornato, MD (Richmond, VA).
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.resuscitation.2013.01.007.
Footnotes
A Spanish translated version of the abstract of this article appears as Appendix in the final online version at http://dx.doi.org/10.1016/j.resuscitation.2013.01.007.
Conflict of interest statement
There are no conflicts of interest.
References
- 1.Cudnik MT, Schmicker RH, Vaillancourt C, et al. A geospatial assessment of transport distance and survival to discharge in out of hospital cardiac arrest patients: implications for resuscitation centers. Resuscitation. 2010;81:518–23. doi: 10.1016/j.resuscitation.2009.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ong ME, Chiam TF, Ng FS, et al. Reducing ambulance response times using geospatial-time analysis of ambulance deployment. Acad Emerg Med. 2010;17:951–7. doi: 10.1111/j.1553-2712.2010.00860.x. [DOI] [PubMed] [Google Scholar]
- 3.Ott WE. GIS in EMS. JEMS. 2003;28:89–91. [PubMed] [Google Scholar]
- 4.Peleg K, Pliskin JS. A geographic information system simulation model of EMS: reducing ambulance response time. Am J Emerg Med. 2004;22:164–70. doi: 10.1016/j.ajem.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Sasson C, Keirns CC, Smith D, et al. Small area variations in out-of-hospital cardiac arrest: does the neighborhood matter? Ann Intern Med. 2010;153:19–22. doi: 10.1059/0003-4819-153-1-201007060-00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yasunaga H, Miyata H, Horiguchi H, et al. Population density, call-response interval, and survival of out-of-hospital cardiac arrest. Int J Health Geogr. 2011;10:26. doi: 10.1186/1476-072X-10-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunne RB, Compton S, Zalenski RJ, Swor R, Welch R, Bock BF. Outcomes from out-of-hospital cardiac arrest in Detroit. Resuscitation. 2007;72:59–65. doi: 10.1016/j.resuscitation.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 8.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brookoff D, Kellermann AL, Hackman BB, Somes G, Dobyns P. Do blacks get bystander cardiopulmonary resuscitation as often as whites? Ann Emerg Med. 1994;24:1147–50. doi: 10.1016/s0196-0644(94)70246-2. [DOI] [PubMed] [Google Scholar]
- 10.Becker LB, Han BH, Meyer PM, et al. Racial differences in the incidence of cardiac arrest and subsequent survival. The CPR Chicago Project. N Engl J Med. 1993;329:600–6. doi: 10.1056/NEJM199308263290902. [DOI] [PubMed] [Google Scholar]
- 11.Sasson C, Keirns CC, Smith DM, et al. Examining the contextual effects of neighborhood on out-of-hospital cardiac arrest and the provision of bystander cardiopulmonary resuscitation. Resuscitation. 2011;82:674–9. doi: 10.1016/j.resuscitation.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vaillancourt C, Lui A, De Maio VJ, Wells GA, Stiell IG. Socioeconomic status influences bystander CPR and survival rates for out-of-hospital cardiac arrest victims. Resuscitation. 2008;79:417–23. doi: 10.1016/j.resuscitation.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 13.Feero S, Hedges JR, Stevens P. Demographics of cardiac arrest: association with residence in a low-income area. Acad Emerg Med. 1995;2:11–6. doi: 10.1111/j.1553-2712.1995.tb03071.x. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell MJ, Stubbs BA, Eisenberg MS. Socioeconomic status is associated with provision of bystander cardiopulmonary resuscitation. Prehosp Emerg Care. 2009;13:478–86. doi: 10.1080/10903120903144833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Swor R, Khan I, Domeier R, Honeycutt L, Chu K, Compton S. CPR training and CPR performance: do CPR-trained bystanders perform CPR? Acad Emerg Med. 2006;13:596–601. doi: 10.1197/j.aem.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 16.Vaillancourt C, Stiell IG, Wells GA. Understanding and improving low bystander CPR rates: a systematic review of the literature. CJEM. 2008;10:51–65. doi: 10.1017/s1481803500010010. [DOI] [PubMed] [Google Scholar]
