Abstract
We describe a case of progressive multifocal leucoencephalopathy (PML) in a 39-year-old patient diagnosed with chronic lymphocytic leukaemia (CLL) who underwent two allogenic matched-sibling stem cell transplantations. PML was confirmed just after the first transplantation with cerebral MRI and by PCR in the cerebrospinal fluid. After immunosuppression withdrawal and cidofovir treatment, he achieved a reversal of clinical symptoms, John Cunningham (JC) virus positivity and MRI lesions regression. He remained asymptomatic for 5 years with no signs of infection activity, even though he received three new chemotherapy regimens due to a CLL relapse. However, after the second stem cell transplantation, new neurological symptoms began and a reactivation of the JC virus infection was detected. This time, treatment with mefloquine was started, but he experienced a progressive neurological deterioration and died 1 month after the symptoms began.
Background
Progressive multifocal leucoencephalopathy (PML) is an unusual and fatal disease after having used stem cell transplantation with a median survival of 19.5 months1 since the symptomatic onset. We believe that this is a very rare case because of the positive outcome that lasted 5 years and being the first reported case of reactivation after a durable remission.
Case presentation
On July 2007, a 39-year-old man diagnosed with chronic lymphocytic leukaemia (CLL) received a matched-sibling allogenic stem cell transplantation after two chemotherapy regimens with rituximab, fludarabine and ciclofosfamide. Conditioning was performed with fludarabine, ciclofosfamide and total body irradiation. Graft-versus-host-disease (GVHD) prophylaxis consisted of methotrexate and cyclosporine A. His pretransplant serology was negative for HIV, cytomegalovirus (CMV), hepatitis B and hepatitis C. John Cunningham (JC) polyoma virus serostatus was not tested. On day +150, he came to us after 1 week of progressive neurological symptoms: confusion, apathy and psychotic episodes. PML diagnosis was confirmed with MRI and JC virus DNA PCR in the cerebrospinal fluid. Immunosuppression with cyclosporine was discontinued but, because of no evidence of improvement, antiviral therapy with cidofovir was started 2 months after the onset of symptoms. After three cycles, symptoms progressively improved though behavioural disorders continued for 1 year after the treatment. He achieved a reversal of JC virus PCR positivity after five cycles of cidofovir and MRI scans showed a reduction of the lesions, but not a complete reversal.
Investigations
Haematological test at diagnosis showed lymphopenia with absolute lymphocyte count 690/mm3 and CD4 lymphocyte count 308 mm3.
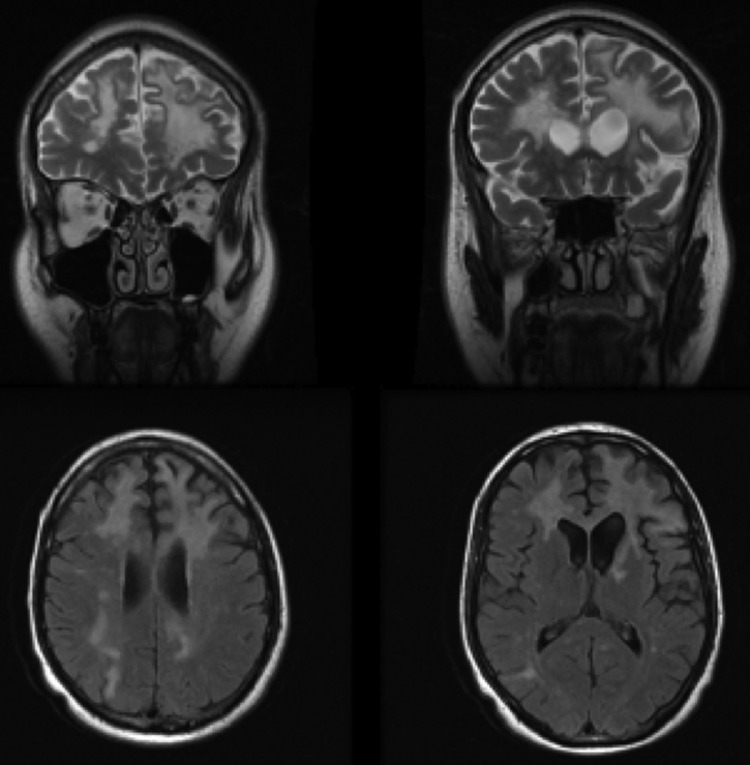
MRI at diagnosis showed several white matter hyperintense T2 lesions, the biggest one in the left frontal paraventricular region with severe perilesional oedema (figure 1). An MRI performed after treatment with cidofovir showed lesions regression.
