Abstract
During heat stress and dehydration, thermoregulation is partly suppressed to save body fluid and circulation. Drinking induces the recovery of thermoregulatory responses including sweating. Our objective is to investigate the effect of water temperature and voluntary drinking on the extent of the drinking-induced sweating. Six healthy subjects 23.7 ± 0.6 yr old and 80.7 ± 5.7 kg wt were dehydrated by performing mild exercise (ergometer cycling) in a hot and humid chamber (38-40°C, 20-28% relative humidity). After dehydration, subjects were allowed to drink water with temperatures of 5, 16, 26, 58°C on four separate days. The sweating rate was measured on the forehead area before and after drinking. Also, blood samples were collected during the experiments and plasma osmolality was measured. Sweating increased markedly just a few minutes after the onset of drinking. The rate of this response was lower in ingested water temperature of 5°C (0.43 ± 0.03 g, p = 0.000). Different intake occurred with different water temperatures (respectively 4.2, 6.4, 3.1, 1.8 ml/kg). Water at 16°C induced higher intake (6.4 ml/kg) together with lower sweating (0.54 ± 0.03 g), which can result in optimum level of hydration. Conclusion- When dehydrated subjects drink water with different temperatures, there are different sweating responses together with different voluntary intakes. According to our results, consuming 16°C water, cool tap water, could be suggested in dehydration.
Keywords: Drink temperature, perspiration, voluntary intake, thermoregulatory evaporation, drinking induced thermoregulatory responses
Introduction
During heat stress –either by heat exposure, exercise, or other physical activities and pressures– balancing and regulating thermal state, fluid state and circulation is an important challenge. Heat stress induces thermoregulatory responses including sweating, coetaneous vasodilatation and panting (in animals). These responses induce dehydration which can go beyond compensatability and impose cardiovascular strain. Therefore, when the central nervous system senses dehydration via hypovolemia and hyperosmolarity in dorsal preoptic region, it distributes inhibitory signals to effectors of the thermoregulatory responses, as if the ‘physiologic thermostat’ has been reset to a higher point and thus the body temperature rises [1-5]. Fluid intake (ingestion or even injection) ameliorates the dehydration and eliminates, at least partially, the inhibition of the thermoregulatory responses; so there are phenomena called ‘drinking induced thermoregulatory responses’ [6-8] and one of them is ‘drinking induced sweating’. This phenomenon was introduced in 1965 [9] and has been the stuff of various studies since then. It has been reported that drink temperature influences thermoregulatory responses [10-12] and one study has reported that drinking induced sweating rate is lower in lower drink temperatures [12]. But the studies in question have investigated the effects of forced hydration by instructing subjects to drink specific amounts of the beverages, which could be stressful, especially in higher temperatures, inducing sympathetic activity, and thus affecting sweating in an interfering way. We hypothesize that what happens naturally is that dehydrated subjects voluntarily drink different amounts of beverages with different temperatures [13-15] and their sweating response would result from reflex effects of both the amount of intake [18] and beverage temperature. So we have investigated and compared sweating response following different water temperatures when subjects drank their desired amounts.
Materials and methods
Subjects
Six healthy male volunteers, age 23.7 ± 0.6 years and weight 80.7 ± 5.7 kg participated in this study. The study was reviewed and approved by the Investigation Committee of Tabriz University of Medical Sciences. All subjects gave their informed written consent for their participation.
Procedure
Pretest instructions included eating a light lunch, refraining from drinking any beverage several hours before the experiment, and no exercise on the day of the experiments. Before each experiment, subjects entered a chamber and rested in the sitting position for 30 min at a thermoneutral temperature (28°C, 20-28% relative humidity (rh)). Body weight was measured with light clothing. After drawing a blood sample by venopuncture as the first control sample, subjects entered another chamber (38-40°C, 20-28% rh). They performed a mild exercise (ergometer cycling) by alternating 10-min rest and 20 min exercise periods for 60 min, then exercise continued for the last 30-min period to induce a reduction in total body weight through sweating. Total heat exposure time was 120 min. During heat exposure, subjects were under constant observation for indications of any inability to tolerate the experimental conditions (e.g., elevated heart rate, nausea or confusion).
