Abstract
Purpose
Cleidocranial dysplasia is an autosomal dominant disorder characterized by defective ossification of the intramembraneous ossification (primarily the clavicles, cranium, and pelvis), and it is caused by mutations in the RUNX2 gene that is responsible for osteoblast differentiation. Spine deformities were of progressive nature and considered to be the major orthopedic abnormalities encountered in our practice in patients with cleidocranial dysplasia. We aimed to further delineate the underlying spine pathology and its etiological understanding. Extraspinal deformities were dealt with respectively.
Material and methods
In this paper, we describe 7 patients who were consistent with the phenotypic and the genotypic characterization of cleidocranial dysplasia. Reformatted computed tomography (CT) scans have been applied in several instances to further understand the underlying pathology of progressive spine tilting. Radiographs were sufficient to illustrate other skeletal malformations.
Results
Anatomical survey demonstrates that a broad spectrum of frequently unrecognized orthopedic aberrations were encountered. We believe that torticollis has evolved in connection with the persistence of synchondrosis of the skull base and the upper cervical spine and these are strongly correlated to the well-known pathology of posterior occipital synchondrosis. Similarly, scoliosis and kyphoscoliosis resulted from the pathologic aberration of the cartilaginous stage of disrupted embryological development. All our results are discussed for the first time. Coxa vara, patellar dysplasia, and genu valgum were observed as extraspinal deformities.
Conclusion
This paper includes for the first time the anatomical analysis of the malformation complex of the craniocervical and the entire spine in patients with cleidocranial dysplasia. Reformatted CT scan was the modality of choice. We were able to illustrate that the persistence of skull base and the cervical spine synchondrosis were correlated with the pathological mechanism of the posterior occipital synchondrosis. Therefore, injuries to the craniocervical region in these patients might lead to a wide range of dreadful complications, ranging from complete atlanto-occipital or atlanto-axial dislocation to nondisplaced occipital condyle avulsion fractures with the possibility of morbid and or mortal outcome. On the other hand, the persistence of a cartilaginous spine was the reason behind the progressive spine tilting. This pathological form can be considered as a notoriously unpredictable malformation complex. The value of presenting these patients is to demonsterate that the genotype is not a precise index to assess the severity and the natural history of the phenotype.
Keywords: cleidocranial dysplasia, spine and skeletal malformations, radiographs, CT scanning, orthopedic interventions
Introduction
Cleidocranial dysplasia is a disorder in which the bones formed by intramembraneous ossification (primarily the clavicles, cranium, and pelvis) are abnormal. The characteristic feature in cleidocranial dysplasia is hypoplasia or absence of the clavicles. Although the most significant abnormalities are seen in the bones formed by intramembraneous ossification, enchondral growth is disturbed to a lesser degree, resulting in mild dwarfism. The main diagnostic criteria are hereditary malformative syndrome characterized by abnormal development of the skull (increased transverse diameter with delayed ossification of the fontanelles) and the clavicles are either aplastic or hypoplastic.1 Autosomal dominant inheritance with high penetrance and wide expressive variability, though one third of the cases are due to mutations. The possibility of a recessive form has been suggested as well.
Previous studies revealed that cleidocranial dysplasia is a dysplasia of the median points of particular segments of the skeleton (lack of median fusion of the cranial sutures and the symphysis of the mandible and posterior vertebral arches in addition to diastasis of the symphysis pubis and aplasia of the central nuclei of the clavicles).2–4
Tang et al5 have indicated that RUNX2 serves as a master gene regulating osteoblast-specific gene expression. The gene is expressed in the cells of osteoblast lineage only, and its expression is regulated by calciotropic agents. In odontogenesis, RUNX2 regulates key epithelial mesenchymal interactions that control the progress of morphogenesis and histodifferentiation of the epithelial enamel organ.
None of the above mentioned studies discussed the craniocervical and the spine pathology in patients with cleidocranial dysplasia. We proved that the posterior occipital synchondrosis is an extensive pathological mechanism with cephalocaudal mechansim.
Methods
The study protocol was approved by the Medical University of Vienna (Ethics Committee, EK Nr. 921/2009), and informed consents were obtained from the patients’ guardians. Our patients were of different ethnic origins. The patients’ records were studied at the Department of Bone Disorders, Orthopedic Hospital of Speising, Vienna, Austria. Extensive search for specific phenotypic features, natural history, and skeletal surveys were performed to prepare this review, which is illustrative of the spectrum of the skeletal abnormalities in cleidocranial dysplasia. All manifested round, flat facies, which were small in comparison with the large size of the skull. The superior orbital margins were prominent than the inferior margins.
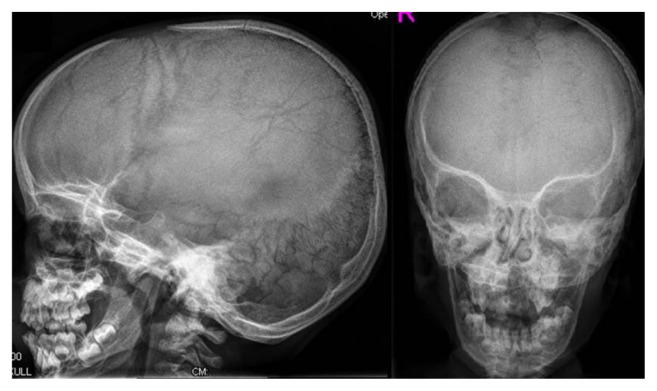
Saddle-shaped nose, flap ears, retroposed maxilla, and prominent mandible with a high-arched palate were notable. All our patients presented with abnormal cranial development such as frontal bossing, separated by a vertical sulcus (natiform forehead) associated with prominent parietal bossing, with the transverse diameter. Skull radiographs showed brachycephalic skull with increased biparietal diameter, frontal bossing, wide spaced sutures, multiple sutural (wormian bones), absent parietal bone ossification, with the anterior fontanelle remaining open associated with persistent posterior occipital synchondrosis. Closure of the sutures is markedly delayed, and the anterior fontanels were markedly enlarged. Persistence of the cranial fontanels, especially the bregmatic, with diastasis of the sutures and a membranous texture upon palpation (papyraceous cranium) were encountered in all patients (Fig. 1).