Figure 1.
December 2007. Coronal and axial images (T2 and fluid-attenuated inversion recovery) show focal hyperintense signal.
Cerebrospinal fluid analysis showed elevated proteins, normal glucose and lactate dehydrogenase (LDH) levels, cell count and cytology. Cultures for bacteria, virus and fungi were negative, as well as PCR for CMV. JC virus PCR was positive.
Differential diagnosis
Progressive multifocal leucoencephalopathy should be taken into consideration in any bone marrow transplant recipient with neurological symptoms. However, encephalopathy is the most common complication affecting the central nervous system after stem cell transplantation and differential diagnosis should include toxic, metabolic, infectious, drug-induced, cerebrovascular or neoplastic causes, each of them with different approach and prognosis.2 3 Our patient showed no metabolic disorders. Because of its prior chemotherapy treatment, he had a special high risk for infections and MRI was compatible with it, so broad-spectrum antibiotic and antifungal treatments were started. Although cultures for bacteria and fungi were negative, this treatment was sustained until the JC virus PCR was confirmed. Simultaneously, tests for other viruses were made in his cerebrospinal fluid (CMV, Epstein Barr virus (EBV), herpes simplex virus (HSV)), but all the tests had negative results. Also, immunosuppression was withdrawn to avoid drug toxicity and infection progression. A brain biopsy was rejected due to the JC virus positivity.
Treatment
As PML is usually fatal and there is no therapeutic option that has proven to be of any real clinical benefit, we considered cidofovir to be an option, since is usually well tolerated and may achieve a positive outcome.4 5
Outcome and follow-up
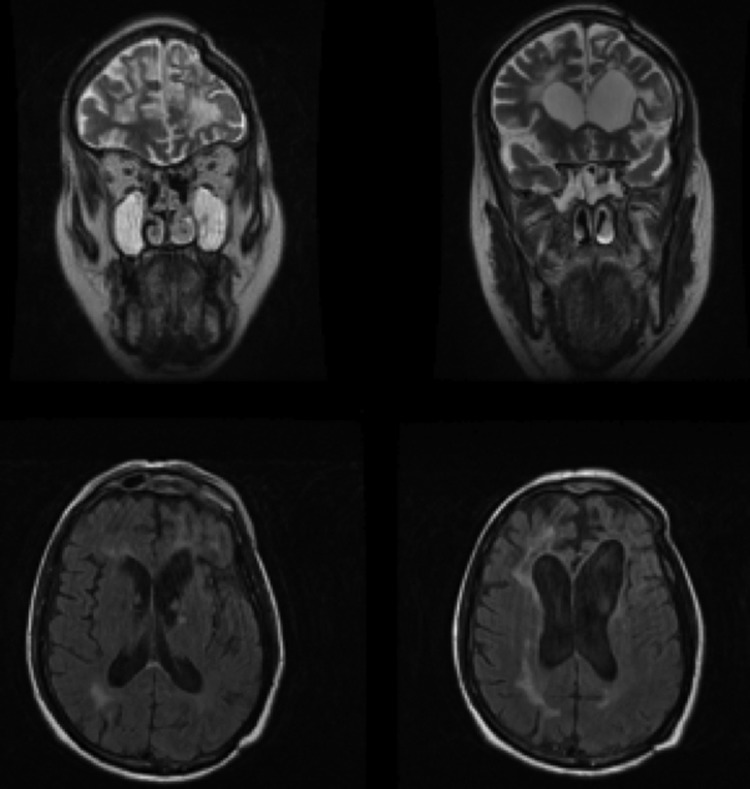
Three years after PML diagnosis, CLL relapsed and therefore he was treated with three new chemotherapy regimens (rituximab, lenalidomide, bendamustine). On July 2012, he underwent a second allogenic matched sibling stem cell transplantation from a different donor, his multiparous sister. After transplantation, he suffered GVHD affecting skin and lungs and immunosuppression with steroids and tacrolimus was required over a long period. After 8 months, he developed new neurological symptoms (ataxia and double vision), and JC virus DNA was confirmed again in cerebrospinal fluid. An MRI performed showed new progression of the frontal lesions (figure 2). CD4 were up to 500/mm3 when the JC virus reactivation was detected. Immunosuppression was decreased, but not discontinued, because of severe GVHD. In spite of the positive outcome for 5 years, this time cidofovir could not be administered due to hospital supply problems, and treatment with mefloquine was started. He experienced progressive neurological deterioration (psychomotor slowing, aphasia and episodes of seizure) and died 1 month after the beginning of the symptoms. At that moment, there was no evidence of CLL progression. His family refused to have an autopsy.
