Abstract
Objectives: To explore a method of surface electrocardiogram for assessing cardiac dysfunction in patients with old myocardial infarction. Methods: 1000 patients with old myocardial infarction in Anzhen hospital were analyzed retrospectively. The planar QRS-T angle was calculated automatically according to QRS-wave and T-wave vectors by the electrocardiogram machine. Results: Among these 1000 patients, 822 (82.2%) were male and 178 (17.8%) were female, the mean age was 59.3±10.5 years (34~89 years). The average planar QRS-T angle was 88.5±50.6°. The planar QRS-T angle and LVEF was negative correlation (r=-0.406, p<0.01), the lower the LVEF, the better the relationship with planar QRS-T angle. QRS-T angle>90° had optimal sensitivity and specificity (76%, 74%) in diagnosis of cardiac dysfunction. Conclusion: The planar QRS-T angle and LVEF of patients with old myocardial infarction is negative correlation, the larger the planar QRS-T angle, the lower the LVEF. The planar QRS-T angle may be an easier and more feasible index for assessing cardiac dysfunction in patients with old myocardial infarction.
Keywords: Planar QRS-T angle, old myocardial infarction, cardiac dysfunction
Introduction
Left ventricular systolic function after Ml has been extensively studied and related to heart failure and cardiac mortality. Recent studies showed that spatial QRS-T angle, defined as the angle between the mean QRS and T vectors, is a strong independent predictor of incident coronary heart disease (CHD) and total mortality [1]. However, most clinicians are not familiar with measurement of the spatial QRS-T angle, and it is not routinely available in clinical electrocardiographic reports, which potentially limits wider use and validation of these reports. In contrast, the frontal plane axes of QRS and T are readily available in electrocardiographic reports printed by most current electrocardiographs, and these angles are understood and easily interpreted by clinicians.
This study retrospectively analyzed 1000 cases of old myocardial infarction patients’ planar QRS-T angle in order to give a value to the cardiac dysfunction.
Materials and methods
From this study, 1000 participants had complete electrocardiographic and clinical data available. The Simpson method was used to measure left ventricular ejection fraction (LVEF) by echocardiography. Identical electrocardiographs (Philips 300pi) were used and standard 12-lead ECGs were recorded for all subjects using strictly standardized procedures. All ECGs were processed in the central electrocardiograph laboratory. The machine measured the vector of QRS wave and T wave, and then, the angles between the two vectors (Planar QRS-T Angle) were calculated.
Materials
1000 patients with old myocardial infarction in Anzhen hospital were analyzed retrospectively. The old myocardial infarction was defined as at least 6 months after he or she suffered acute myocardial infarction with pathologic Q wave at least in two adjust ECG leads. Exclusion criterion included cardiac valve dysfunction, pulmonary heart disease, congenital heart disease, infectious endocarditis, pericardial disease, acute left cardiac dysfunction, arrhythmia and left or right complete bundle branch block (QRS duration ≥120 ms).
Statistical analysis
Statistical analysis was performed using SPSS16. The measured data are reported as mean±SD and analyzed using independent samples t-test. Categorical data are expressed as a percentage count (%), using x2 test to compare the two groups. The cutpoint can be established by receiver operating characteristic curve (ROC), false positive rate (1-specificity) as x-coordinate, and sensitivity as Y-coordinate. Partial correlation analysis was used to deal with the correlation of LVEF and planar QRS-T angle. p<0.05 means significant difference; p<0.01 means extremely difference.
Results
Baseline characteristics
Of the 1000 cases of old myocardial infarction patients, 822 cases were male (82.2%) and 178 cases were female (17.8%) (Table 1). The average age of these patients was 59.3±10.5 (between 34 to 89 years). 485 cases had anterior myocardial infarction (48.5%); 475 cases had inferior myocardial infarction (47.5%); 554 cases complicated with hypertension (55.4%); 309 cases with diabetes mellitus (30.9%); 434 cases with dyslipidemia (43.4%); 581 cases were smokers (58.1%).
Table 1.
Baseline Characteristics of patients
| Baseline Characteristics | All patients (n=1000) | Planar QRS-T angle≤90 (n=388) | QRS-T angle>90 (n=612) |
|---|---|---|---|
| Age | 59.3±10.5 | 58.6±10.8 | 60.6±10.0** |
| Male (%) | 822 (82.2) | 323 (82.7) | 499 (81.5) |
| QRSD (ms) | 91.4±15.3 | 89.8±14.6 | 94.3±16.1* |
| Hypertension n (%) | 554 (55.4) | 207 (53.4) | 347 (56.7)* |
| DM n (%) | 309 (30.9) | 113 (33.4) | 246 (29.2)** |
| Dyslipdemia n (%) | 434 (43.3) | 179 (46.1) | 254 (41.5) |
| Smoking history n (%) | 580 (58.0) | 222 (57.2) | 358 (58.5) |
| Anterior MI n (%) | 485 (48.5) | 165 (42.5) | 320 (52.3)* |
| Interior MI n (%) | 475 (47.5) | 204 (52.6) | 271 (44.3)* |
Notes: Compared with group whose planar QRS-T angle≤90;
P<0.05;
P<0.01.