Figure 1.
Skull radiographs show brachycephalic skull with increase biparietal diameter, frontal bossing, wide spaced sutures, multiple sutural (wormian bones), and absent parietal bone ossification. The anterior fontanelle remains open, associated with posterior occipital synchondrosis. Closure of the sutures is markedly delayed, and the anterior fontanelle are markedly enlarged. Persistence of the cranial fontanelles, especially the bregmatic, with diastasis of the sutures and a membranous texture upon palpation of the papyraceous cranium are constant features in CCD.
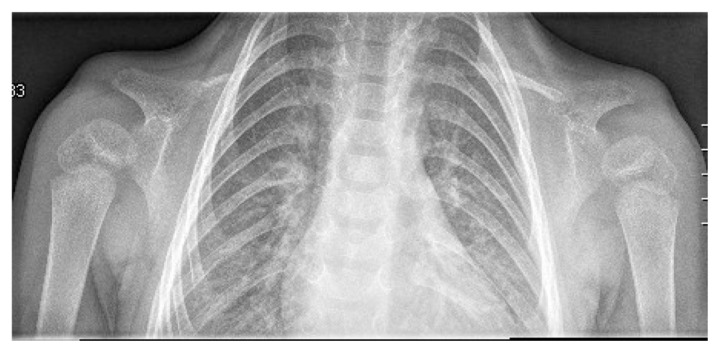
The trunks in all our patients were characterized by the presence of complete aplasia of the clavicles and are associated with disappearance of the supraclavicular and infraclavicular fossae so that the neck seems to imperceptibly continue into the thorax. Also present were winged scapulae and drooping shoulders with abnormal excessive mobility allowing the shoulders to be adducted to the point were the deltoid areas touch each other in the region of the sternum (puppet shoulders). In addition, the scapulae touch each other posteriorly (Fig. 2).
Figure 2.
The trunks in all our patients were characterized by the presence of complete aplasia of the clavicles and are associated with disappearance of the supraclavicular and infraclavicular fossae so that the neck seems to imperceptibly continue into the thorax. Winged scapulae, drooping shoulders with abnormal excessive mobility, allowing the shoulders to be adducted to the point where the deltoid areas touch each other in the region of the sternum (puppet shoulders) are shown.
All our patients showed abnormal craniofacial contour, torticollis, scoliosis, and kkyphoscolisois, and a constellation of extraspinal deformities such as coxa vara and genu valgum were also present.
Cranial development
The anatomy of the skull prior to skeletal maturity is important to consider in the management of spine maldevelopment. During the first 1 or 2 years of life, significant changes in the shape and location of the membranous bones of the calvarium occur as the skull plates grow and interdigitate. At birth, the anterior fontanel is present due to gaps between the paired frontal and parietal bones; this decreases in size by 6 months and is completely closed by 18 months of age.
The posterior fontanel, lying between paired occipital bones, generally closes by 4 months of age. Fifty percent of postnatal head growth occurs by the age of 18 months. Between 2 and 5 years of age, head circumference rapidly increases, tapering off by the age of 5 years.
Unlike the head, 50% of trunk growth is not reached until the age of 8 years; thus, head size is disproportionately large until then. Younger children have less cervical lordosis, the cervical Cobb’s angle is inversely proportional to the child’s age until 8. This allows the child’s head to center over the thorax to maintain balance and requires modification of the normal head position when using a halo immobilization. After the age of 5 years, the rate of skull growth decreases, and adult head size is generally attained by age 12.6–8
Radiographs were nonsufficient to understand the nature of the abnormal craniofacial contour. Therefore we referred to a reformatted computed tomography (CT) scan.
Torticollis
In all our patients, there was no sternocleidomastoid muscle spasm, nor was there aplasia of the muscles in the nuchal cavity of the affected side. The muscle strength, sensation, and reflexes ( Hoffman’s, Babinski’s and Chaddock’s reflexes) of the upper and lower limbs were negative. Bowel and bladder sphincter control were normal.
The neck mobility limitations were the reason to further analyze the craniocervical junction, namely the base of skull and the upper cervical vertebrae.
Skull base
The skull base is a platform at the bottom of the cranium that cradles the brain, provides support and protection, and serves as the entrance and exit for major vascular and neural structures. The skull base separates the neurocranium (calvaria) from the facial viscerocranium (jaw and muscles of mastication).
The skull base is called the chondrocranium because most of these bones are performed in cartilage and ossify by the process of endochondral ossification. Most of the facial bones and calvaria expand rapidly owing to the brain.6,7
The bones of the skull base are derived from cartilaginous precursors, known as the chondrocranium, while the calvarial bones form from membranous bone. The development of the cartilaginous skull base begins around the 40th day of gestation, with the conversion of mesenchyme into cartilage. This mesenchyme surrounds the developing notochord to form a floor for the base of the brain. During the 5th week, the notochord becomes enclosed by the bodies of the upper cervical vertebrae and passes into the basioocciput. Here it lies directly in contact with the endoderm of the embryonic pharynx. Skull base synchondroses are regarded as important growth centers of the craniofacial skeleton, particularly the sphenooccipital synchondrosis, because of its late ossification and important contribution to postnatal cranial base growth. The sphenooccipital synchondrosis seems to have a more prominent role in growth of the human skull up to adult life than other midline chondral structures. In the postnatal period, endochondral ossification of the cranial base synchondroses contributes to the expansion of the ossification centers and growth of the cranial base. Therefore, cranial base synchondroses are analogous structures to growth plates of the long bones in that they allow for rapid endochondral growth of the bone and eventually close when the bone reaches its final size.6,7,9,10
Radiographic assessment of the cervicocranium is the traditional modality for patients with spine deformities. It is based on the anteroposterior open mouth radiograph and a lateral radiograph and oblique view. There are instances in which interpretation of the upper cervical spine can be misleading and perhaps challenging because of the wide range of normal/abnormal anatomic variants and synchondroses.
