Abstract
A tattoo is defined as the intentional or accidental deposit of pigment into the skin. The phenomenon of skin tattooing is on the rise worldwide and complications of tattooing are increasingly being recognised in diagnostic and clinical medicine. We describe a case of calcification-like changes on mammography resembling that of breast malignancy as a result of tattoo pigment deposition in an axillary lymph node. Recognition of such changes in routine breast screening is crucial to avoid further unnecessary invasive investigations and surgery in such patients.
Background
A tattoo is defined as the intentional or accidental deposit of pigment into the skin.1 The phenomenon of skin tattooing is on the rise worldwide, but the exact prevalence is unknown. One survey carried out in 1998 showed that approximately 10% of adult Australians had tattoos.2 Complications of tattooing are increasingly being recognised; however, there is still a notable paucity of literature on the subject in medical journals.
Case presentation
A 47-year-old asymptomatic woman presented to BreastScreen Queensland, Australia, for routine mammography. No prior films were available for comparison. The client had no significant family history and was not on hormone replacement therapy.
Investigations
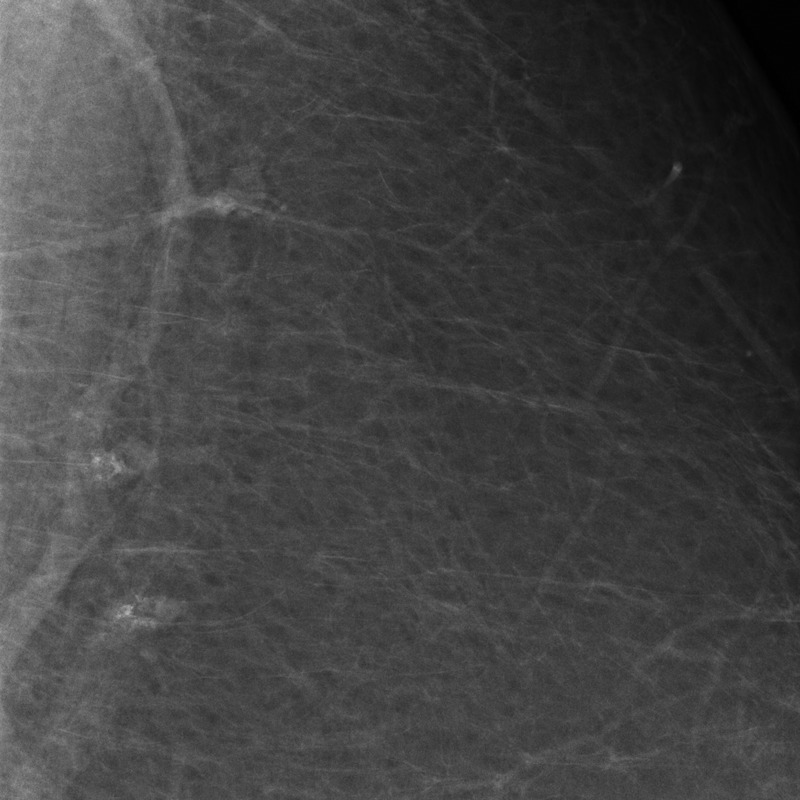
A standard four view screening mammogram was performed and the mediolateral oblique (MLO) view (figure 1) showed two left lateral soft tissue densities measuring approximately 1.0×0.5 cm closely related to the superior pectoralis major. The densities were not identified on ultrasound scan and the changes were interpreted as pleomorphic foci of calcification (figure 2).
Figure 1.

Lateral medial oblique view of the left breast showing two foci of radiopacity (arrow) resembling coarse calcification.
Figure 2.
High-power view of the two radiopacities.
An 18 gauge stereotactic guided core biopsy was performed, as there was concern for breast malignancy given the nature of the densities and apparent pleomorphic calcification. The apparent calcification was evident in the core biopsy specimen radiograph (figure 3).
Figure 3.