After the cessation of exercise, subjects dried their body and their forehead, and were then weighed. An indwelling cannula was inserted into a large superficial vein in the forearm to collect free-flowing blood samples. Second control blood sample was drawn through the indwelling cannula. The first control blood sample compares the plasma concentrations of sodium before and after heat exposure while second control blood sample is considered as a control to compare them before and after drinking.
Before drinking (The point of 0 min in Figure 1), sweat rate was measured as control, then subjects were allowed to drink water at temperatures of 5, 16, 26 and 58°C in voluntary volumes. Blood samples were drawn through the indwelling cannula at the start of drinking (0 min) and at 3, 9, 12, and 15 minutes after drinking.
Figure 1.
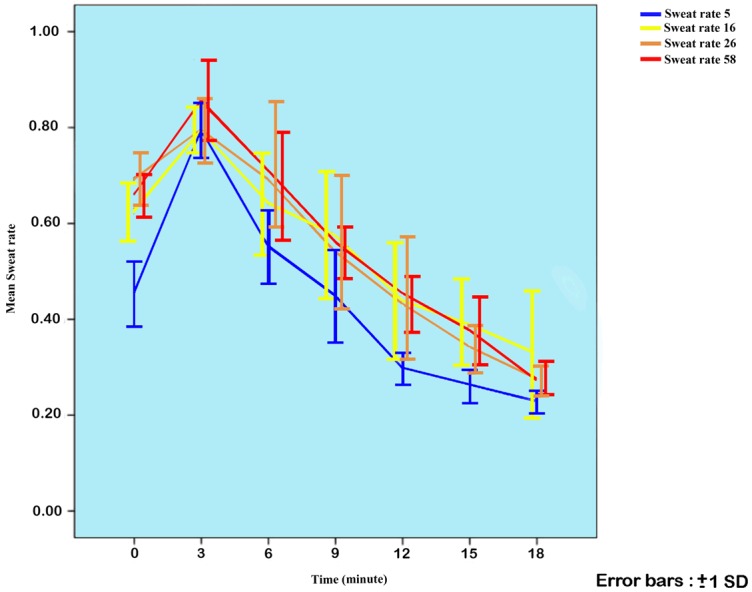
Sweat rates during trials with different water temperatures shown as mean ± SD. The point of 0 min represents the time of drinking. Error bars have been moved slightly to be discriminated.
Measurements
Forehead sweat rate was chosen to represent a localized area of sweating and was measured by the weight gain of a covered filter paper disk (96 cm²) placed on the skin over the forehead. The front sides of the disks were covered with waterproof tape to prevent evaporation. The disk was left on the skin each 3 minutes. It was enough to reliably detect weight gain and for saturation of the filter paper. The weight of a filter paper disk was gauged using EK-500 G beam balance, accurate to ± 0.01 g. Body weight was measured using a Secca beam balance, accurate to ± 100 g. As a result of experimental conditions, a decrease in weight primarily reflects water loss by thermoregulatory responses, mainly sweating.
Plasma sodium concentration was determined by Eppendorf flame photometry (model EFOX 5054, Instrumentation Laboratory). Sodium concentrations were measured as milliequivalents per kilogram of water by correcting for total solids. Because sodium and its associated anions account for about 94 percent of the solute in the extracellular compartment (including plasma), plasma osmolality can be roughly approximated as:
Posm = 2.1 * Plasma sodium concentration [16].
We applied this formula for the estimation of plasma osmolality from plasma sodium concentration.
Statistics
Data were analyzed by SPSS16. The difference in variables was assessed using paired t test (one measurement) and repeated measures analysis of variance (multiple measurements). Values of P<0.05 were considered statistically significant, and all data are presented as means ± SD.