The axis
The axis is formed from 4 primary ossification centers: the body, the 2 neural arches, and the dens. These ossification centers are separated by a cartilaginous plate called a synchondrosis. The synchondrosis between the dens and the body of C-2 is prone to fractures in young children.
In children, the axis is divided by synchondroses between the dens, body, and neural arches. The cartilaginous plate between the dens and body of C2 is an area of potential weakness that does not ossify until the child is 5 to 7 years old. The weak synchondrosis, in combination with the relatively large size of the child’s head, which can act as a pendulum in high speed trauma, makes the odontoid synchondrosis prone to traumatic injury.11,12
Trauma is the main cause of Occipito-atlantal abnormality, particularly in pediatric acute care practice. Children are vulnerable to this injury because of their small occipital condyles and horizontally oriented atlanto-occipital joints. Trauma can cause injury or rupture of the tectorial membrane and the alar ligaments that allow movement of the cranium relative to the spine.13 Dynamic lateral cervical spine radiographs showed vague anatomical structure of the odontoid in our patients.
The existence of craniocervical malformation signifies the potential for both sudden death and or significant morbidity as a result of maldevelopment of the skull base and the upper cervical vertebrae. To further understand the craniocervical malformation complex we referred to reformatted CT scan.
Scoliosis
The embryologic development of the vertebral column is a complex and rapid process. The complete anatomic pattern is formed in mesenchyma during the first 6 weeks of intrauterine life. Defects of formation or segmentation of the primitive vertebrae may occur during this period. Once the abnormal mesenchymal mold is established, the cartilaginous and bony stages follow that pattern, and the vertebral anomalies are fully established at birth. The classification of the developmental vertebral anomalies that produce congenital scoliosis is based on the embryologic development of the spine. There are 2 basic groups of anomalies: those caused by a defect of formation and those caused by a defect of segmentation of one or more vertebrae.14
Synchondrosis is the development of union between 2 bones by the formation of either hyaline cartilage or fibrocartilage. A synchondrosis is usually temporary and exists during the growing phase until the intervening cartilage becomes progressively thinner during skeletal maturation and ultimately becomes obliterated and converted into bone before adult life. In simple terms, a synchondrosis is a cartilaginous joint. It allows only slight movement between bones compared with the synovial joint, which has a much greater range of movement. The process of ossification within the centrum of the vertebral body is similar to that of tertiary ossification. Longitudinal growth mostly occurs at the chondroepiphyseal portions of the end-plates.
These areas also allow circumferential expansion of the vertebral centrum. The posterior elements also demonstrate longitudinal growth. An anterior growth plate exists at each neurocentral synchondrosis. A posterior growth plate at the spinous process synchondrosis allows the laminar and pedicular regions to lengthen. Posterior element growth ceases at 5 to 8 years of age after the synchondrosis close. Anterior column continues until 16 to18 years of age, and asymmetric closure may lead to scoliosis. Latitudinal growth is the result of a combination of perichondral and periosteal apposition, while longitudinal growth is due to endochondral ossification.
Vertebral growth plates enlarge via the addition of cells at the periphery. Interstitial growth in the transverse growth plate appears to be related to the enlargement of the epiphyseal ossification center. The vertebral physis has a limited height compared with that of long bones. The perichondral ossification zone of Ranvier is much less evident in a growing vertebra. Vertebrae grow through a typical endochondral ossification sequence, with the initial production of primary spongiosa. Remodelling occurs throughout the growth process until skeletal maturity. Throughout the human body, cartilaginous joints can be found in the symphysis pubis, between the ribs and sternum, between adjacent vertebrae in the spinal column, and at the growth plates between the epiphysis and metaphysic of tubular bones.15
Radiographs in our scoliotic patients showed progressive scoliosis and kyphoscoliosis in 5 patients out of 7. To further delineate the underlying pathology of the progressive spine tilting in these patients, we referred to reformatted CT scan.
Lower limb abnormalities
Coxa vara
Coxa vara is a decrease in the angle between the head or neck and shaft of the femur, often in presence of a metaphyseal defect.
In other words the neck-shaft angle is less than 110°. It is characterised by a decrease in the neck-shaft angle and clinically by a waddling gait or limb length discrepancy. Symptoms do not develop until the child starts to walk and often not before the age of 3 or 4 years. There is a typical limp or a waddling gait resembling that of dysplastic developmental dislocation of the hip. Abduction of the hip is limited, there is a positive Trendelenburg’s sign on standing on the affected side, and the greater trochanter is elevated. Congenital coxa vara results in a decrease in metaphyseal bone as a result of abnormal maturation and ossification of proximal femoral chondrocyte. As a result of congenital coxa vara, the inferior medial area of the femoral neck may be fragmented. A progressive varus deformity might also occur in congenital coxa vara as well as excessive growth of the trochanter and shortening of the femoral neck. Coxa vara is treated by valgus osteotomy of the proximal femur. Indications for surgery are identical to those for developemental coxa vara (ie, a neck-shaft angle of less than 90°, a Hilgenreiner-epiphyseal angle of 60° or more, or progression of deformity). Younger patients may show progressive acetabular remodelling after osteotomy. In older children, pelvic osteotomy to improve the containment of the hip is advised. Adductor tenotomy may be required after valgus osteotomy because of the lenghthening effect of valgus.
