Abstract
Extrapulmonary tuberculosis (EPTB) is common in HIV-infected patients, especially at lower CD4 cell counts, yet is often difficult to diagnose with certainty. A 35-year-old man presented with dyspnoea and constitutional symptoms of tuberculosis (TB). Laboratory investigations included a positive HIV test and a CD4 cell count of 138 cells/μL. Chest radiography revealed a globular-shaped heart and bilateral pleural effusions, while echocardiography confirmed a massive pericardial effusion. The new Xpert MTB/RIF (Xpert) assay detected rifampicin-sensitive Mycobacterium tuberculosis in pericardial as well as sputum samples. Smear of the pericardial sample was negative. The patient was started on anti-TB treatment and is presently well. He will initiate antiretroviral therapy after 4–6 weeks. To the best of our knowledge, this is the first case report of EPTB diagnosed on pericardial fluid using the Xpert assay in Africa. This report also summarises the use of this assay in the diagnosis of EPTB in HIV-associated TB.
Background
Sub-Saharan Africa carries the greatest proportion of new cases of tuberculosis (TB), with more than 260 cases per 100 000 population.1 In 2011, there were 1.4 million TB-related deaths worldwide, of which 430 000 (31%) were HIV associated.1 Although the new Xpert MTB/RIF (Xpert) assay has been validated specifically for diagnosis of pulmonary TB,2 extrapulmonary tuberculosis (EPTB) often poses a diagnostic challenge and is reported in up to 40% of HIV-infected patients with TB.3 Recently, the Xpert assay has shown potential to dramatically improve the rapid diagnosis of EPTB from a variety of non-sputum samples. We report a case of EPTB unexpectedly detected from a pericardial fluid sample using the Xpert assay.
Case presentation
A 35-year-old man presented to the emergency department with a 2-month history of progressive shortness of breath, productive cough and ankle swelling. He also reported with fever, night sweats, loss of weight and loss of appetite. He had no medical history of TB and had never been tested for HIV. After noticing the ankle swelling, he also consulted a local prophet who advised him to stand on a heated mixture of sand, coffee and salt.
The physical examination revealed tachycardia, bipedal oedema, generalised lymphadenopathy, raised jugular venous pressure and an impalpable apex beat. No pulsus paradoxus or arterial hypotension was observed. Auscultation revealed normal heart sounds and no pericardial friction rub. Breath sounds were reduced posterior over the lower zones of both lungs. Bilateral clean ulcers were also present on the soles of both feet. The remainder of the systemic examination was otherwise normal.
Investigations
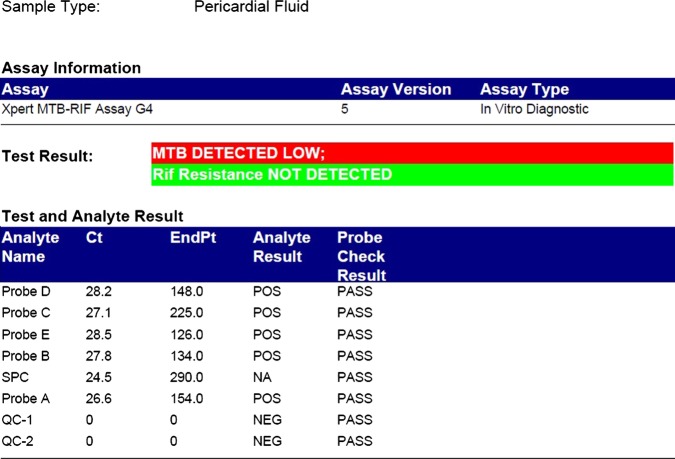
ECG showed sinus tachycardia and T-wave inversion in leads V3–V6. An enlarged, globular-shaped cardiac silhouette was present on chest X-ray as were bilateral pleural effusions (figure 1). Echocardiography revealed a massive pericardial effusion, measuring 4.46 cm posteriorly and 3 cm anteriorly. Consequently, emergency percutaneous ultrasound-guided pericardiocentesis was performed and an intrapericardial catheter inserted for continued drainage. Sputum, pericardial and pleural fluid samples were sent for analysis.
