Abstract
A 32-year-old primigravida presented at our emergency room at 6 weeks of gestation with acute severe right upper quadrant abdominal pain, radiating to the right flank. Vital signs were stable. Abdominal ultrasound showed a round inhomogeneous mass of 10 cm diameter behind the right kidney, suspected for adrenal haemorrhage. The patient was admitted for observation. An MRI showed some right-sided pleural effusion and a round mass in the adrenal region with no recognisable adrenal gland, therefore most likely originating from the right adrenal. After 10 days the patient was discharged with no change in size of the haematoma. MRI was carried out every 2 months which showed a decrease in size of the haematoma, with no other abnormalities. Based on stable MRI and the patient’s preference, a vaginal delivery mode was chosen. At 37 weeks of gestation labour was induced, followed by an uncomplicated delivery.
Background
Spontaneous adrenal haemorrhage in pregnancy is a rare condition. Until now, most cases are treated surgically. However, when a patient’s clinical condition is stable, expectant management can be successful, with minimal risk for patient and fetus.
Case presentation
A 32-year-old primigravida presented at our emergency room at 6 weeks of gestation with acute severe right upper quadrant abdominal pain, radiating to the right flank, worsening with deep inspiration, accompanied by nausea and vomiting. The pain was progressive during the day. Her medical history reported a depression, a breast reduction, a cholecystectomy and hypothyroidism for which she had used thyrax in the past. A day earlier she was also seen at the emergency room for similar, although less severe discomforts. At that moment the pain was radiating to the thorax and she was suspected to have a pulmonary embolism, for which she received tinzaparine 0.7 mL. She was scheduled for advanced imaging the following day. However, before the scheduled CT scan was performed she returned to our emergency room with progressive discomforts.
Investigations
Her vital signs showed blood pressure of 130/80 mm Hg, pulse rate of 45 bpm, temperature of 36.6°C, respiratory frequency of 20/min and with saturation of 100%. Transvaginal ultrasound showed a live intrauterine pregnancy. Laboratory findings showed the following values: haemoglobin 7.6 mmol/L, haematocrit 0.36 L/L, mean cell volume 85.7 fl, leucocytes 18.4×109/L with a differentiation of 88.7% neutrophil granulocytes, thrombocytes 313×109/L, sodium 137 mmol/L, potassium 3.4 mmol/L, creatine 48 μmol/L, ureum 4.6 mmol/L, normal liver enzymes and glucose, and C-reactive protein 4.6 mg/L. A urine sediment showed some erythrocytes, ketones and protein.
Abdominal ultrasound showed a round inhomogeneous mass of 10 cm diameter behind the right kidney, suspected for adrenal haemorrhage (figure 1). Furthermore, the mass was causing a lateral shift of the right kidney and vena cava. The patient was admitted to our hospital for observation. Our differential diagnosis of the adrenal haemorrhage included idiopathic adrenal haemorrhage, haemorrhage due to a vascular or anatomical abnormality, bleeding because of adrenal venous thrombosis, a coagulopathy related to the pregnancy or acute bleeding inside an adrenal adenoma or neoplasm. One day later the ultrasound of the abdomen was repeated and showed no change in size of the mass. An MRI showed some right-sided pleural effusion and a round mass of 10×8.5×11.6 cm in the adrenal region with no recognisable right adrenal gland, therefore most likely originating from the right adrenal. The mass was heterogeneous with some layering and a hyperintense rim on the T1-weighted images, consistent with recurrent bleeding or haematoma (figure 2). The diagnosis was a spontaneous adrenal haemorrhage. The patient’s haemoglobin level dropped to 5.7, with a haematocrit of 0.28, on the day of admission and remained stable until the day of discharge. No blood transfusion was necessary. Renal and adrenal function remained normal, tested in a 24-h urine collection a day after admittance. The norepinephrine level in urine was determined to investigate the presence of a phaeochromocytoma and was slightly increased, 0.78 μmol/24 h, which later normalised and it was felt to be mildly elevated due to stress.
Figure 1.