Results
Subjects became dehydrated (2.37 ± 0.08% reduction of initial body weight which accords 24.3 ± 1.2 ml/kg), therefore, and as plasma assessments showed, a highly significant (P = 0.000 and 0.001) rise occurred in Posm and then no significant change in Posm occurred up to 15 min after drinking. The Posm changes did not differ statistically on different days. Plasma osmolalities of subjects during the experiments are shown in Table 1.
Table 1.
Plasma osmolality (mosmol/kg H2O) of subjects while they drink water with different temperatures
| Experiment type | intake (ml/kg) | Posm before procedure | Posm 3 min before drinking | Posm 15 min after drinking |
|---|---|---|---|---|
| Drinking 5°C water | 4.2 (0.1) | 297.50 (3.16) | 304.50 (3.25) | 314.15 (1.58) |
| Drinking 16°C water | 6.4 (0.2) | 308.00 (2.54) | 313.25 (3.62) | 312.55 (3.09) |
| Drinking 26°C water | 3.1 (0.1) | 306.25 (1.58) | 313.60 (4.54) | 311.50 (3.91) |
| Drinking 58°C water | 1.8 (0.1) | 305.90 (3.43) | 315.00 (5.48) | 313.25 (4.08) |
Sweating rates in different water temperatures are shown in Figure 1. Maximum sweating in all temperatures occurred 3minutes after drinking, which was significantly more than the rate in the time of drinking (p = 0.000). As illustrated in Figure 1, the 58°C trial showed higher sweat rate at this point (0.86 ± 0.04 g). Total sweat rate of the 5°C trial was statistically lower compared to the other trials, and the difference was highly significant (mean: 0.43 ± 0.03 g, P = 0.000). Sweat rate of other trials were not statically different.
Discussion
We tested the effect of ingested water temperature on the extent of rehydration induced sweating response, assessing both the effect of different water temperatures and different water volumes (due to various voluntary intakes). The temperatures were defined by subjects as cold (5°C), cool (16°C), tepid (26°C) and warm (58°C). Therefore the investigation tested the effect of these senses on the sweating response. These temperatures are commonly used in daily life as refrigerated water (5°C), cool tap water (16°C), water approximately at room temperature (26°C), and water at the temperature of a hot drink e.g. coffee (58°C).
Our results indicated that sweating was aggravated significantly in all subjects within the first 3 minutes after drinking, and this thermoregulatory response varied according to ingested water temperature; being the lowest in trial of cold water (5°C) compared with other trials. The sweating rate did not differ statistically in other trials. It has been reported that compared to ingestion of warm water (38°C), cold water (0.5°C) attenuates the increments in sweat rate of the whole body and the forearm (local), but in the case of cool water this reduction was true just for the whole body sweating and not for the local one [12]. As our measurement defined the localized sweat rate (forehead), similar to the study mentioned, cold water (5°C) induced significantly lower increments in sweat rate but cool water did not. Studies have shown that when dehydrated subjects intake fluid, their core temperature declines and the ultimate temperature is not influenced by the temperature of beverage, but colder water induces faster correction of core temperature [10-12]. In practice, cold drink acts as a heat sink [17], thus there is lower need for heat dissipation, and less sweating. Also for warmer drinks, it has been demonstrated that although some heat load is imposed to the subject, due to appropriate thermoregulatory reflexes, the core temperature is adjusted properly [10-12], and one of these reflexes, as we have described here, is higher drinking-induced sweating. It seems, in Figure 1, that the sweating rate at the peak point (3 min after drinking) is higher in 58°C water, but the difference was not statistically significant. Measuring whole body sweating and also forced hydration and higher intake of warm water would probably result in significant differences of sweat rate on this score.