The major extra-articular limitations to adduction of the proximal segment of the femur after osteotomy are the tensor fascia lata and the gluteus medius and minimus muscles. If adequate adduction is not present when a valgus osteotomy is performed, an abduction contracture will result. Because of the long lever arm of the lower extremity, the abduction contracture, in some cases, may resolve with physical therapy and gravity.16,17 All our patients illustrated coxa vara.
Genu valgum
Genu valgum is a lower limb deformity that is characterized by the typical pattern of circumduction, requiring that the individual swing each leg outward while walking in order to take up steps without striking the planted limb with the moving limb. In children younger than 6 years, physiologic genu valgum is common but self-limiting and innocuous.
In children with pathologic genu valgum, when the axis deviates into or beyond the lateral compartment of the knee, regardless of the etiology, a remarkable number of problems may ensue.
Pathologic genu valgum warrants aggressive treatment to alleviate symptoms and prevent progression. Surgical intervention is the only successful intervention for correcting the deformity, which includes osteotomy and hemiepiphysiodesis (growth manipulation). Hemiepiphysiodesis may be planned, either temporary with staples or transphyseal screws or permanent via timed hemiepiphysiodesis. Valgus alignment of the lower extremities is normal in a child between 2 and 8 years of age. The maximum amount of physiologic valgus occurs between 2 and 4 years, after which the alignment of the lower extremities assumes a mild valgus femoral-tibial angle, the normal alignment in an adult. Therefore, by 8 years of age, there should be little or no change in alignment of the lower extremity, and preparation for treatment of what is deemed excessive physiologic valgus may be made at this age. In a younger child passing through the physiologic valgus phase, radiographs are not indicated unless there is evidence of unusual phenotypic features compatible with a skeletally dysplastic disorder. After 8 years of age, correction of excessive genu valgum may be indicated when there is gait disturbance, difficulty in running, knee discomfort, patellar malalignment, evidence of ligamentous instability, or excessive cosmetic concern.17–19 Two patients only out of 7 showed genu valga.
Patellar dysplasia
The anlage of the patella starts to form as early as the sixth week of foetal life by detachment from the anlage of the lower part of the femur, which takes place proximal to the region of the future joint and then descends by the third month of fetal life and lies in the depression between the future femoral condyles. The rectus femoris future tendon material is then seen running over the anterior surface of the anlage of the patella.20
Van Huyssteen et al21 showed that patients with symptomatic patellar instability will have either objective patellar instability (true atraumatic dislocation with an anatomical abnormality) or potential patellar instability (pain, catching or locking of the patellofemoral joint, and inability to rehabilitate quadriceps with an anatomical abnormality). All our patients manifested ischialpatellar dysplasia.
Results
Cranial development
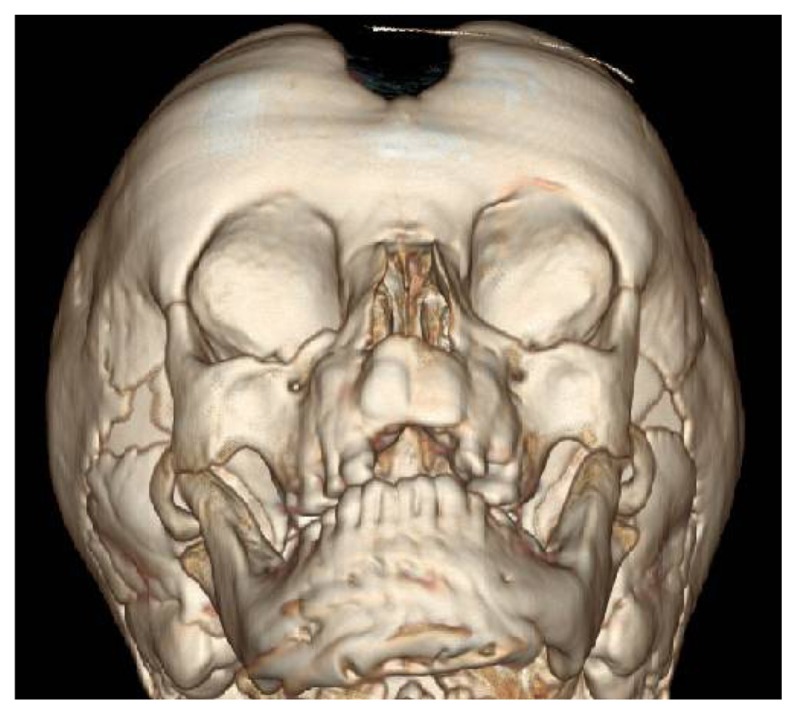
Reformatted CT scan of the skull in our patients showed increased biparietal diameter and frontal bossing, and the anterior fontanel remains open and markedly enlarged in an adult patient. There was defective ossification of the mandibular menti (symphysis). In addition, there was persistence of the line of the 2 pieces of the mandible (persistent synchondrosis), and prognathism was marked (Fig. 3).
Figure 3.
Reformatted CT scan of the skull show increased biparietal diameter and frontal bossing, and the anterior fontanel remains open and markedly enlarged in an adult patient. There was defective ossification of the mandibular menti (symphysis). In addition, there was persistence of the line of the 2 pieces of the mandible (persistent synchondrosis). Prognathism was marked associated with defective development of the upper jaw.