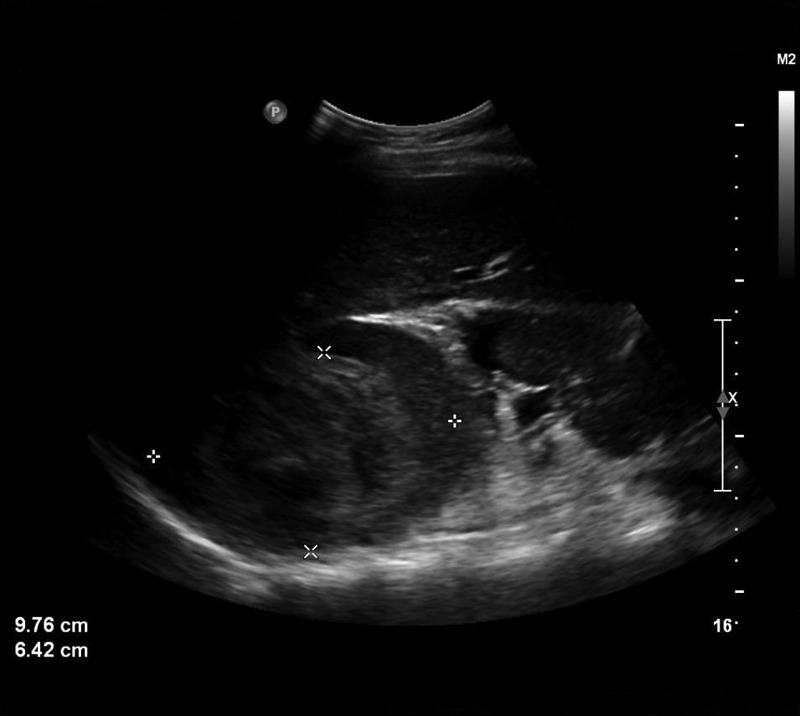
Abdominal ultrasound on the day of admittance showing a round inhomogeneous mass of almost 10 cm diameter behind the right kidney, suspect for adrenal haemorrhage.
Figure 2.
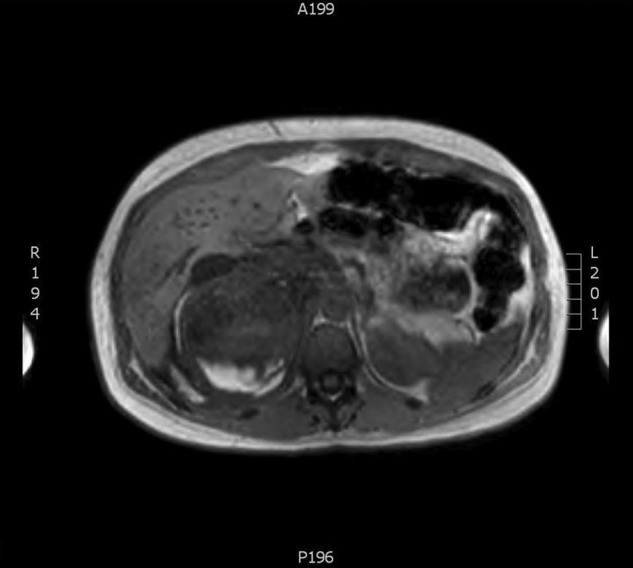
T1-weighted imaging of the adrenal area, a day after admittance. The mass in the right adrenal shows both hyperintense and isointense areas, due to recurrent bleeding.
Differential diagnosis
Our differential diagnosis of the adrenal haemorrhage included idiopathic adrenal haemorrhage, haemorrhage due to a vascular or anatomical abnormality, bleeding because of adrenal venous thrombosis, coagulopathy related to the pregnancy or acute bleeding inside an adrenal adenoma or neoplasm.
Outcome and follow-up
After 10 days the patient was discharged with no change in size of the adrenal haematoma on abdominal ultrasound. Follow-up examinations took place at the outpatient clinics of internal medicine and obstetrics. A 24-h urine collection was repeated 6 weeks after admittance and renal and adrenal functions remained normal. MRI was carried out every 2 months which showed a decrease in size of the haematoma to 4.4×5.5 cm, with no other abnormalities (figure 3). Specialists from different hospitals in the Netherlands were asked for their advice regarding the time of intervention and the desired mode of delivery; however, there was no consensus. Our main concern was the risk of rebleeding due to increased abdominal pressure during the delivery, although we did not find reports in literature regarding this matter.
Figure 3.
