Abstract
In the present case a 30-year-old African American man was admitted with fever and chills secondary to two large hepatic abscesses diagnosed on an ultrasound. The patient was started on antibiotics after blood cultures were drawn. Initially the abscess was drained and showed dramatic improvement upon repeat imaging. The blood cultures revealed Gram-negative rods that were identified as Fusobacterium necrophorum. At that time the patient was switched to levofloxacin and metronidazole based on sensitivities. On this new antibiotic regime the patient improved dramatically. After just 5 days the patient was discharged home on oral antibiotics and was scheduled to follow-up in 1 week. In the present case we present a healthy 30-year-old man with no significant co-morbidities who developed a hepatic abscess from F necrophorum but successfully recovered after appropriate antibiotic treatment.
Background
Hepatic abscesses typically form when bacteria enter the liver through one of many routes: the portal circulation, the biliary tract or through haematogenous spread from a distant site of infection.1 This is important because pyogenic liver abscesses are the most common type of visceral abscess with an annual incidence estimated at 2.3 cases per 100 000 people, more frequently in men but why is not currently known.2 In a clinical context, fever, chills, nausea, vomiting and right upper quadrant pain are the most common presenting symptoms.3 While all of these symptoms are very non-specific they are more likely to raise the spectre of a problem of hepatic origin. As with numerous other conditions, diabetes mellitus and occult cancer dramatically increase the risk of abscess development while renal disease and pneumonia show a more modest increase in risk.4 From previous studies the enteric bacteria including Klebsiella species, Escherichia coli and Enterococcus are the major sources of pyogenic hepatic abscesses.3 Since the mortality rate due to this occurrence is 2–12%, appropriate antibiotic therapy along with percutaneous drainage is essential in alleviating symptoms and preventing death.3 5 6
Fusobacterium necrophorum is a non-motile, Gram-negative anaerobe that is normally found in the mouth, pharynx, gastrointestinal tract and urinary tract.7 8 Infection with this organism is seen primarily in males between 16 and 23 and commonly from January to March, though this is due to unknown reasons.9
In the present case we describe a man with numerous constitutional symptoms that was ultimately diagnosed with multiple hepatic abscesses on an ultrasound (US) as well as a CT caused by the rare organism F necrophorum. After aggressive drainage, early antibiotics and repeated imaging the patient's abscesses resolved without surgical intervention. Thus, in the case report that follows, we detail how even rare hepatic abscesses can be treated with medical management alone.
Case presentation
A 30-year-old African American man was admitted to our hospital after reporting fevers, chills, malaise, nausea, vomiting and diarrhoea for several days prior to admission. The patient's history was unremarkable. He is a Jehovah's Witness, who lives at home with his wife, and as a result will not accept any blood products because of his beliefs.
The patient is an obese, normotensive African American man with a fever of 38.3°C, tachycardia of 115 bpm, a respiratory rate of 43 breaths/min and had an oxygen saturation of 100% on 3 L of oxygen. He was alert and oriented in mild distress. The patient's eyes showed mild scleral icterus. The patient was also tachycardic with slight lower extremity oedema and a mildly distended abdomen without organomegaly. Laboratory tests on admission (table 1) revealed leucocytosis and an elevation in creatine. There was also a low level of total protein and albumin, with elevated levels of aspartate aminotransferase and alanine aminotransferase. Additionally, there was an elevated total bilirubin with a high direct fraction. A blood culture was obtained prior to the beginning of antibiotic therapy.
Table 1.
Laboratory findings on admission showing the increases in AST, ALT and bilirubin
| Blood |
Electrolytes and chemistries |
Urinalysis |
|||
|---|---|---|---|---|---|
| WCC | 22 800 | Na | 143 | Color | Yellow |
| Segs | K | 4.0 | Clarity | Slightly hazy | |
| Band | Cl | 112 | Glucose | Negative | |
| Mono | CO2 | 19 | Bilirubin | Negative | |
| Eos | BUN | 23 | Ketones | Trace | |
| Baso | Cr | 1.79 | Specific gravity | 1.011 | |
| Lym | Glucose | 88 | Blood | Large | |
| RBC | TP | 5.6 g/dL | pH | 5.5 | |
| Hgb | 11.8 | Alb | 2.9 g/dL | Protein | Trace |
| Hct | 35.6 | AST | 152 U/L | Urobilinogen | 1.0 EU/dL |
| Plt | 78 000 | ALT | 114 U/L | Nitrite | Negative |
| Alk Phos | 115 U/L | Leucocytes | Negative | ||
| T. Bili | 2.0 mg/dL | ||||
| D Bili | 1.5 mg/dL | ||||
| Phosphorus | 2.7 mg/dL | ||||
| Lactic acid | 1.8 mmol/L | ||||
| Magnesium | 1.6 mg/dL | ||||
Alb, albumin; Alk Phos, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; Band, band neutrophils; Baso, basophils; BUN, blood urea nitrogen; Cl, chloride; CO2, carbon dioxide; Cr, creatine; D Bili, direct bilirubin; Eos, eosinophilia; Hct, haematocrit; Hgb, haemoglobin; K, potassium; Lym, lymphocytes; Mono, monocytes; Na, sodium; Plt, platelet; RBC, red blood cell; Segs, segmental neutrophils; T. Bili, total bilirubin; TP, total protein; WCC, white cell count.