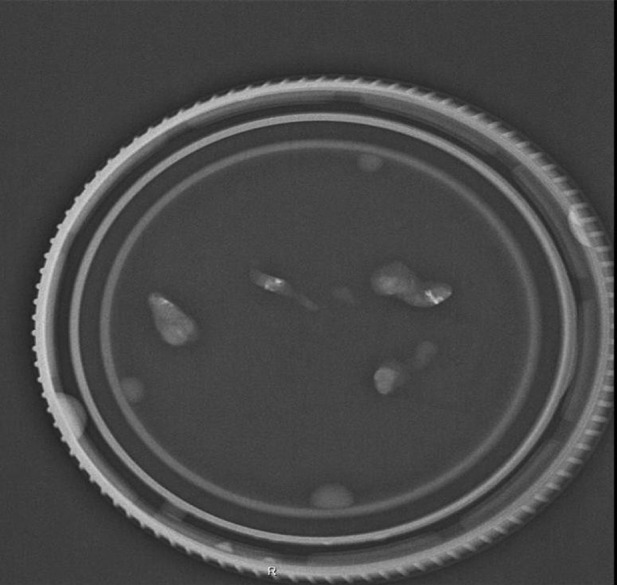
Radiograph of the breast tissue cores showing foci of radiopacity resembling coarse calcification in two core tissue fragments.
The histological sections showed a reactive, benign lymph node with black pigment in the nodal sinuses and macrophages (figure 4). No true calcification was present and there was no neoplasia (figure 5). Special stains for melanin, haemosiderin, iron and calcium were negative. A negative pan-cytokeratin (AE1/AE3) confirmed the absence of epithelial cells in the lymph node. In addition, serial sections through the block were non-contributory. A diagnosis of intranodal carbon pigment secondary to skin tattooing was made.
Figure 4.
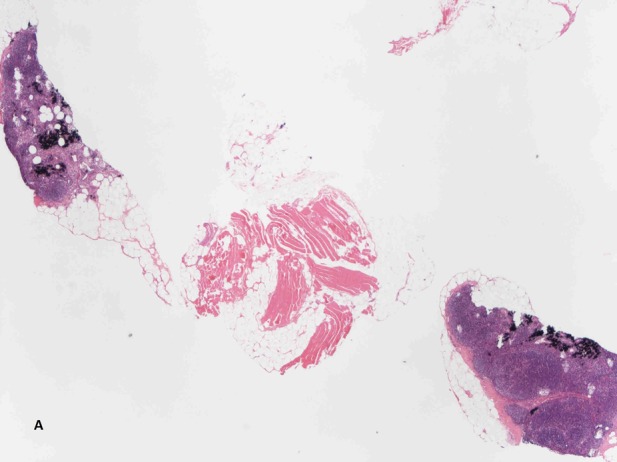
Low-power photomicrograph showing two foci of dark tattoo pigment in lymph node tissue.
Figure 5.
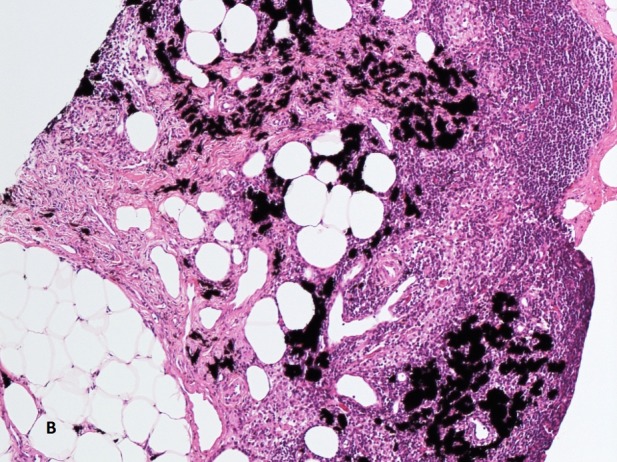
High-power photomicrograph showing dark tattoo pigment particles in nodal sinuses and macrophages.
Outcome and follow-up
Further patient history was sought and it was confirmed that the patient had a decade-old tattoo on the skin of her mid-back (figure 6). Black, blue and other, now faded, dark inks had been used.
Figure 6.

Long-standing lower back midline tattoo of the patient consisting predominantly of black, grey and blue colours.