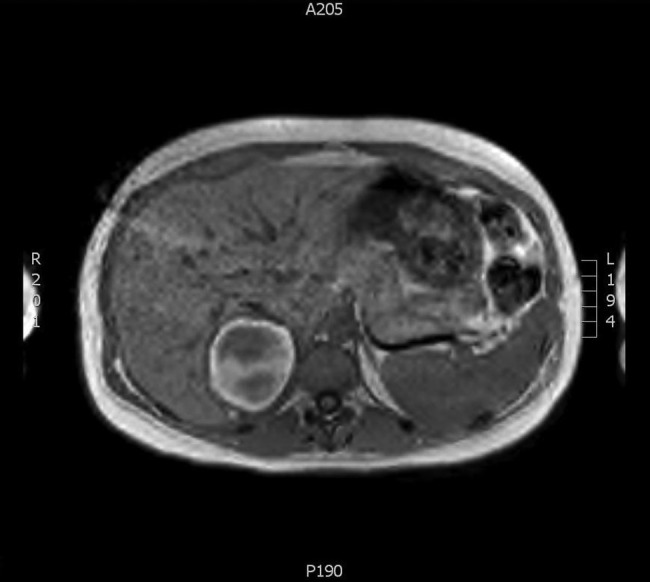
T1-weighted imaging showing a decrease in volume of the adrenal mass, several months after diagnosis. The haematoma is becoming hyperintense from the peripheral rim, due to the oxidation and conversion of deoxyhaemoglobin to free methaemoglobin.
Based on stable MRI and patient’s preference, a vaginal delivery mode was chosen. At 37 weeks of gestation labour was induced. Vital signs were normal. An uncomplicated delivery followed and a male infant of 3330 g was born, with Apgar Scores 9/10.
Postpartum the patient recovered well, but continued to have some mild symptoms related to the haemorrhage. An MRI scan 3 months postpartum still showed a residual haematoma of the right adrenal (figure 4). Four months after delivery a laparoscopic resection of the haematoma and a partial resection of the right adrenal was performed. Histological examination showed a pseudocyst, most likely to be of vascular origin, with no signs of malignancy. A 24-h urine collection showed again normal renal and adrenal functions.
Figure 4.
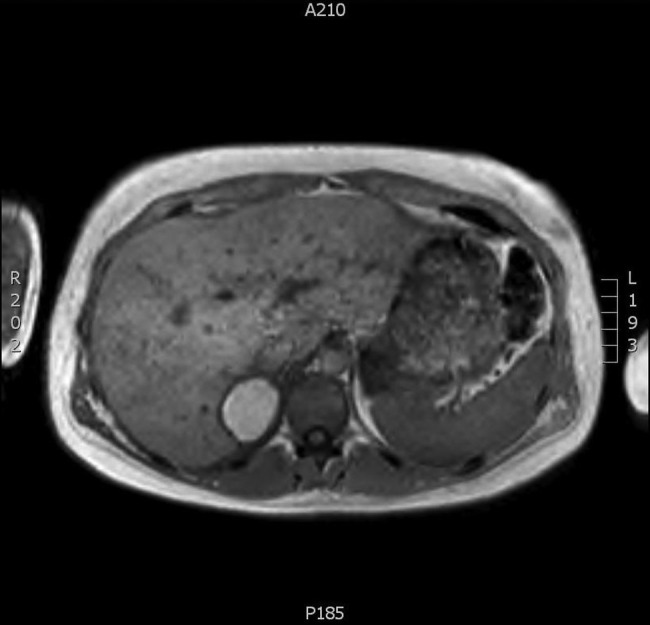
T1-weighted imaging showing further decrease in volume of the mass, almost a year after diagnosis. The mass is now fully hyperintense, showing further conversion from of deoxyhaemoglobin to free methaemoglobin.
Discussion
A PubMed search was conducted with the Mesh Terms “Adrenal Gland Diseases”, “Hemorrhage” and “Pregnancy”. Also title and abstract were searched for the terms “Adrenal”, “Hemorrhage” and “Pregnancy” to find the latest publications. Language was limited to English. A total of 85 hits were identified. Related citations were viewed and ultimately 11 publications were selected. The 12th article was selected by searching Pubmed for adrenal artery embolisation in spontaneous adrenal haemorrhage.