US showed hepatomegaly with two parenchymal masses noted within the right lobe of the liver as seen in figure 1. The first measured 4.7×4.3×3.9 cm and the second was 4.9×5.7×5.8 cm in diameter. A CT scan with contrast showed two large pyogenic hepatic abscesses with minimal enhancement as seen in figure 2. The abscess was drained under fluoroscopic guidance and a multipurpose drain was inserted. A sample of the drained fluid was cultured and the patient was started empirically on metronidazole and piperacillin/tazobactam.
Figure 1.
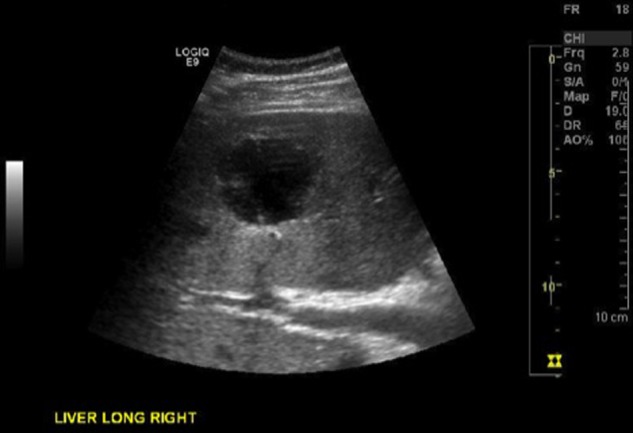
Ultrasound of liver showing a hyperechogenic region representing a large hepatic abscess.
Figure 2.
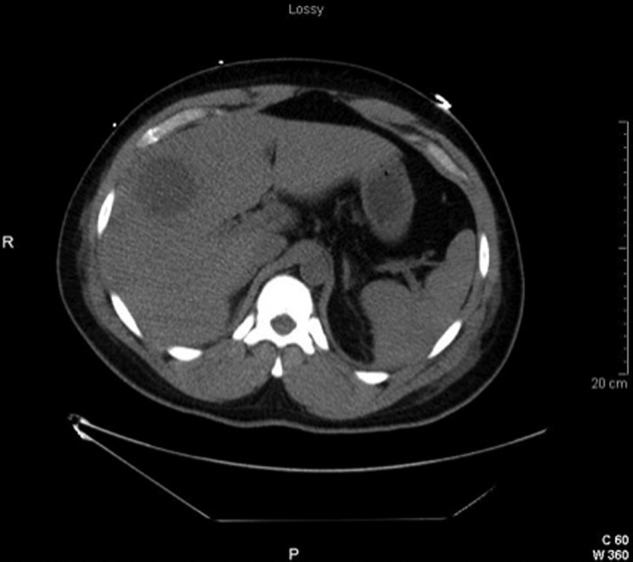
A CT scan of abdomen predrain insertion.
A repeat CT scan of the abdomen and pelvis with contrast 4 days later showed significant interval improvement of the drained abscess as seen in figure 3. The other abscess showed no significant change at that time. The blood cultures identified F necrophorum growth and as a result piperacillin/tazobactam was continued for four more days. At that time, levofloxacin 750 mg daily was started orally along with metronidazole 500 mg orally every 8 h based on the culture sensitivities that were returned. The patient reported that all of his symptoms continued to improve with treatment. The antibiotic course was to be continued until the abscesses resolved on repeat imaging.
Figure 3.

CT scan of the abdomen 2-week postdrain insertion and the resolution of the hepatic abscess.
Treatment
As stated previously, the patient was started on empiric antibiotics including piperacillin/tazobactam as well as metronidazole. These medications were indicated as the initial suspicion of an enteric organism causing the hepatic abscess that was seen on the US imaging. However, after the initial drainage cultures were drawn and the antibiotic therapy was altered to metronidazole and levofloxacin based on the sensitivities that were received from the culture analysis.