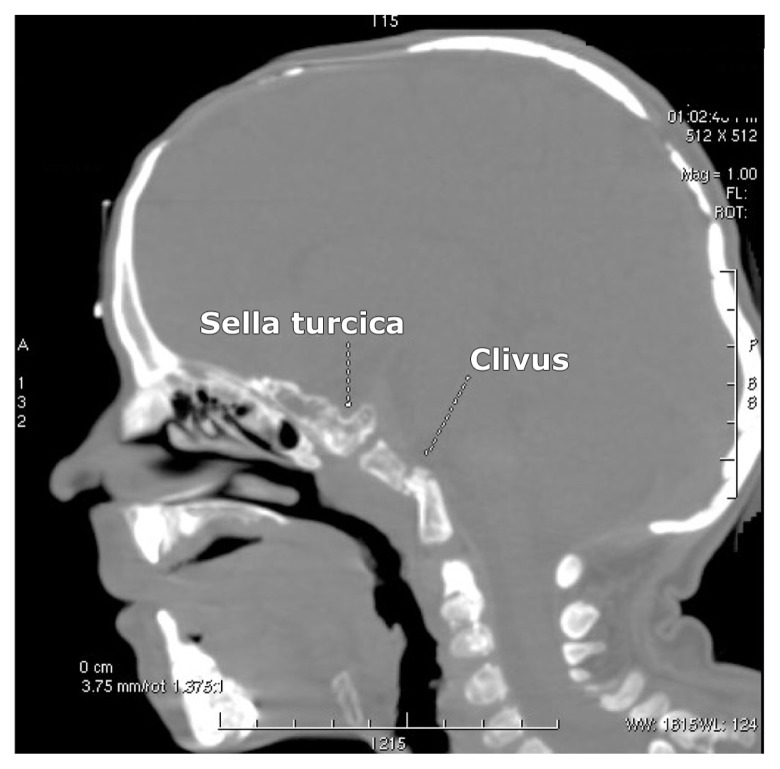
Torticollis
We encountered extreme malformation complex of diffuse skull base and upper cervical spine malformation complex. Sagittal reformatted CT scan in a 15-year-old patient with cleidocranial dysplasia showed defective ossification of the sella turcica and the clivus as well. In addition, it showed that the entirety of the skull base and most of the sphenoid bone and the clivus were cartilaginous, while the remainder of the cranial vault underwent simultaneous defective membranous ossification. The odontoid was hypoplastic and there was agenesis of the anterior arch of the atlas. Also note the severe ossification defects of the anterior and the posterior fontanels respectively (Fig. 4). Dentocentral synchondrosis has been detected in all patients.
Figure 4.
Sagittal reformatted CT scan in a 15-year-old adult patient with cleidocranial dysplasia showed defective ossification of the sella turcica and the clivus. In addition, it showed that the entirety of the skull base and most of the sphenoid bone and the clivus are cartilaginous, while the remainder of the cranial vault underwent defective membranous ossification. The odontoid is hypoplastic, and there was agenesis of the anterior arch of the atlas. Also note the severe ossification defects of the anterior and the posterior fontanels respectively.
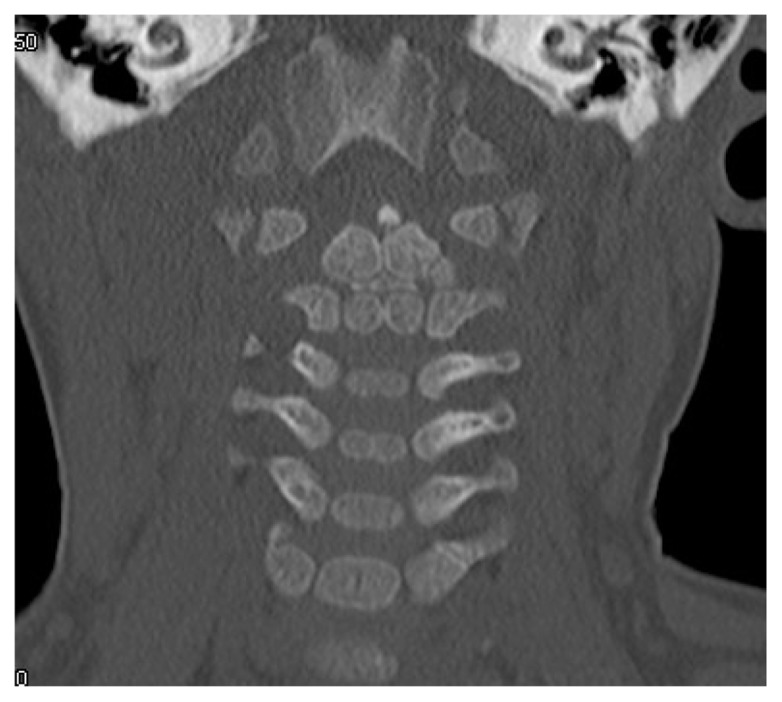
Coronal reformatted CT scan in an 9-year-old-patient showed dentocentral synchondrosis of the axis associated with odontoid process dysplasia and persistence of infantile synchondrosis over the entire cervical spine (Fig. 5).
Figure 5.
Coronal reformatted CT scan in a 9-year-old patient showed dentocentral synchondrosis of the axis associated with odontoid process dysplasia and persistence of infantile synchondrosis over the entire cervical vertebrae.
Scoliosis
Reformatted coronal CT scan of the spine in an adult patient (17 years of age) showed the massive pathologic aberration of the cartilaginous stage of development (defective primary ossification of the vertebral column) causing effectively the maldevelopment of extensive butterfly and hemivertebrae (like) because of defective ossification along the entire spine with subsequent development of progressive scoliosis/ kyphoscoliosis (Fig. 6).
Figure 6.

Reformatted coronal CT scan of the spine in a 17-year-old adult patient showed the massive pathologic aberration of the cartilaginous stage of development (defective primary ossification of the vertebral column) causing effectively the maldevelopment of extensive butterfly-like and hemivertebrae like malformation (defective vertebral ossification) along the entire spine with subsequent development of progressive scoliosis/kyphoscoliosis.