- 17.Bradley SM, Rea TD. Improving bystander cardiopulmonary resuscitation. Curr Opin Crit Care. 2011;17:219–24. doi: 10.1097/MCC.0b013e32834697d8. [DOI] [PubMed] [Google Scholar]
- 18.Taniguchi T, Sato K, Fujita T, Okajima M, Takamura M. Attitudes to bystander cardiopulmonary resuscitation in Japan in 2010. Circ J. 2012;76:1130–5. doi: 10.1253/circj.cj-11-0054. [DOI] [PubMed] [Google Scholar]
- 19.Cho GC, Sohn YD, Kang KH, et al. The effect of basic life support education on laypersons’ willingness in performing bystander hands only cardiopulmonary resuscitation. Resuscitation. 2010;81:691–4. doi: 10.1016/j.resuscitation.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 20.Lester CA, Donnelly PD, Assar D. Lay CPR trainees: retraining, confidence and willingness to attempt resuscitation 4 years after training. Resuscitation. 2000;45:77–82. doi: 10.1016/s0300-9572(00)00170-2. [DOI] [PubMed] [Google Scholar]
- 21.Lynch B, Einspruch EL. With or without an instructor, brief exposure to CPR training produces significant attitude change. Resuscitation. 2010;81:568–75. doi: 10.1016/j.resuscitation.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 22.Sipsma K, Stubbs BA, Plorde M. Training rates and willingness to perform CPR in King County, Washington: a community survey. Resuscitation. 2011;82:564–7. doi: 10.1016/j.resuscitation.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 23.Kulldorff M. A spatial scan statistic. Commun Stat: Theory Methods. 1997;26:1481. [Google Scholar]
- 24.McNally B, Stokes A, Crouch A, Kellermann AL CS Group. CARES: Cardiac Arrest Registry to Enhance Survival. Ann Emerg Med. 2009;54:674–83. e2. doi: 10.1016/j.annemergmed.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 25.McNally B, Robb R, Mehta M, et al. Out-of-Hospital Cardiac Arrest Surveillance – Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005–December 31, 2010. MMWR Surveill Summ. 2011;60:1–19. [PubMed] [Google Scholar]
- 26.Bureau USC. 2000 Census Summary File 3. Suitland, MD: U.S. Census Bureau; 2000. [Google Scholar]
- 27.Kulldorff M, Nagarwalla N. Spatial disease clusters: detection and inference. Stat Med. 1995;14:799. doi: 10.1002/sim.4780140809. [DOI] [PubMed] [Google Scholar]
- 28.Kulldorff M. Information Management Services I. In: Kulldorff M, editor. SaTScan v7.0: Software for the spatial and space–time scan statistics. 7.0. Boston, MA: Information Management Services Inc; 2006. [Google Scholar]
- 29.Bradley EH, Curry LA, Ramanadhan S, Rowe L, Nembhard IM, Krumholz HM. Research in action: using positive deviance to improve quality of health care. Implement Sci. 2009;4:25. doi: 10.1186/1748-5908-4-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krumholz HM, Curry LA, Bradley EH. Survival after acute myocardial infarction (SAMI) study: the design and implementation of a positive deviance study. Am Heart J. 2011;162:981–7. e9. doi: 10.1016/j.ahj.2011.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berkman L. Role of social-relations in health promotion. Psychosom Med. 1995:245–54. doi: 10.1097/00006842-199505000-00006. [DOI] [PubMed] [Google Scholar]
- 32.McCarthy M. Social determinants and inequalities in urban health. Rev Environ Health. 2000;15:97–108. doi: 10.1515/reveh.2000.15.1-2.97. [DOI] [PubMed] [Google Scholar]
- 33.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of U.S. socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156:471–82. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 34.Krieger N, Zierler S, Hogan JW, et al. Neighborhoods and health. Geocoding and measurement of neighborhood socioeconomic position: a US perspective. NY: Oxford Press; 2003. pp. 147–78. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.