Similar radiographic changes were reported on subsequent mammography at follow-up and the patient is free of malignant breast disease a year after the initial presentation.
Discussion
Tattoo ink is composed of two ingredients: a dye which is often a heavy metal-containing compound and a solvent. The solvents often used are either water-based, alcohols or glycols. Iron oxides and carbon are often used for black colour. For other colours, the following are commonly in use: mercury sulphide for red, cobalt aluminate for blue, cadmium sulphide for yellow and chromium oxide for green.3 Since there is no regulation in the use of tattoo inks anywhere in the western world, the exact ingredients of tattoo ink are highly variable and can never be known precisely in most cases. Our patient had a fading black tattoo on her back. Ninety-one per cent of posterior trunk lymphatic drainage goes to the axillae4 and tattoo pigment is carried by activated macrophages from the skin dermis to the regional nodes.
To the best of our knowledge, this is the first case report of tattoo pigment mimicking breast carcinoma on imaging confirmed by histology. Honegger et al5 described one case of tattoo pigment mimicking nodal calcification which was diagnosed by fine needle aspiration cytology of the axillary lymph node, but a core biopsy was not performed.
It is not always possible to differentiate intranodal tattoo pigment from calcification associated with sinister breast pathology on radiographic examination alone.6 In our case, the intranodal tattoo pigment had a pleomorphic appearance with associated densities. It is likely that the radiographic appearances may vary with the heavy metal composition of the tattoo inks present. Microcalcification is typical of metastatic breast cancer to axillary lymph nodes.7
The differential diagnosis of axillary nodal calcification and calcific type densities also include fat necrosis8 and coarse calcification seen in granulomatous diseases such as tuberculosis, sarcoidosis and post-BCG vaccination.9 Amorphous or punctate densities resembling calcification have been described in lymph nodes of patients with rheumatoid arthritis treated with gold injections.10 Silicone gel particles from microscopic breast implants leakage typically manifest as a ‘snowstorm’ appearance on mammography.11
Macroscopically, lymph nodes involved by tattoo pigment are often normal in size and texture and of variable colour. The non-polarisable, dark coarse granules are often seen in subcapsular and sinusoidal histiocytes on light microscopy. Nodal architecture is always preserved.12 The pigment is resistant to melanin bleach and does not stain with Masson stain, unlike melanin.13 Stains for iron and calcium are variably positive depending on the composition of the tattoo ink. Carbon is an inert compound which does not have a positive marker in routine use. Immunohistochemical markers for melanocytic differentiation may be useful in distinguishing intranodal tattoo pigment (negative) from nodal naevus rests and metastatic melanoma (positive). Nodal pigmentation, as in our case, can manifest clinically several years to decades after tattoo application. It may also show on radiological and histopathological examinations years after the tattoo has been removed making a diligent clinical examination and history taking pivotal in clinching the diagnosis.14
Tattoo ink can mimic sinister pathology elsewhere and cause similar diagnostic difficulty if it is not recognised. For example, several cases of tattoo ink mimicking melanin pigment in sentinel node biopsies performed for malignant melanoma have been described.12 Tattoo pigment can also cause false positive marker uptake in positron emission tomography scan15 and iron oxide containing inks have been reported to elicit a tingling or burning sensation in the skin on MRI scanning.16
In conclusion, cosmetic tattooing is on the increase and tattoo pigment should be recognised as a cause of axillary nodal changes on radiology that can mimic metastatic breast carcinoma. Recognition of this phenomenon in breast screening is crucial to avoid unnecessary invasive investigations and surgery.
Learning points.
The phenomenon of skin tattooing is on the rise worldwide and is not without medical complications in a small proportion of people. Medical practitioners need to acquaint themselves with the various pathologies associated with the practice.
Most tattoo inks are composed of heavy metal compounds in one or more solvents.
There are no clearly defined regulations on the use of inks in the tattoo industry in most countries resulting in high variability in the composition of tattoo inks on the market.
Tattoo pigment in lymph nodes may show as coarse calcification on mammography which may be misinterpreted as a sign of metastatic disease.