Aetiology
Adrenal haemorrhage is a rare condition, and symptoms often remain unrecognised. Autopsy figures for adrenal haemorrhage from all causes range from 0.14% to 1.1%.1 The incidence in pregnancy is unknown.2 Typically it is associated with meningococcal septicaemia, also known as Waterhouse-Friderichsen syndrome, but it can in fact occur in other clinical conditions. The most frequent being mechanical injury, postoperatively, haemorrhagic diathesis, chronic venous congestion, anticoagulation or coagulopathies such as antiphospholipid syndrome, intracranial and septic disorders, neoplastic infiltration of the adrenal gland, severe stress and pregnancy.3 4 So far only a few cases of adrenal haemorrhage in pregnancy have been reported, at different gestational ages. Anatomic factors predisposing to extensive haemorrhage are thought to be the rich arterial blood supply of the adrenal gland, its limited venous drainage and the delicate architecture of the vessel walls.3 Physiological adrenal cortex hyperplasia and hypertrophy during pregnancy, stress and central adrenal vein thrombosis may be other causes.3 In pregnancies complicated by pre-eclampsia, elevated blood pressure may cause rupture of the adrenal vessels. Necrosis and haemorrhage of the adrenal cortex were found in one-third of fatal cases of eclampsia.5
Clinical features
Adrenal haemorrhage can be asymptomatic or symptoms can be non-specific.1 3 Symptoms of adrenal haemorrhage may include acute onset of localised abdominal, flank pain, nausea, vomiting, hypotension, palpable flank mass, agitation and exhaustion. Most patients have associated low-grade fever.3 However, no pathognomonic symptoms exist.4
Diagnosis
Laboratory findings may vary from normal values to acute adrenal insufficiency, accompanied by hyponatraemia, hyperkalaemia, profound hypoglycaemia, leucocytosis, and falling haematocrit level.4 5 However, standard laboratory evaluation is not helpful in establishing the diagnosis.3
The initial imaging during pregnancy is usually abdominal ultrasound. The presence of a heterogeneous adrenal mass may suggest an adrenal haematoma, but follow-up imaging with MRI is required to exclude an underlying lesion such as an adenoma, phaeochromocytoma or carcinoma as the cause of the haemorrhage, which may require surgical intervention.6 MRI is the most accurate imaging modality for the diagnosis of non-traumatic spontaneous adrenal haemorrhage. Spontaneous adrenal haemorrhage appears on MRI as a heterogeneous mass and enlargement of one or both adrenal glands.5
In the acute phase (less than 7 days old), the haematoma appears isointense to hypointense on T1-weighted images and hyperintense on T2-weighted images as a result of the presence of intracellular deoxyhaemoglobin. In the subacute phase (7 days to 7 weeks), as the deoxyhaemoglobin is oxidised and converted to free methaemoglobin, the haemotoma gradually becomes hyperintense on T1-weighted images, beginning at periphery and moving towards the centre. In the chronic phase (beyond 7 weeks), a hypointense rim of haemosiderin may develop around the resolving haematoma. Gradient-echo images may show a characteristic blooming artefact from the magnetic susceptibility of haemosiderin. Gadolinium-enhanced T1-weighted images may show no enhancement or a thin rim of peripheral enhancement around the haematoma. A mixed signal in a chronic expanding haematoma (an ancient haematoma) has been called the mosaic sign. This signal is due to the coexistence of old and fresh blood.7 Although MRI appears to be more accurate than other imaging modalities, it still is difficult to determine if haemorrhage is secondary to a tumour.8
Differential diagnosis of a spontaneous adrenal haemorrhage includes adrenal venous thrombosis, acute bleeding inside an adrenal adenoma or neoplasm, haemorrhage resulting from septicaemia or pyelonephritis; in consequence some of these women are seen by the urologists.5 6
Treatment
Adrenal haemorrhage has clinical consequences only if followed by adrenal insufficiency 3 5 or in case of massive blood loss, in which case it can be potentially life threatening.9
Management of spontaneous adrenal haemorrhage in pregnancy therefore depends on the clinical condition of the patient, the amount of bleeding, imaging findings and the adrenal function.6 If haemorrhage is massive, surgery may be indicated to control bleeding. Radiological intervention can also be a viable alternative in patients who are unstable or medically unfit for major abdominal surgery. Embolisation allows preservation of any functional adrenal parenchyma and enables the patient to be stabilised, acting as a bridge to subsequent surgery.9 10
If the bleeding is less severe and the patient is haemodynamically stable, conservative management can be appropriate during pregnancy.2 5 6 11 Timely treatment with steroid replacement might be required. Preterm delivery may be necessary if adrenal haemorrhage is progressive or associated with severe pre-eclampsia or eclampsia.2 If adrenal haemorrhage is due to adrenal venous thrombosis anticoagulation therapy is necessary.11 Surveillance in the postpartum period is required in all cases, because the stress of delivery could theoretically cause recurrent adrenal haemorrhage.5 6 9 After resorption of the haematoma, full recovery of adrenal function with discontinuation of possible steroid replacement can be expected in most cases.11
Learning points.
