Abstract
A 60-year-old Chinese patient was seen multiple times in the ophthalmology outpatient department due to persistent anterior-chamber inflammation and raised intraocular pressure. The patient was being treated with topical corticosteroids and oral acyclovir. Signs of corneal endotheliitis were observed in subsequent follow-ups. A clinical diagnosis could be made on slit-lamp examination, but aetiology could not be specified. An anterior-chamber diagnostic tap performed 18 months after the initial presentation revealed cytomegalovirus (CMV). Prompt response was noted with oral valganciclovir treatment. Our case highlights the importance of performing anterior-chamber tap in cases with persistent anterior-chamber inflammation. There was a long interval between the presentation and diagnosis mainly due to the absence of any concurrent ocular signs. An anterior-chamber tap was delayed until the ocular signs were suggestive of CMV endotheliitis. Timely diagnosis in such cases can improve the outcome as well as the prognosis.
Background
Diagnosis and management of persistent or recurrent anterior chamber inflammation with no other ocular signs can be a challenging scenario. We presented a case with anterior-chamber inflammation in which there was a long gap between the presentation and treatment mainly due to the absence of clinical signs.
Case presentation
A 60-year-old Chinese patient presented to the general ophthalmology clinic of our hospital in March 2011 with sudden blurring of vision and pain in the left eye. The visual acuity was 20/20 in the right eye and 20/30 in the left eye at the time of presentation. On slit-lamp examination, the left-eye cornea was clear. Anterior chamber was remarkable for fine keratic precipitates in the inferior half of the cornea and trace cells without any other ocular abnormality. The right eye was normal. The intraocular pressure (IOP) measured by Goldman applanation tonometry was 11 mm Hg in the right eye and 54 mm Hg in the left eye. The patient was administered topical 0.15% brimonidine eye drops twice daily, a combination of 2% dorzolamide and 0.5% timolol eye drops twice daily, and 1% prednisolone acetate eye drops 8 times a day. In addition, oral acetazolamide 250 mg was prescribed four times a day. The IOP dropped to 8 mm Hg in the left eye after 48 h. The antiglaucoma medications were stopped and prednisolone eye drops were tapered off to once a day dosage over the next 4 weeks. However, the patient returned within the next 2 weeks with a similar clinical picture of recurrent anterior chamber inflammation and an IOP of 30 mm Hg in the left eye. A similar management plan was adopted. In addition, oral acyclovir was added at a dose of 400 mg 5 times a day for 2 weeks subsequently reducing it to twice daily dosage. However, the anterior-chamber inflammation did not subside with oral acyclovir. Over the next few months, the patient consulted other ophthalmologists in private and was treated with oral acyclovir at a variable dose of 400 mg 2–5 times a day for a few months. Each time the dose of prednisolone acetate was lowered, the anterior chamber inflammation reappeared. In August 2012, the patient came back with further deterioration in visual acuity in the left eye. The visual acuity was 20/20 in the right eye and 20/50 in the left eye. Slit-lamp examination showed mild microcystic epithelial oedema, corneal stromal oedema and Descemet's membrane folds. The oedema involved lower three-fourth of the cornea with a clear demarcation between the oedematous and clear areas (figure 1A). A set of coin-shaped keratic precipiates were observed in the nasal quadrant (figure 1B). Topical 0.3% acyclovir eye ointment was added five times a day. There was no response within 1 week of treatment. The visual acuity deteriorated to 20/80 in the left eye and sectoral corneal oedema progressed to involve the upper nasal quadrant as well. A decision was taken to perform an anterior chamber tap. An informed consent was obtained and anterior chamber tap was performed under topical anaesthesia in the operating theatre.
Figure 1.
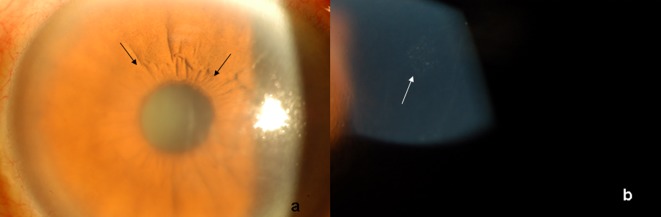
Slit-lamp photograph showing demarcated area of corneal oedema (arrows) (A); coin-shaped keratic precipitates (arrow) (B).
Investigations
After the anterior chamber tap, the aqueous humour was sent to the Microbiology laboratory for detection of cytomegalovirus (CMV), herpes simplex virus (HSV) and varicella zoster virus (VZV). The PCR was positive for CMV only.
Treatment
Oral valgancicovir was started at a dose of 900 mg twice daily. In addition, 1% prednisolone acetate eye drops were continued eight times a day. A significant improvement was noted in the signs and symptoms of the patient within 1 week of the start of treatment. At the end of 1 month after starting oral valgancicovir, the visual acuity improved to 20/20 in the left eye. The coin-shaped keratic precipitates disappeared and there was no residual anterior chamber inflammation (figure 2A). Diffuse iris atrophy was evident on slit-lamp examination (figure 2B). Over the period of the next 3 months, the patient developed corticosteroid-induced posterior subcapsular cataract. A successful phacoemulsification and intraocular lens implantation was performed in the left eye. The dose of oral valganciclovir was halved in April 2013 to 450 mg twice daily without any recurrence of the CMV endotheliitis.
Figure 2.
