Abstract
A 64-year-old woman who previously suffered myalgia with lower dose simvastatin was given just one high dose of simvastatin and developed rhabdomyolysis. This was a potentially life-threatening complication. Fortunately she recovered with conservative management and did not require haemofiltration. This case reminds us of the risks of statins and the caution that needs to be exercised when prescribing these medications to patients with a history of intolerances.
Background
This case report highlights a potentially fatal complication of statin therapy. Although the serious side effects of statins are rare, the sheer number of patients who take these drugs means that unfortunately, we are likely to see these complications in practice. This case serves as a reminder to exercise caution when prescribing these drugs and to remain vigilant for complications.
Case presentation
A 64-year-old woman presented to the acute medical take with a 1 day history of haematuria and myalgia. This occurred within 24 h of her first dose of simvastatin 80 mg which was started following review with a locum general practitioner (GP) at her usual practice. The indication was the treatment of dyslipidaemia in the context of primary prevention (10 year Framingham risk 11%). She took one dose and then on the following day developed pain and stiffness in her shoulders and thighs.
Her medical history was notable for hypercholesterolaemia and fibroids. She was not on any other regular medication. She was allergic to penicillin. She works as a medical secretary, drinks alcohol occasionally and does not smoke.
Clinical examination was normal, with no clinical evidence of muscle tenderness or weakness.
Investigations
On admission her creatine kinase was 426 700 (reference range 9–168 IU/L). Her liver function tests were also deranged, with a raised alanine transaminase (ALT) of 409 IU/L (reference range 0–55 IU/L). Her ALT had been normal 6 days prior to admission (19 IU/L). Her other liver enzymes were normal, including alkaline phosphatase and bilirubin. Her creatinine remained normal throughout.
Admission urinalysis showed large haematuria and proteinuria. Her ECG showed normal sinus rhythm. A venous blood gas showed she was not acidotic.
Treatment
Through her stay she remained symptomatic with myalgia but there was no weakness. She was given aggressive intravenous fluid resuscitation and had a good diuresis. Her creatinine did not rise and there was no requirement for haemofiltration.
Outcome and follow-up
Upon further questioning it transpired that she had previously been taking simvastatin at a dose of 40 mg. On this regime she developed muscle stiffness so it was discontinued by the patient herself. Several months later she returned to the practice and her fasting lipid profile was noted to be elevated; therefore, simvastatin was restarted at a higher dose of 80 mg by the locum GP.
Of note on admission her fasting lipid profile was: total cholesterol 5.3 mmol/L, high-density lipoprotein (HDL) 0.90 mmol/L and HDLR 5.89.
She was discharged on day 8 following admission and has made a good biochemical recovery (figure 1), although still reports intermittent myalgia.
Figure 1.
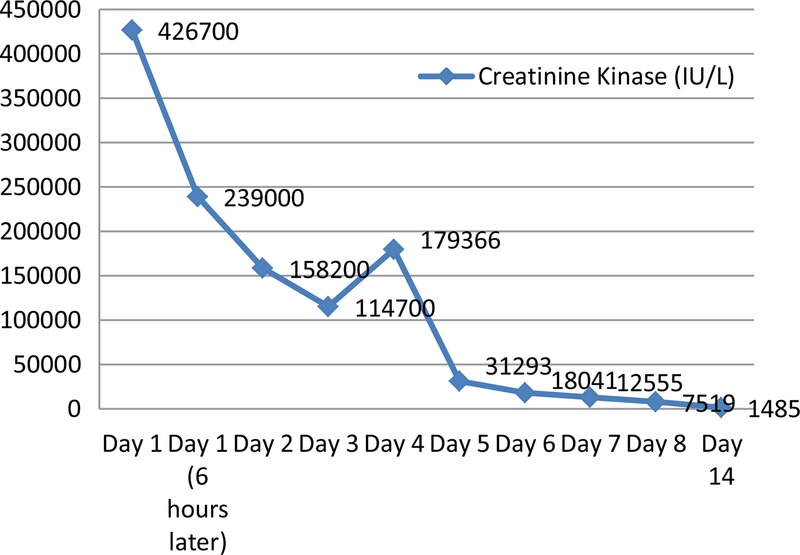
A graph outlining the trend in serum creatine kinase.
Discussion
Questions being asked: what is the incidence of statin-induced rhabdomyolysis, what are the predictors and is the effect dose dependent? To what extent should we limit statin use in those who have had previous statin side effects?