This result confirms that the overall latitudinal growth, the longitudinal growth, the vertebral growth plates, and the interstitial growth of the entire spine in patients with cleidocranial dysplasia are remarkably defective.
Lower limb abnormalities
Coxa vara
One 12-year-old patient underwent valgus osteotomy of the proximal femora. LCP-Pediatric-Hip Plate has been applied bilaterally to correct the varus deformity and to rotate the proximal femoral physis from a vertical to horizontal position (Fig. 7).
Figure 7.
AP radiograph in a 12-year-old patient showed valgus osteotomy of the proximal femora to correct the coxa vara. LCP-Pediatric-Hip Plate has been applied bilaterally to correct the varus deformity and to rotate the proximal femoral physis from a vertical to horizontal position.
Genu valgum
Hemiepiphysiodesis (guided growth technique) was planned in a 9-year-old patient (temporary hemiepiphysiodesis with 8-plates via timed hemiepiphysiodesis has been performed) (Fig. 8).
Figure 8.

Hemiepiphysiodesis in a 9-year-old patient (temporary hemiepiphysiodesis with 8-plates via timed hemiepiphysiodesis) was performed.
Patellar dysplasia
Anterioposterio (AP) radiograph of the pelvis and lateral radiographs of the knees in an 11-year-old patient with cleidocranial dysplasia show that the pelvis and knees showed a combination of delayed ossification of the ischium and pubis. In addition, there was maldevelopment of the capital femoral epiphyses and both were separated from the metaphyses with upward and medial inclination. Note the gap between the epiphyses and the irregular metaphyses respectively. Hypoplasia of the patellae was evident with subsequent development of patellar maltracking (Figs. 9 and 10).
Figure 9.
AP radiograph of the pelvis in a 9-year-old patient with cleidocranial dysplasia. Note that the pelvis showed a combination of delayed ossification of the ischium and pubis. In addition, there was maldevelopment of the capital femoral epiphyses, and both were separated from the metaphyses with upward and medial inclination. Note the gap between the epiphyses and the irregular metaphyses respectively.
Figure 10.
Lateral knees radiograph in a 9-year-old patient showed defective ossification of the patellae with subsequent development of patellar maltracking.
Discussion
Marie and Sianton1 and recent reports3–5 revealed that cleidocranial dysplasia or dysostosis involves dental anomalies and bone abnormalities with membranous ossification of clavicles, cranium, face, and pelvis but rarely of the spine and the remainder of the skeleton. The main radiographic features, as previously reported, are associated with the skull, which is described as brachyphalic associated with increased biparietal diameter, frontal bossing, wide-spaced sutures, multiple wormian bones, and anterior fontanelle remaining open in adulthood associated with posterior occipital synchondrosis persisting until 4 or 5 years of life.3,4 Our results showed that skull base and entire spine malformation complexes are the paramount deformities in patients with cleidocranial dysplasia and require special attention and care.
The cervical spine differs from the thoracic or lumbar region in both anatomy and functional respects. In particular, the upper cervical spine has its own unique anatomy, including several ligaments designed to permit axial rotation of the atlas and head. Therefore the pathogenesis of cervicothoracic scoliosis should be carefully evaluated. Studying the craniocervical abnormality in scoliotic patients needs a higher index of suspicion and prompt evaluation.
The odontoid abnormalities have a reputation for being missed, leading to a situation of future instability and potential risk for neurologic injury.13 The axis develops from 5 primary centers of ossification, which are usually present at birth. There is 1 center for the body of the axis, 2 for the odontoid process (which represents the body of the atlas), and 2 for the vertebral arch. The neurocentral synchondrosis, the cartilaginous structure that joins the body to the 2 posterior centers of ossification, ossifies between the ages of 3 and 6 years. In our group of patients, it was quite obvious that synchondrosis was a permanent rather than a temporary process.
Currarino22 described primary spondylolysis of the axis in 3 children, 1 of whom had pycnodysostosis. He suggested that the lesion might be congenital and represents a defect of chondrification of the mesenchymal precursor of the vertebra rather than a failure of fusion of the centers of ossification.
Embryologically, the spine develops in 3 stages: the membranous, the cartilaginous, and the ossific. In the membranous stage, the axial skeleton first differentiates from the mesenchyme, most of which occurs in serially arranged pairs of mesodermal segments designated as sclerotomes. The sclerotomes migrate to lie in paired segmental masses alongside the notochord. Each sclerotome differentiates into a compact caudal portion and a less dense cranial half. At alternate segments, there is an intersegmental artery between a less dense and a compact portion. The denser caudal part of each sclerotome mass then unites with the looser cranial half and thus forms the substance of the definitive vertebra. The intervertebral disk differentiates from the denser caudal region. This is called the membranous vertebral column, which is succeeded at about the fourth week of foetal life by the cartilaginous vertebral column. Two cartilaginous centers appear on either side of the notochord and rapidly extend around it, thereby forming the bodies of the cartilaginous vertebrae. Second pairs of cartilaginous foci appear in the lateral parts of the vertebral arch. Still different cartilaginous centers appear for each costal arch.23,24 Interestingly, it was evident that our patients manifested typical patterns of embryological cartilaginous aberration.
Kusumi and Turnpenny25 described a list of spine malformation complex in connection with several syndromic entities that resulted from disruption of the induction of formation of the axial skeleton; Klippel-Feil syndrome, spondylocostal dysotosis, Jarcho-Levin syndrome, Goldenhar syndrome, VACTERL association (also VATER syndrome) which is a non-random association of birth defects were included as well in their study. Cleidocranial dysplasia was not included.