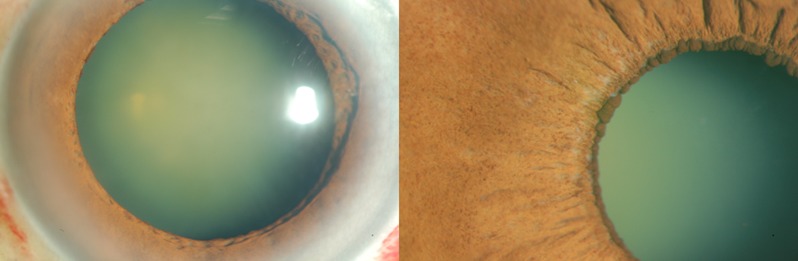
Slit-lamp photograph showing resolution of corneal oedema 1 month after treatment with oral valganciclovir (A); diffuse iris atrophy noticed after resolution of corneal oedema (B).
Discussion
The majority of the cases with anterior-chamber inflammation are idiopathic and do not require an anterior chamber tap. Common indications for a diagnostic anterior chamber tap include, persistent anterior chamber inflammation not responding to corticosteroids or presumed antiherpetic treatment, clinical features of Posner Schlossman syndrome or non-responding Fuchs’ heterochromic iridocyclitis and, high IOP despite maximal antiglaucoma therapy.1 In the present case, the initial treatment was based on the lines of idiopathic anterior chamber inflammation with no other ocular signs. The anterior uveitis had a waxing and waning course while the patient was on topical corticosteroids and oral acyclovir. Also, multiple opinions were being sought by the patient. It was only when the patient presented with corneal signs that were suggestive of CMV endotheliitis; a decision was taken to perform a diagnostic anterior chamber tap. In our case, the onset of corneal signs was very late in the disease course. The clinical signs suggestive of CMV endotheliitis included localised corneal oedema that was resistant to topical corticosteroids or acyclovir, linear endotheliitis, and coin-shaped keratic precipitates.1–7 Although aetiological agents in linear corneal endotheliitis include HSV and CMV, arrangement of keratic precipitates in a coin-shaped pattern is a specific manifestation of CMV-related corneal endotheliitis. Also, HSV and VZV are associated with disciform corneal endotheliitis.8
The utility of anterior chamber tap has been questioned recently in cases with anterior uveitis.9 However, since the treatment of CMV endotheliitis is very expensive, empirical therapy with oral valgancicovir was not considered. CMV was isolated form the aqueous humour and the patient responded very well to oral valganciclovir therapy.
Given the paucity of information about CMV endotheliitis, it is difficult to conclude about the ideal treatment. Taking a hint from the published literature, oral valgancicovir was started in our case. Although our case responded very well to the valganciclovir therapy, the optimal length of treatment needed is unknown to us.
Our case highlights the possibility of occurrence of CMV infection with persistent anterior chamber inflammation even in the absence of corneal signs. These cases can be taken up for an early diagnostic anterior-chamber tap if the clinical index of suspicion is high.
Learning points.
Diagnostic anterior chamber tap should be considered early in the course of the disease in cases with persistent anterior chamber inflammation not responding to corticosteroids or acyclovir treatment.
Typical signs of corneal endotheliitis should be looked for carefully on slit-lamp examination.
Oral valganciclovir treatment should be considered for the treatment of cytomegalovirus endotheliitis.
Footnotes
Contributors: VJ was involved in design and concept. VJ, RK and ALY were involved in writing of the manuscript and AY provided administrative support.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Koizumi N, Yamasaki K, Kawasaki S, et al. Cytomegalovirus in aqueous humor from an eye with corneal endotheliitis. Am J Ophthalmol 2006;2013:564–5 [DOI] [PubMed] [Google Scholar]
- 2.Chee SP, Bacsal K, Jap A, et al. Corneal endotheliitis associated with evidence of cytomegalovirus infection. Ophthalmology 2007;2013:798–803 [DOI] [PubMed] [Google Scholar]
- 3.Kandori M, Inoue T, Takamatsu F, et al. Prevalence and features of keratitis with quantitative polymerase chain reaction positive for cytomegalovirus. Ophthalmology 2010;2013:216–22 [DOI] [PubMed] [Google Scholar]
- 4.Suzuki T, Hara Y, Uno T, et al. DNA of cytomegalovirus detected by PCR in aqueous of patient with corneal endotheliitis after penetrating keratoplasty. Cornea 2007;2013:370–2 [DOI] [PubMed] [Google Scholar]
- 5.Chee SP, Bacsal K, Jap A, et al. Clinical features of cytomegalovirus anterior uveitis in immunocompetent patients. Am J Ophthalmol 2008;2013:834–40 [DOI] [PubMed] [Google Scholar]
- 6.Van Boxtel L, Van der Lelij A, van der Meer J, et al. Cytomegalovirus as a cause of anterior uveitis in immunocompetent patients. Ophthalmology 2007;2013:1358–62 [DOI] [PubMed] [Google Scholar]
- 7.Zamir E, Stawell R, Jhanji V, et al. Corneal endotheliitis triggered by cataract surgery in a Chinese patient with cytomegalovirus anterior uveitis. Clin Experiment Ophthalmol 2011;2013:913–15 [DOI] [PubMed] [Google Scholar]
- 8.Sutcliffe E, Baum J. Acute idiopathic corneal endotheliitis. Ophthalmology 1984;2013:1161–5 [DOI] [PubMed] [Google Scholar]
- 9.Anwar Z, Galor A, Albini TA, et al. The diagnostic utility of anterior chamber paracentesis with polymerase chain reaction in anterior uveitis. Am J Ophthalmol 2013;2013:781–6 [DOI] [PubMed] [Google Scholar]