Acknowledgments
The authors would like to thank Associate Professor Jane Armes of Mater Pathology, South Brisbane for peer review of the manuscript.
Footnotes
Contributors: AM was originator of the paper, did the literature review, writing of the manuscript, applied for ethics approval, prepared histology photomicrographs and obtained the patient's tattoo photo. BS signed out the case, supervised AM and contributed the histopathological information and description. JMG reported the mammographs and researched on the differential diagnosis of breast related calcifications. CRG prepared radiological images, provided clinical history and obtained patient consent.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Cruz FA, Lage D, Frigerio RM, et al. Reactions to the different pigments in tattoos: a report of two cases. An Bras Dermatol 2010;2013:708–11 [DOI] [PubMed] [Google Scholar]
- 2.Makkai T, McAllister I. Prevalence of tattooing and body piercing in the Australian community. Commun Dis Intell 2001;2013:67–72 [DOI] [PubMed] [Google Scholar]
- 3.Timko AL, Miller CH, Johnson FB, et al. In vitro quantitative chemical analysis of tattoo pigments. Arch Dermatol 2001;2013:143–7 [PubMed] [Google Scholar]
- 4.Uren RF, Howman-Giles R, Thompson JF. Patterns of lymphatic drainage from the skin in patients with melanoma. J Nucl Med 2003;2013:570–82 [PubMed] [Google Scholar]
- 5.Honegger MM, Hesseltine SM, Gross JD, et al. Tattoo pigment mimicking axillary lymph node calcifications on mammography. AJR Am J Roentgenol 2004;2013:831–2 [DOI] [PubMed] [Google Scholar]
- 6.Brown RC, Zuehlke RL, Ehrhardt JC, et al. Tattoos simulating calcifications on xeroradiographs of the breast. Radiology 1981;2013:583–4 [DOI] [PubMed] [Google Scholar]
- 7.Gorkem SB, O'Connell AM. Abnormal axillary lymph nodes on negative mammograms: causes other than breast cancer. Diagn Interv Radiol 2012;2013:473–9 [DOI] [PubMed] [Google Scholar]
- 8.Hooley R, Lee C, Tocino I, et al. Calcifications in axillary lymph nodes caused by fat necrosis. AJR Am J Roentgenol 1996;2013:627–8 [DOI] [PubMed] [Google Scholar]
- 9.Burdeny DA, Reed MH, Ferguson CA. Calcification of axillary lymph nodes following BCG vaccination. Can Assoc Radiol J 1989;2013:92–3 [PubMed] [Google Scholar]
- 10.Bruwer A, Nelson GW, Spark RP. Punctate intranodal gold deposits simulating microcalcifications on mammograms. Radiology 1987;2013:87–8 [DOI] [PubMed] [Google Scholar]
- 11.Scaranelo AM, Marques AF, Smialowski EB, et al. Evaluation of the rupture of silicone breast implants by mammography, ultrasonography and magnetic resonance imaging in asymptomatic patients: correlation with surgical findings. Sao Paulo Med J 2004;2013:41–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peterson SL, Lee LA, Ozer K, et al. Tattoo pigment interpreted as lymph node metastasis in a case of subungual melanoma. Hand 2008;2013:282–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shinohara MM, Nguyen J, Gardner J, et al. The histopathologic spectrum of decorative tattoo complications. J Cutan Pathol 2012;2013:1110–18 [DOI] [PubMed] [Google Scholar]
- 14.Tehrani H, Lamberty BGH. Axillary lymphadenopathy secondary to tattoo pigment and silicone migration. J Plast Reconstr Aesthet Surg 2008;2013:1381. [DOI] [PubMed] [Google Scholar]
- 15.Nam H, Smith S, Laing R. A pitfall of 18-fluorodeoxyglucose-PET in a patient with a tattoo. Lancet Oncol 2007;2013:1147–8 [DOI] [PubMed] [Google Scholar]
- 16.Offret H, Offret M, Labetoulle M, et al. [Permanent cosmetics and magnetic resonance imaging]. J Fr Ophtalmol 2009;2013:4. [DOI] [PubMed] [Google Scholar]