Outcome and follow-up
The patient was scheduled for follow-up as an outpatient in 1 week. The patient was then seen and the abscesses completely resolved after completing the antibiotics as an outpatient.
Discussion
Hepatic abscesses due to F necrophorum are extremely rare in humans. The development is usually secondary to spread through haematogenous dissemination or the portal circulation. In the present case it remains unknown how this infection began; however, it seems most likely that there was haematogenous spread of this organism through the portal vein, which is the most likely mechanism .1
Prompt diagnosis with aggressive antibiotic therapy is essential for hepatic abscesses caused by F necrophorum, since it can be potentially lethal.3 Generally, the larger the abscess is, the higher the risk of morbidity and mortality.10 In this case, definitive diagnosis was made by blood culture after both US and CT revealed the two hepatic abscesses.
The patient was placed on broad-spectrum antibiotic coverage including piperacillin/tazobactam and metronidazole upon admission on the suspicion of an abscess. After blood cultures confirmed F necrophorum as the causative agent, the patient was continued on metronidazole, and levofloxacin was added for enhanced coverage based on sensitivities. There is scant evidence for the treatment of F necrophorum at the present time; therefore, the choice of antibiotics was guided based on sensitivities alone. At the time of discharge the patient had nearly complete symptom resolution.
In summation, F necrophorum is a rare bacterium that can cause potentially fatal hepatic abscesses in people. This case demonstrates that it is critical to examine all patients with a clinical evaluation coupled with a high index of suspicion of infection or abscess development based on the physical examination as well as the related symptoms. Early laboratories, cultures and aggressive antibiotics are all critical to the effective medical management of this condition so that the patient can be treated effectively while avoiding the risks of surgery.
Learning points.
Fusobacterium necrophorum is a very rare organism that can cause hepatic abscesses in immunocompetent individuals.
Hepatic abscesses when treated early and aggressively with judicious choice of antibiotics can spare patients the risks of surgical drainage.
Clinical evaluation of patients with an appropriate index of suspicion for hepatic infections and early imaging are critical to effectively guide care before definitive diagnosis can be made.
Footnotes
Contributors: EF is the primary author of this manuscript and contributed to all phases of production. MKP, SS and CFK assisted in the writing, editing and final submission of the aforementioned manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Mohsen AH, Green ST, Read RC, et al. Liver abscess in adults: ten years experience in a UK centre. QJM 2002;2013:797–802 [DOI] [PubMed] [Google Scholar]
- 2.Kaplan GG, Gregson DB, Laupland KB. Population-based study of the epidemiology of and the risk factors for pyogenic liver abscess. Clin Gastroenterol Hepatol 2004;2013:1032–8 [DOI] [PubMed] [Google Scholar]
- 3.Rahimian J, Wilson T, Oram V, et al. Pyogenic liver abscess: recent trends in etiology and mortality. Clin Infect Dis 2004;2013:1654–9 [DOI] [PubMed] [Google Scholar]
- 4.Tsai F-C, Huang Y-T, Chang L-Y, et al. Pyogenic liver abscess as endemic disease, Taiwan. Emerg Infect Dis 2008;2013:1592–600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chuang HC, Chen TL, Chiang DH, et al. Clinical and bacteriological characteristics of pyogenic liver abscess in non-diabetic patients. J Microbiol Immunol Infect 2009;2013:385–92 [PubMed] [Google Scholar]
- 6.Yu SC, Ho SS, Lau WY, et al. Treatment of pyogenic liver abscess: prospective randomized comparison of catheter drainage and needle aspiration. Hepatology 2004;2013:932–8 [DOI] [PubMed] [Google Scholar]
- 7.Bennett KW, Eley A. Fusobacteria: new taxonomy and related diseases. J Med Microbiol 1993;2013:246–54 [DOI] [PubMed] [Google Scholar]
- 8.Brazier JS. Human infections with Fusobacterium necrophorum. Anaerobe 2006;2013:165–72 [DOI] [PubMed] [Google Scholar]
- 9.Brazier JS, Hall V, Yusuf E, et al. Fusobacterium necrophorum infections in England and Wales 1990–2000. J Med Microbiol 2002;2013:269–72 [DOI] [PubMed] [Google Scholar]
- 10.Yang CC, Yen CH, Ho MW, et al. Comparison of pyogenic liver abscess caused by non-Klebsiella pneumoniae and Klebsiella pneumoniae. J Microbiol Immunol Infect 2004;2013:176–84 [PubMed] [Google Scholar]