Huynh et al26 hypothesized that asymmetrical (left-sided or right-sided) growth at this site is believed to lead to pedicle-length asymmetry, which then causes vertebral rotation and, ultimately, the development of scoliotic curves. A computer model was used to investigate whether pedicle asymmetry, either alone or in combination with other deformations, could be involved in the pathomechanisms leading to scoliosis. In light of our findings, we can consider that the hypothesis of Huynh et al is partially accepted.
The lower extremities are normally weight bearing throughout life; axial alignment of the lower extremities is critical with respect to determining the demands to which articular cartilage is repeatedly exposed during gait. Alignment is therefore an important consideration in many clinical situations, whether considering deformity corrections, fracture reduction, or total knee arthroplasty. Alignment refers to the collinearity of the hip, knee, and ankle. Orientation refers to the position of each articular surface relative to the axes of the individual limb segments (tibia and femur). Alignment and orientation are best judged using standing long AP view radiographs of the entire lower extremity. Proper rotation of the limb is critical and requires the patella be centered between the femoral condyles and directed forward. A standardized technique is useful to assure that the radiographs are reproducible. The knee is most vulnerable to changes in the normal coronal plane relationship of the joints of the lower extremity.17,27
Valgus osteotomy of the upper femur at the intertrochanteric or subtrochanteric level is the most effective way to correct the varus deformity, to rotate the proximal femoral physis from a vertical to horizontal position (relieving shear stress on it), and to enhance ossification of the defect. LCP-Pediatric-Hip Plate has been applied bilaterally to correct the varus deformity and to rotate the proximal femoral physis from a vertical to horizontal position and has been performed successfully in 1 of our patients.28 Guided growth technique has been performed to overcome the genu valga in 2 patients with cleidocranial dysplasia.
The guided growth is a well known technique from the work of Blount.29 Though 8- plate technique as invented by Peter Stevens, which consists of extraperiosteal application of small low-profile 2-hole plate and an overpassing growth plate, was our choice.30 The pelvis and knees show a combination of absent or delayed ossification of the ischium or part of the ischium and or pubis and absent or deficient ossification and hypoplasia of the patellae. Small or absent patellae associated with abnormal ossification of the ischiopubic junction and/or infra-acetabular ax cut notches are critical findings for the clinical diagnosis of small patella syndrome.20 It seems that patients with cleidocranial are manifesting similar pelvic and patellar abnormalities as in small-patella syndrome.
The patellar stability relies on the limb alignment; the osseous architecture of the patella and the trochlea, the integrity of the soft tissue constraints, and the interplay of the surrounding muscles are the basic principles of normal alignment. Ischiopubic-patella syndrome is a generalized bone dysplasia with diagnostic features in the pelvis and knees and subtle changes in other parts of the skeleton, as well as dysmorphic features.20
Summary
A literature review in patients with cleidocranial dysplasia was mostly restricted to delineate the phenotypic and genotypic correlations. None of the above mentioned articles discussed the aetiology behind the serious spine malformation complex. Through the detailed anatomical analysis of the spine via reformatted CT scan, we were able to confirm the existence of disrupted embryological development amid the cartilaginous stage of embryological development of the spine. This sort of aberration was the reason of the maldevelopemnt of the entire spine causing progressive scoliosis and kyphoscoliosis in 5 patients with cleidocranial dysplasia. In practice, this sort of spine pathology can be considered a hazardous pattern of spine maldevelopment.
Spine physicians and surgeons should have proper understanding of the risks involved in therapy or surgery for patients with cleidocranial dysplasia. Without a definite knowledge of the pathophysiology of a suspected syndrome, it is quite difficult to plan a preoperative strategy for major spine surgery in these patients.
Conclusion
The value of presenting these patients is to demonstrate that the genotype is not a precise index to assess the severity and the natural history of the phenotype.
Footnotes
Author Contributions
AAK, FBC wrote the paper and analyzed the radiographic and tomographic data; VK, RG, CR, FG performed the operations on these children; JH, KK helped in structuring the manuscript. All authors reviewed and approved of the final manuscript.
Competing Interests
Author(s) disclose no potential conflicts of interest.
Disclosures and Ethics
As a requirement of publication the authors have provided signed confirmation of their compliance with ethical and legal obligations including but not limited to compliance with ICMJE authorship and competing interests guidelines, that the article is neither under consideration for publication nor published elsewhere, of their compliance with legal and ethical guidelines concerning human and animal research participants (if applicable), and that permission has been obtained for reproduction of any copyrighted material. This article was subject to blind, independent, expert peer review. The reviewers reported no competing interests.
Funding
Author(s) disclose no funding sources.