The abrupt sweating response to drinking (within 3 min of the beginning of drinking), before any considerable change in plasma osmolality indicates that an osmotic signal acting on the brain via the blood osmoreceptors cannot account for the rapid onset of sweating [5]. Therefore some signals associated with the act of drinking, possibly from receptors in the oropharynx, could be involved in the recovery of thermoregulatory evaporation. These receptors appear to discriminate the temperature of received fluid as in thermoreceptors. Actually, as we sense the thermal content of what we drink, the physiological regulations of our body take it into account. Studies assessing drinking-induced thermoregulatory responses conclude that the phenomenon are not initiated by changes in plasma osmolality (Posm) or in blood volume and appear to depend upon oropharyngeal receptors [6,7,18-21].
The most useful application of researches about dehydration and drinking is about fluid balance in athletes [22] and soldiers [12,13]. Our results show 16°C water induces much more intake, meanwhile sweating response is much lower, and therefore the most efficient hydration occurs. So water temperature of 16°C could be recommended for consumption of dehydrated athletes and soldiers.
Conclusion
When dehydrated subjects drink water with different temperatures, the sweating response is influenced both by the water temperature and the volume of voluntary intake. The sweating response in cold water differs significantly compared to other water temperatures. Water temperature of 16°C, as in cool tap water, is the most optimum point for acquiring hydration in dehydrated athletes or other subjects.
Acknowledgements
We express our deep appreciation to our subjects who voluntarily participated in this experiment. We also make a point of our gratitude to Dr Y. Hadidi for agreeing to edit the English text of this paper. The current investigation was financially supported in the Drug Applied Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
Disclosure of conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Morimoto T, Itoh T. Thermoregulation and body fluid osmolality. J Basic Clin Physiol Pharmacol. 1998;9:51–72. doi: 10.1515/jbcpp.1998.9.1.51. [DOI] [PubMed] [Google Scholar]
- 2.Baldwin BA, Parrott RF. Autonomic thermoregulatory effects of electrical stimulation of the hypothalamus in the sheep (Ovis aries) Journal of Thermal Biology. 1984;9:279–284. [Google Scholar]
- 3.Brozmanova A, Jochem J, Javorka K, Zila I, Zwirska-Korczala K. Effects of diuretic-induced hypovolemia/isosmotic dehydration on cardiorespiratory responses to hyperthermia and its physical treatment in rabbits. Int J Hyperthermia. 2006;22:135–47. doi: 10.1080/02656730500531988. [DOI] [PubMed] [Google Scholar]
- 4.Gisolfi CV, Wenger CB. Temperature regulation during exercise: old concepts, new ideas. Exerc Sport Sci Rev. 1984;12:339–72. [PubMed] [Google Scholar]
- 5.Travis KA, Johnson AK. In vitro sensitivity of median preoptic neurons to angiotensin II, osmotic pressure, and temperature. Am J Physiol. 1993;264:R1200–5. doi: 10.1152/ajpregu.1993.264.6.R1200. [DOI] [PubMed] [Google Scholar]
- 6.McKinley MJ, Weissenborn F, Mathai ML. Drinking-induced thermoregulatory panting in rehydrated sheep: influences of oropharyngeal/ esophageal signals, core temperature, and thirst satiety. Am J Physiol Regul Integr Comp Physiol. 2009;296:R1881–8. doi: 10.1152/ajpregu.90890.2008. [DOI] [PubMed] [Google Scholar]