Figure 1.
A chest radiograph showing an enlarged, globular shaped heart and bilateral pleural effusions.
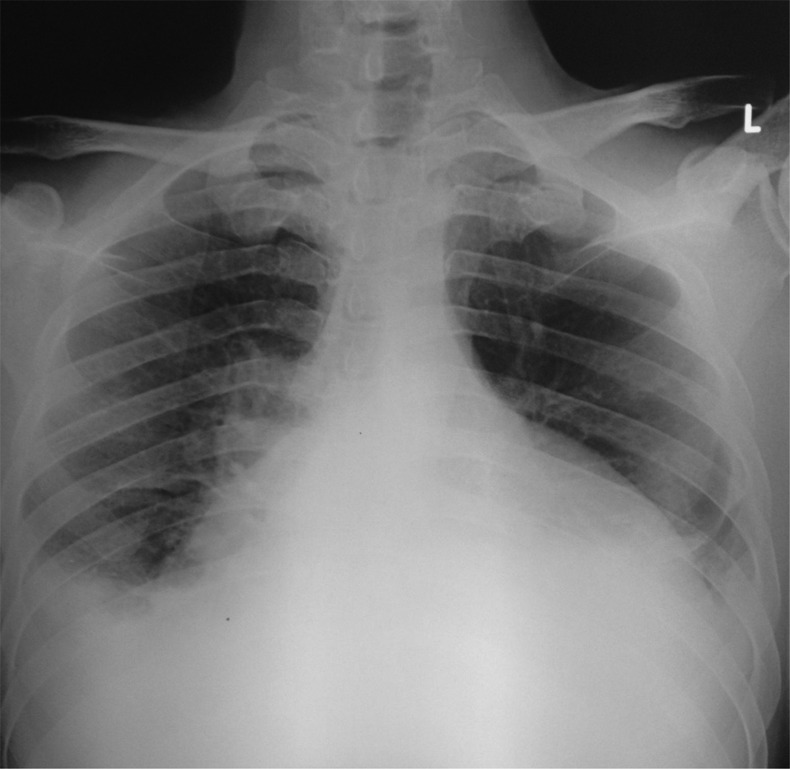
Initial laboratory results confirmed a positive HIV ELISA and CD4 count of 138 cells/μL. Pericardial as well as pleural fluid samples were negative for acid-fast bacilli (AFB). Both samples were exudates and showed high adenosine deaminase levels. The Xpert assay, however, detected rifampicin-sensitive TB in the pericardial sample and in the sputum (figure 2). A diagnosis was made of pulmonary and EPTB, with pericardial and possibly pleural involvement. In our setting, South Africa, the Xpert assay has completely replaced smear microscopy as the initial diagnostic test for pulmonary TB. As a result, smear microscopy was not performed on sputum. In addition, given that we are in a resource limited setting and that we already had a positive Xpert assay on sputum, we decided not to perform this test. Nevertheless, smear is still widely used for monitoring response to treatment in patients with pulmonary TB and for making the diagnosis of EPTB. The use of the Xpert assay in extrapulmonary samples is not presently included in the national laboratory's list of available diagnostic services. However, as part of a study into the use of the Xpert assay in EPTB, our hospital was able to process our pericardial sample at no added cost.
Figure 2.
Xpert MTB/Rif assay report showing a positive test for Mycobacterium tuberculosis and no rifampicin resistance. M tuberculosis is identified when two out of the five probes give a positive signal in one cycle.
Treatment
After emergency percutaneous pericardiocentesis, medical treatment with full anti-TB therapy was started. Corticosteroids were also given to prevent constriction. The ulcers on his feet were cleaned, dressed and secured with bandages. By day 4 in hospital, his symptoms had improved significantly and the drain was removed. To reduce the hazard of immune reconstitution inflammatory syndrome, antiretroviral therapy was delayed for 4–6 weeks and the patient was discharged from hospital.