Figure 2.
March 2013. New images consistent with progressive multifocal leucoencephalopathy and residual gliotic lesions.
Discussion
This case is of special interest since it is rare to see a remission and later find reactivation of the disease. Another interesting aspect of our case is that he was treated with two different drugs with a very different outcome.
PML is a demyelinating central nervous system disorder caused by JC polyomavirus and characterised by the destruction of oligodendrocytes. Asymptomatic primary infection with JC virus usually occurs during childhood and the virus remains latent in kidneys indefinitely. The seroprevalence in adults is 80–90%.6 In immunocompromised hosts such as in patients with transplant, HIV infection and immunosuppressive-treated patients, JC virus can reactivate and cause this deadly disorder.7 PML was initially described in haematological patients with lymphoproliferative and myeloproliferative diseases, but it is more common in patients with HIV. Stem cell transplantation-related PML is very rare, with an estimated incidence rate of 35.4/ 100 000 person-years.8
Stem cell transplantation was not his only risk factor to develop PML. He had received fludarabine at diagnosis and rituximab as part of a combination therapy for his multiple relapses. Both of these drugs are known to be predisposing factors to PML, due to a profound T and B cell immunosuppression.9 10 However, in this case, there is a clear relationship between the stem cell transplantation and the onset of infection. Probably, each of the three factors contributed to the development of the disease, but stem cell transplantation seems to be the trigger factor.
Though in patients with HIV the CD4 count is the most important predisposing factor, there may be other unknown factors in stem cell transplantation related PML. Our patient showed low count of CD4 during the first infection, but a normal count during the second. On the other hand, he was treated with higher doses of immunosuppression that were reduced, but not discontinued because of GVHD. These data could suggest that PML after stem cell transplantation may be more related to the immunosuppression therapy and impairment of T cell function than to the lymphopenia.
PML results in a generally quick and fatal outcome, with few reported cases of improvement and prolonged stability.11 Although no treatment has proven to demonstrate any real therapeutic benefit, many different approaches have been tried.11–13 Withdrawal or dose reduction of the immunosuppressive regimen is the first approach, but it does not necessarily improve the outcome. Cidofovir is an antiviral agent that has been used in some of these patients with controversial results.5 6 12 13 However, clinical studies in patients with HIV showed no benefit.14 It is unclear whether the improvement in our patient was induced by cidofovir or it would have happened indistinctly with the discontinuation of immunosuppression. In 2013, during the second reactivation of the virus, the patient was unable to receive cidofovir because of hospital supply problems, so mefloquine, an antimalarial drug with likely efficacy against JC virus,15 16 was used instead. Treatment with mefloquine was not effective, but we have to take into account that the patient was severely immunosuppressed with tacrolimus and steroids, and complete withdrawal was not possible due to GVHD. Another difference between both PML episodes is the use of different immunosuppressant drugs, although no clear association with any specific immunosuppressant agent has been found.
Learning points.
Progressive multifocal leucoencephalopathy should be considered in the differential diagnosis of bone marrow recipients with neurological symptoms.
There is no proven effective therapy, but the withdrawal of immunosuppression and drugs such as cidofovir could be effective.
Late relapse of progressive multifocal leucoencephalopathy is also possible when immunosuppression is increased after long standing remission.