- 7.Takamata A, Mack GW, Gillen CM, Jozsi AC, Nadel ER. Osmoregulatory modulation of thermal sweating in humans: reflex effects of drinking. Am J Physiol. 1995;268:R414–22. doi: 10.1152/ajpregu.1995.268.2.R414. [DOI] [PubMed] [Google Scholar]
- 8.Libert JP, Candas V, Amoros C, Sagot JC, Lenzi P. Temperature regulation during intermittent exercise with progressive dehydration. Jpn J Physiol. 1986;36:253–66. doi: 10.2170/jjphysiol.36.253. [DOI] [PubMed] [Google Scholar]
- 9.Senay JRLC, Christensen ML. Cardiovascular and sweating response to water ingestion during dehydration. J Appl Physiol. 1965;20:975–979. doi: 10.1152/jappl.1965.20.5.975. [DOI] [PubMed] [Google Scholar]
- 10.Lee JK, Shirreffs SM. The influence of drink temperature on thermoregulatory responses during prolonged exercise in a moderate environment. J Sports Sci. 2007;25:975–85. doi: 10.1080/02640410600959947. [DOI] [PubMed] [Google Scholar]
- 11.Lee JKW, Maughan RJ, Shirreffs SM. The influence of serial feeding of drinks at different temperatures on thermoregulatory responses during cycling. J Sports Sci. 2008;26:583–590. doi: 10.1080/02640410701697388. [DOI] [PubMed] [Google Scholar]
- 12.Wimer GS, Lamb DR, Sherman WM, Swanson SC. Temperature of ingested water and thermoregulation during moderate-intensity exercise. Can J Appl Physiol. 1997;22:479–93. doi: 10.1139/h97-031. [DOI] [PubMed] [Google Scholar]
- 13.Sandick BL, Engell DB, Maller O. Perception of drinking water temperature and effects for humans after exercise. Physiol Behav. 1984;32:851–5. doi: 10.1016/0031-9384(84)90205-1. [DOI] [PubMed] [Google Scholar]
- 14.Szlyk PC, Sils IV, Francesconi RP, Hubbard RW, Armstrong LE. Effects of Water Temperature and Flavoring on Voluntary Dehydration in Men. Physiol Behav. 1989;45:639–47. doi: 10.1016/0031-9384(89)90085-1. [DOI] [PubMed] [Google Scholar]
- 15.Khamnei S, Hosseinlou A, Zamanlu M. Water temperature, voluntary drinking and fluid balance in dehydrated Taekwondo athletes. Journal of Sports Science and Medicine. 2011;10:718–724. [PMC free article] [PubMed] [Google Scholar]
- 16.Guyton A, Hall JE. Text book of medical physiology. Philadelphia: Elsevier Saunders; 2011. p. 358. [Google Scholar]
- 17.Butudom P, Barnes DJ, Davis MW, Nielsen BD, Eberhart SW, Schott HC 2nd. Rehydration fluid temperature affects voluntary drinking in horses dehydrated by furosemide administration and endurance exercise. Vet J. 2004;167:72–80. doi: 10.1016/s1090-0233(03)00054-6. [DOI] [PubMed] [Google Scholar]
- 18.Khamnei S, Hosseinlou A, Ibrahimi H. The Effect of Volume of Consumed Water on Drinking-Induced Sweating and Plasma Levels of Arginine Vasopressin, Epinephrine and Norepinephrine. International Journal of Endocrinology and Metabolism. 2004;2:19–28. [Google Scholar]
- 19.Thrasher TN, Nistal-Herrera JF, Keil LC, Ramsay DJ. Satiety and inhibition of vasopressin secretion after drinking in dehydrated dogs. Am J Physiol. 1981;240:E394–E401. doi: 10.1152/ajpendo.1981.240.4.E394. [DOI] [PubMed] [Google Scholar]
- 20.Baker MA. Effects of dehydration and rehydration on thermoregulatory sweating in goats. J Physiol. 1989;417:421–435. doi: 10.1113/jphysiol.1989.sp017810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Figaro MK, Mack GW. Regulation of fluid intake in dehydrated humans: role of oropharyngeal stimulation. Am J Physiol. 1997;272:R1740–6. doi: 10.1152/ajpregu.1997.272.6.R1740. [DOI] [PubMed] [Google Scholar]
- 22.Galloway SD. Dehydration, rehydration, and exercise in the heat: rehydration strategies for athletic competition. Can J Appl Physiol. 1999;24:188–200. doi: 10.1139/h99-016. [DOI] [PubMed] [Google Scholar]