References
- 1.Marie P, Sianton P. Observation d’ hydrocephalie hereditaire (pere et fils) par vice de development du crane et du cerveau. Bull Mem Soc Med Hop Paris. 1897;14:706. [Google Scholar]
- 2.Jensen BL. Somatic development in cleidocranial dysplasia. Am J Med Genet. 1990;35:69–74. doi: 10.1002/ajmg.1320350113. [DOI] [PubMed] [Google Scholar]
- 3.Suba Z, Balaton G, Gyulai-Gaal S, Balaton P, Barabas J, Tarjani I. Cleidocranial dysplasia: diagnostic criteria and combined treatment. J Craniofac Surg. 2005;16:1122–6. doi: 10.1097/01.scs.0000179747.75918.58. [DOI] [PubMed] [Google Scholar]
- 4.Shen Z, Zou CC, Yang RW, et al. Cleidocranial dysplasia: report of 3 cases and literature review. Clin Pediatr. 2009;48:194–8. doi: 10.1177/0009922808323107. [DOI] [PubMed] [Google Scholar]
- 5.Tang S, Xu Q, Xu X, et al. A novel RUNX2 missense mutation predicted to disrupt DNA binding causes cleidocranial dysplasia in a large Chinese family with hyperplastic nails. BMC Med Genet. 2007;8:82–7. doi: 10.1186/1471-2350-8-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curtin HD, Chavali R. Imaging of the skull base. Radiol Clin North Am. 1998;36:801–17. doi: 10.1016/s0033-8389(05)70065-8. [DOI] [PubMed] [Google Scholar]
- 7.Sperber GH. Craniofacial Embryology. Boston, MA: Wright; 1981. pp. 87–101. [Google Scholar]
- 8.Hayashi I. Morphological relationship between the cranial base and dentofacial complex obtained by reconstructive computer tomographic images. Eur J Orthod. 2003;25:385–91. doi: 10.1093/ejo/25.4.385. [DOI] [PubMed] [Google Scholar]
- 9.Bjork A. Cranial base development. Am J Orthod. 1955;41:199–255. [Google Scholar]
- 10.Ford E. Growth of the human cranial base. Am J Orthod. 1958;44:498–506. [Google Scholar]
- 11.Cendekiawan T, Wong RWK, Rabie ABM. Relationships between cranial base synchondroses and craniofacial developement. A Review. The Open Anatomy Journal. 2010;2:67–75. [Google Scholar]
- 12.Garton HJL, Park P, Papadopoulos SM. Fracture dislocation of the neurocentral synchondrosis of the axis. Case illustration. J Neurosurg Spine. 2002;96:350. doi: 10.3171/spi.2002.96.3.0350. [DOI] [PubMed] [Google Scholar]
- 13.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–74. [PubMed] [Google Scholar]
- 14.Labrom R. Growth and Maturation of the spine from birth to adolescent. J Bone Joint Surg. 2007;89:3–7. doi: 10.2106/JBJS.F.01236. [DOI] [PubMed] [Google Scholar]
- 15.Theiler K. Vertebral malformations. Adv Anat Embryol Cell Biol. 1988;112:1–99. doi: 10.1007/978-3-642-73775-6. [DOI] [PubMed] [Google Scholar]
- 16.Trigui M, Pannier S, Finidori G, Padovani JP, Glorion C. Coxa vara in chondrodysplasia. prognosis study of 35 hips in 19 children. J Pediatr Orthop. 2008;28(6):599–606. doi: 10.1097/BPO.0b013e3181831ec8. [DOI] [PubMed] [Google Scholar]
- 17.Staheli LT. Lower deformity in infants and children. A review. J Pediatr Orthop. 1990;10:559–63. [PubMed] [Google Scholar]
- 18.Steel HH, Sandrow RE, Sullivan PD. Complications of tibial osteotomy in children for genu varum or valgum. Evidence that neurological changes are due to ischaemia. J Bone Joint Surg Am. 1971;53:1629–35. [PubMed] [Google Scholar]
- 19.Jelinek EM, Bittersohl B, Martiny F, et al. The 8-plate versus physeal stapling for temporary hemiepiphyseodesis correcting genu valgum and genu varum: a retrospective analysis of thirty five patients. Int Orthop. 2012;36(3):599–605. doi: 10.1007/s00264-011-1369-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scott JE, Taor WS. The “small patella” syndrome. J Bone Joint Surg B. 1979;61:172–5. doi: 10.1302/0301-620X.61B2.438269. [DOI] [PubMed] [Google Scholar]
- 21.Van Huyssteen AL, Hendric MRG, Barnett AJ, Wakeley CJ, Eldridge JDJ. Cartilage-bone mismatch in the dysplastic trochlea: an MRI study. J Bone Joint Surg Br. 2006;88(5):688–91. doi: 10.1302/0301-620X.88B5.16866. [DOI] [PubMed] [Google Scholar]
- 22.Currarino G. Primary spondylolysis of the axis vertebra (C2) in three children, including one with pycnodysostosis. Pediatr Radiol. 1989;19(8):535–8. doi: 10.1007/BF02389566. [DOI] [PubMed] [Google Scholar]
- 23.Kaplan KM, Spivak JM, Bendo A. Embryology of the spine and associated congenital abnormalities. Spine J. 2005;5:564–76. doi: 10.1016/j.spinee.2004.10.044. [DOI] [PubMed] [Google Scholar]
- 24.Hamilton MG, Myles ST. Pediatric spinal injury: review of 174 hospital admissions. J Neurosurg. 1992;77:700–4. doi: 10.3171/jns.1992.77.5.0700. [DOI] [PubMed] [Google Scholar]
- 25.Kusumi K, Turnpenny P. Formation errors of the vertebral column. J Bone Joint Surg Am. 2007;89(Suppl 1):64–71. doi: 10.2106/JBJS.F.00486. [DOI] [PubMed] [Google Scholar]
- 26.Huynh A-M, Aubin C-E, Rajwani T, et al. Pedicle growth asymmetry as a cause of adolescent idiopathic scoliosis: a biomechanical stimulation study. Paper presented at: 11th Annual International Philip Zorab Symposium; Apr 3–5, 2006; Oxford, United Kingdom. [Google Scholar]
- 27.Gamble JG, Simmons SC, Freedman M. The symphysis pubis. Anatomic and pathologic considerations. Clin Orthop Relat Res. 1986;203:261–72. [PubMed] [Google Scholar]
- 28.Morrisy RT, Weinstein SL. Atlas of Pediatric Orthopedic Surgery. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- 29.Blount WP, Clarcke GR. The classic. Control of bone growth by epiphyseal stapling. A preliminary report. J Bone J Surg Clin Orthop. 1971;77:4–17. [PubMed] [Google Scholar]
- 30.Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 2007;27(3):253–9. doi: 10.1097/BPO.0b013e31803433a1. [DOI] [PubMed] [Google Scholar]