Outcome and follow-up
At the 2-week follow-up visit, the pericardial fluid grew Mycobacterium tuberculosis fully susceptible to isoniazid as well as rifampicin on molecular screening with the GenoType MTBDRplus assay. The patient has been following up at the medical outpatient's clinic and reports no recurrent symptoms. He is due to initiate antiretroviral therapy at his next visit. His feet have healed well.
Discussion
This case illustrates the clinical value of the Xpert assay in the diagnosis of EPTB. Although recent reports have demonstrated the effectiveness of the Xpert assay in a variety of non-sputum samples,4 its use in pericardial fluid has only been evaluated, to the best of our knowledge, in a handful of clinical samples from three separate studies.5–7
Compared with conventional diagnostic tests for TB, the Xpert assay shows many potential benefits.8 Of six prospective and retrospective laboratory studies in which more than 150 extrapulmonary samples were tested, the Xpert assay showed acceptable sensitivity and high specificity for the diagnosis of TB. Sensitivity ranged between 54% and 95% and specificity was 98–100%.5–7 9–11 This wide range of sensitivities suggests that it is prudent at this time to regard the Xpert assay as a ‘rule-in’ test for the diagnosis of EPTB, rather than as a means of ruling out the diagnosis. Moreover, reported sensitivities often vary among different extrapulmonary sample types. Some studies, for instance, have observed lower sensitivity for the diagnosis of TB from pleural and other cavitatory samples.5 12
While the sensitivity of the Xpert assay is lower in smear-negative than in smear-positive samples,5–7 10 this case nonetheless highlights the value of a positive assay in the context of smear-negative EPTB. Of interest, one retrospective study of HIV-infected patients used small amounts of urine and the Xpert assay to screen for TB. Test sensitivity was reportedly 44% in those with CD4 counts below 50 cells/μL.13 These findings suggest that the assay may have usefulness as a screening tool in specific populations such as those with advanced immunodeficiency. TB is the most frequent cause of death among HIV-infected patients in Africa14 and in many instances this diagnosis is not made prior to death. Wider assessment of the role of the assay in the diagnosis of occult and elusive forms of TB is likely to benefit patients and physicians in Africa.
Although TB is by far the most common cause of pericardial effusion in HIV-infected patients,15 the Xpert assay is useful in the clinical decision-making process as it allows not only confirmation of a microbiological diagnosis, but also rapid detection—within 2 h—of rifampicin drug resistance. Historically, TB has been difficult to diagnose in pericardial fluid; the fluid is seldom smear (AFB) positive and the culture turnaround time too long (4–8 weeks) to assist in initial management decisions.16 The rapid diagnosis of TB drug resistance is thus important. The WHO estimates that multidrug-resistant disease now accounts for 3.7% of new incident cases of MTB.1 As rifampicin resistance is strongly suggestive of multidrug-resistant TB,8 its detection has important treatment considerations. In developing countries, this aspect of the Xpert assay is important in clinical practice, as timely and accurate drug susceptibility testing might not be possible. Time to detection of resistance, for example, varies from 20 days for a line-probe assay to 106 days for conventional methods.17 Other benefits of the Xpert assay, such as ease of use and reduced biohazard risk, should also be noted.8
In summary, compared with culture and smear microscopy, the Xpert assay combines acceptable sensitivity and excellent specificity of TB detection in EPTB with rapid determination of rifampicin drug resistance. Although our case documents a unique diagnostic approach to pericardial effusion, and EPTB in general, it has a much broader implication within the fields of HIV and TB. Given the high burden of EPTB in HIV-infected patients with TB, additional studies are warranted to further define the role of the Xpert assay in the context of the African epidemic of TB and HIV.
Learning points.
Extrapulmonary tuberculosis (EPTB) is common in HIV-infected patients with tuberculosis.
HIV-infected patients with EPTB often pose a diagnostic dilemma.
The new Xpert MTB/RIF (Xpert) assay could increase case detection in EPTB.
The Xpert assay allows for rapid identification and timely treatment of drug resistant tuberculosis.