Search strategy: PubMed search using ‘simvastatin’, ‘simvastatin 80 mg’, ‘rhabdomyolysis’, ‘statin induced rhabdomyolysis’.
Conclusions being drawn: this case reminds us of the serious complications of statin therapy and warns us not to ignore the patient's previous experiences with statins.
Myalgias are common in patients taking statins but rhabdomyolysis is rare. The incidence was estimated as 4/100 000 person-years in one study.1 The risk increases with concurrent medication such as fibrates and drugs that inhibit the CYP3A4 isoenzyme (through which statins are metabolised), for example, calcium channel blockers, increasing age and liver dysfunction. This patient did not have any of these risk factors. However, as illustrated in this case, the rhabdomyolysis risk is also dose dependent, estimated as up to 10 times increased risk of rhabdomyolysis with simvastatin 80 mg compared to moderate dosing.2 Simvastatin in particular is the most notable of the statins for this3 but not exclusively; high-dose atorvastatin has similar problems.4 In 2011, the Food and Drug Administration(FDA ) in the USA issued a statement that simvastatin 80 mg should no longer be prescribed de novo and only continued in patients who have tolerated that dose for more than 1 year.5 If lipid control is not achieved using simvastatin 40 mg, then trialling an alternative statin is recommended rather than uptitrating simvastatin.
Mild myalgias are common symptoms with statins. They should settle within a few months upon discontinuation of the drug. If however you are to restart a statin then it is prudent to try a lower dose of a different statin to that which induced the myalgia. Recent observational work supports the efficacy of intermittent dosing of rosuvastatin (eg, 5 mg three times a week)6 or atorvastatin7 which could be useful in patients intolerant of higher doses of statins.
Statins are important drugs in the pharmacological armamentarium to reduce overall cardiovascular risk and we know that intensive lipid lowering reduces cardiovascular risk, in particular in high-risk patient groups such as those with proven cardiovascular events at a young age. Balancing the potential cardiovascular benefit of statins versus the potential side effect profile is an important dialogue for the clinician and patient to engage in. However, using high-dose simvastatin is not necessarily a safe or efficient way to achieve this.8
Learning points.
Generally only a very few patients should be on high-dose statins.
Simvastatin 80 mg is no longer indicated.
If you are trialling a different statin on a patient who has previously been intolerant to another statin then institute close clinical monitoring.
Severe complications of statin therapy can occur with one dose.
Footnotes
Contributors: UT collected the data, prepared the manuscript, and obtained the patient's consent for publication. RC reviewed the manuscript prior to submission.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.García-Rodríguez LA, Massó-González EL, Wallander M-A, et al. The safety of rosuvastatin in comparison with other statins in over 100 000 statin users in UK primary care. Pharmacoepidemol Drug Saf 2008;2013:943–52 [DOI] [PubMed] [Google Scholar]
- 2.Silva M, Matthews M, Jarvis C, et al. Meta-analysis of drug induced adverse events associated with intensive dose statin therapy. Clin Ther 2007;2013:253–60 [DOI] [PubMed] [Google Scholar]
- 3.Stolcpart RS, Olson KL, Delate T, et al. The risk for significant creatine kinase elevation with statins. Am J Cardiovasc Drugs 2010;2013:187–92 [DOI] [PubMed] [Google Scholar]
- 4.Holbrook A, Wright M, Sung M, et al. Statin-associated rhabdomyolysis: is there a dose-response relationship? Can J Cardiol 2011;2013:146–51 [DOI] [PubMed] [Google Scholar]
- 5.http://www.fda.gov/Drugs/DrugSafety/ucm256581.htm [Google Scholar]
- 6.Meek C, Wierzbicki AS, Jewkes C, et al. Daily and intermittent rosuvastatin 5 mg therapy in statin intolerant patients: an observational study. Curr Med Res Opin 2012;2013:371–8 [DOI] [PubMed] [Google Scholar]
- 7.Keating AJ, Campbell KB, Guyton JR. Intermittent non daily dosing strategies in patients with previous statin-induced myopathy. Ann Pharmacother 2013;2013:398–404 [DOI] [PubMed] [Google Scholar]
- 8.SEARCH Investigators Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12 064 survivors of myocardial infarction: a double-blind randomised trial. Lancet 2010;2013:1658–69 [DOI] [PMC free article] [PubMed] [Google Scholar]