Footnotes
Contributors: AS-Q constructed the hypothesis and contributed to the literature review and the drafting of the manuscript. JB-A and CM-S gave expert opinion and reviewed the manuscript. LA-A helped with the drafting and preparation of the manuscript. All authors approved the final version of this manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Mateen FJ, Muralidharan R, Carone M, et al. Progressive multifocal leukoencephalopathy in transplant recipients. Ann Neurol 2011;2013:305–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krouwer HGJ, Wijdicks EFM. Neurologic complications of bone marrow transplantation. Neurol Clin N Am 2003;2013:319–52 [DOI] [PubMed] [Google Scholar]
- 3.Sostak P, Padovan CS, Yousry TA, et al. Prospective evaluation of neurological complications after allogenic bone marrow transplantation. Neurology 2003;2013:842–8 [DOI] [PubMed] [Google Scholar]
- 4.Reilmann R, Imai T, Ringelstein EB, et al. Remission of progressive multifocal leucoencephalopathy in SLE after treatment with cidofovir: a 4 year follow up. J Neurol Neurosurg Psychiatry 2005;2013:1304–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Auré K, Béhin A, Louillet F, et al. Dramatic improvement in non- AIDS related progressive multifocal leucoencephalopathy. J Neurol Neurosurg Psychiatry 2005;2013:1305–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weber T, Trebst C, Frye S, et al. Analysis of the systemic and intrathecal humoral immune response in progressive multifocal leukoencephalopathy. J Infect Dis 1997;2013:250. [DOI] [PubMed] [Google Scholar]
- 7.Koralnik IJ, Gonzalez-Scareno F, Dashe JF. Progressive multifocal leukoencephalopathy: treatment. UpToDate 2009. Available: http://www.uptodate.com/contents/progressive-multifocal-leukoencephalopathy-prognosis-and-treatment?source=see_link (accessed 1 April 2013)
- 8.Amend KL, Turnbull B, Foskett N, et al. Incidence of progressive multifocal leukoencephalopathy in patients without HIV. Neurology. 2010;2013:1326–32 [DOI] [PubMed] [Google Scholar]
- 9.Chakraborty S, Tarantolo SR, Treves J, et al. Progressive multifocal leukoencephalopathy in a HIV-negative patient with small lymphocytic leukemia following treatment with rituximab. Case Rep Oncol 2011;2013:136–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.D'Souza Anita, Wilson Jon, Mukherjee Sudipto, et al. Progressive multifocal leukoencephalopathy in chronic lymphocytic leukemia: a report of three cases and review of the literature. Clin Lymphoma Myeloma Leuk 2010;2013:E1–9 [DOI] [PubMed] [Google Scholar]
- 11.Zhang M, Li F, Rasper M, et al. Prolonged stability of progressive multifocal leukoencephalopathy in a patient with chronic lymphocytic leukemia. J Clin Oncol 2010;2013:e503–6 [DOI] [PubMed] [Google Scholar]
- 12.Osorio S, de la Cámara R, Golbano N, et al. Progressive multifocal leukoencephalopathy after stem cell transplantation unsuccessfully treated with cidofovir. Bone Marrow Trasplant 2002;2013:963–6 [DOI] [PubMed] [Google Scholar]
- 13.Kharfan-Dabaja MA, Ayala E, Greene J, et al. Two cases of progressive multifocal leukoencephalopathy after allogenic hematopoietic cell transplantation and a review of the literature. Bone Marrow Trasplant 2007;2013:101–7 [DOI] [PubMed] [Google Scholar]
- 14.Marra CM, Rajicic N, Barker DE, et al. A pilot study of cidofovir for progressive multifocal leukoenephalopathy in AIDS. Aids 2002;2013:1791. [DOI] [PubMed] [Google Scholar]
- 15.Kishida S, Tanaka K. Mefloquine treatment en a patient suffering from progressive multifocal leucoencephalopathy after umbilical cord blood transplant. Intern Med 2010;2013:2509–13 [DOI] [PubMed] [Google Scholar]
- 16.Gofton TE, Al-Khotani A, ÓFarrell B, et al. Mefloquine in the treatment of progressive multifocal leukoencephalopathy. J Neurol Neurosurg Psychiatry 2011;2013:452–5 [DOI] [PubMed] [Google Scholar]