Footnotes
Contributors: All authors made a contribution to the writing of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.WHO Global tuberculosis report 2012. Geneva, Switzerland: World Health Organization, 2012 [Google Scholar]
- 2.WHO Policy statement: automated real-time nucleic acid amplification technology for rapid and simultaneous detection of tuberculosis and rifampicin resistance: Xpert MTB/RIF system. Geneva, Switzerland: World Health Organization, 2011 [PubMed] [Google Scholar]
- 3.Kingkaew N, Sangtong B, Amnuaiphon W, et al. HIV-associated extrapulmonary tuberculosis in Thailand: epidemiology and risk factors for death. Int J Infect Dis 2009;2013:722–9 [DOI] [PubMed] [Google Scholar]
- 4.Lawn SD, Zumla AI. Diagnosis of extrapulmonary tuberculosis using the Xpert((R)) MTB/RIF assay. Expert Rev Anti Infect Ther 2012;2013:631–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tortoli E, Russo C, Piersimoni C, et al. Clinical validation of Xpert MTB/RIF for the diagnosis of extrapulmonary tuberculosis. Eur Respir J 2012;2013:442–7 [DOI] [PubMed] [Google Scholar]
- 6.Zeka AN, Tasbakan S, Cavusoglu C. Evaluation of the GeneXpert MTB/RIF assay for rapid diagnosis of tuberculosis and detection of rifampin resistance in pulmonary and extrapulmonary specimens. J Clin Microbiol 2011;2013:4138–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vadwai V, Boehme C, Nabeta P, et al. Xpert MTB/RIF: a new pillar in diagnosis of extrapulmonary tuberculosis? J Clin Microbiol 2011;2013:2540–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawn SD, Mwaba P, Bates M, et al. Advances in tuberculosis diagnostics: the Xpert MTB/RIF assay and future prospects for a point-of-care test. Lancet Infect Dis 2013;2013:349–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hillemann D, Rusch-Gerdes S, Boehme C, et al. Rapid molecular detection of extrapulmonary tuberculosis by the automated GeneXpert MTB/RIF system. J Clin Microbiol 2011;2013:1202–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Causse M, Ruiz P, Gutierrez-Aroca JB, et al. Comparison of two molecular methods for rapid diagnosis of extrapulmonary tuberculosis. J Clin Microbiol 2011;2013:3065–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moure R, Martin R, Alcaide F. Effectiveness of an integrated real-time PCR method for detection of the Mycobacterium tuberculosis complex in smear-negative extrapulmonary samples in an area of low tuberculosis prevalence. J Clin Microbiol 2012;2013:513–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Friedrich SO, Von Groote-Bidlingmaier F, Diacon AH. Xpert MTB/RIF assay for diagnosis of pleural tuberculosis. J Clin Microbiol 2011;2013:4341–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lawn SD, Kerkhoff AD, Vogt M, et al. High diagnostic yield of tuberculosis from screening urine samples from HIV-infected patients with advanced immunodeficiency using the Xpert MTB/RIF assay. J Acquir Immune Defic Syndr 2012;2013:289–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lawn SD, Churchyard G. Epidemiology of HIV-associated tuberculosis. Curr Opin HIV AIDS 2009;2013:325–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cegielski JP, Lwakatare J, Dukes CS, et al. Tuberculous pericarditis in Tanzanian patients with and without HIV infection. Tuber Lung Dis 1994;2013:429–34 [DOI] [PubMed] [Google Scholar]
- 16.Mayosi BM, Burgess LJ, Doubell AF. Tuberculous pericarditis. Circulation 2005;2013:3608–16 [DOI] [PubMed] [Google Scholar]
- 17.Boehme CC, Nicol MP, Nabeta P, et al. Feasibility, diagnostic accuracy, and effectiveness of decentralised use of the Xpert MTB/RIF test for diagnosis of tuberculosis and multidrug resistance: a multicentre implementation study. Lancet 2011;2013:1495–505 [DOI] [PMC free article] [PubMed] [Google Scholar]