MRI is the most accurate imaging modality for the diagnosis of spontaneous adrenal haemorrhage and to determine if there is any underlying aetiological mass which may require resection.
Conservative management in a stable patient may be appropriate; however, serial monitoring to ensure stable haemoglobin and adrenal function is indicated.
Surgical intervention may be warranted in an unstable patient, in massive haemorrhage or when an underlying neoplasm is suspected.
Radiological intervention can be a viable alternative in patients who are unstable or medically unfit for major abdominal surgery. Embolisation enables organ preservation and controls bleeding without disruption of the retroperitoneal space thereby reducing the associated morbidity and mortality.
If clinical condition allows you to do so, preterm delivery and a caesarean section can be avoided.
Footnotes
Contributors: All the authors made an individual contribution and were part of conception and design, drafting and revising and final approval.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Moore MA, Biggs PJ. Unilateral adrenal haemorrhage: an unusual presentation. South Med J 1985;2013:989–95 [DOI] [PubMed] [Google Scholar]
- 2.Cardwell MS. Spontaneous adrenal hemorrhage in pregnancy. A case report . J Reprod Med 1988;2013:233–5 [PubMed] [Google Scholar]
- 3.Vella A, Nippoldt TB, Morris JC. Adrenal hemorrhage: a 25-year experience at the Mayo Clinic. Mayo Clinic Proc 2001;2013:161–8 [DOI] [PubMed] [Google Scholar]
- 4.Mweemba DM, Beck I, Tuffnell DJ. Spontaneous maternal adrenal haemorrhage as a cause of intra uterine foetal death. J Obstet Gynecol 2005;2013:194–5 [DOI] [PubMed] [Google Scholar]
- 5.Gavrilova-Jordan LP, Edminster WB, Farrell MA, et al. Spontaneous adrenal hemorrhage during pregnancy: a review of the literature and a case report of successful conservative management. Obstet Gynecol Surv 2005;2013:3. [DOI] [PubMed] [Google Scholar]
- 6.Shantha N, Granger K. Spontaneous adrenal haemorrhage in early pregnancy. J Obstet Gynecol 2008;2013:449–51 [DOI] [PubMed] [Google Scholar]
- 7.Yamada T, Ishibashi T, Saito H, et al. Chronic expanding hematoma in the adrenal gland with pathologic correlations. J Comput Assist Tomogr 2003;2013:354–6 [DOI] [PubMed] [Google Scholar]
- 8.Hoeffel C, Legmann P, Luton JP, et al. Spontaneous unilateral adrenal hemorrhage: computerized tomography and magnetic resonance imaging findings in 8 cases. J Urol 1995;2013:1647–51 [DOI] [PubMed] [Google Scholar]
- 9.Christie J, Batool I, Moss J, et al. Adrenal artery rupture in pregnancy. BJOG 2004;2013:185–7 [DOI] [PubMed] [Google Scholar]
- 10.Patel A, Downing R, Vijay S. Spontaneous rupture of the adrenal artery successfully treated using the endovascular approach: a report of 2 cases. Vasc Endovasc Surg 2013;2013:1–4 [DOI] [PubMed] [Google Scholar]
- 11.Shen JZ, Stranks SN, Ho JT. Spontaneous adrenal haemorrhage in pregnancy. Intern Med J 2011;362–3 [DOI] [PubMed] [Google Scholar]