The average QRS-T angle of patients in this group was 88.5°±50.6°. Patients with QRS-T angle≤90° were 338 cases, and patients with QRS-T angle>90° were 612 cases.
The correlation between QRS-T angle and LVEF value
The average LVEF value was 54.2±12.3%. According to LVEF, we divided the patients into two groups: cardiac dysfunctional group (LVEF<50%, n=297) and normal cardiac functional group (LVEF≥50%, n=703). Shown in Table 2, the average LVEF value of cardiac dysfunctional group is 38.5±6.8%, and the average LVEF value of normal cardiac functional group is 60.8±7.1%.
Table 2.
Correlation analysis of planar QRS-T angle and each LVEF
| LVEF≥50% | LVEF<50% | LVEF≤35% | |
|---|---|---|---|
| LVEF | 60.8±7.1 | 38.5±6.8 | 29.1±3.9 |
| The average of planar QRS-T angle | 72.5±43.4 | 126.4±46.3 | 146.3±33.7 |
| Correlation coefficient r | -0.031 | -0.466 | -0.484 |
| P value | <0.01 | <0.01 | <0.01 |
Through the partial correlation analysis, the influence of other factors (for example age, hypertension, diabetes, dyslipidemia and so on complicated disease) was excluded, the planar QRS-T angle and the LVEF value are negative correlations, correlation coefficient r=-0.406, p<0.01; when LVEF≥50%, correlation coefficient r=-0.031, P<0.01; when LVEF<50%, correlation coefficient r=-0.466, P<0.01; when LVEF value ≤35%, correlation coefficient r=-0.484, P<0.01. In patients with LVEF<50%, the planar QRS-T angle increases every 13.8°, LVEF reduces 5%.
The cutpoint of planar QRS-T angle diagnosing LVEF reducing
We respectively took planar QRS-T angle>80°, >90°, >100° as the diagnosis cutpoint, calculated the sensitivity, specificity and the false positive rate. According to the sensitivity and the false positive rate of every cutpoint, the ROC curve was planned and statistical analysis was carried on in Table 3. The sensitivity of planar QRS-T angle>90° is 76%, the specificity is 74%, Youden Index (YI) is 0.45, the Area Under Curve (AUC) is 0.72 (P<0.01). Compared with the group of planar QRS-T angle>90°, the sensitivity, the specificity, Youden Index, the Area Under Curve of the planar QRS-T angle>80° and >100° is obviously lower.
Table 3.
The sensitivity, the specificity, Youden Index, AUC, 95% confidence interval of each cutpoint
| Planar QRS-T angle | Sensitivity (%) | Specificity (%) | Youden index | False positiverate (%) | AUC | P value | 95% confidence interval |
|---|---|---|---|---|---|---|---|
| >80° | 63 | 69 | 0.37 | 31 | 0.27 | <0.001 | 0.235-0.303 |
| >90° | 76 | 74 | 0.45 | 26 | 0.72 | <0.001 | 0.681-0.753 |
| >100° | 56 | 81 | 0.37 | 19 | 0.31 | <0.001 | 0.270-0.345 |
Notes: AUC=Area under curve.
Discussion
Left ventricular systolic function after Ml has been extensively studied and related to heart failure and cardiac mortality [1]. Myocardium with cardiac dysfunction induces variation of depolarization and repolarization, for example, QRS prolongation, ST-T alteration, but these changes don’t have specificity.
More recently, there was increasing interest in evaluation of the prognostic value of the spatial angle between the QRS and T vectors [2]. A large QRS-T angle reflects an abnormal sequence of ventricular repolarization. Recently, Kors et al [3] showed that spatial QRS-T angle was a strong and independent predictor of cardiac death and total mortality in 6,134 men and women aged ≥55 years from the Rotterdam Study in The Netherlands. More recently, Rautaharju et al [4] evaluated the predictive value the spatial QRS-T angle in 38,283 women in the Women’s Health Initiative Study and showed that a wide spatial QRS-T angle was the strongest predictor of incident CHD events and total mortality.
The calculation of the spatial QRS-T angle requires availability of the orthogonal or at least quasi orthogonal X, Y and Z leads. Compared with planar QRS-T angle, the spatial QRS-T angle is a 3-dimensional space marker, complex calculation, requires dedicated software that is not widely available and cannot be derived by visual ECG analysis after acquisition. The planar QRS-T angle was defined as the angle between the maximum QRS and T-wave vectors in the frontal plane (Figure 1).
Figure 1.
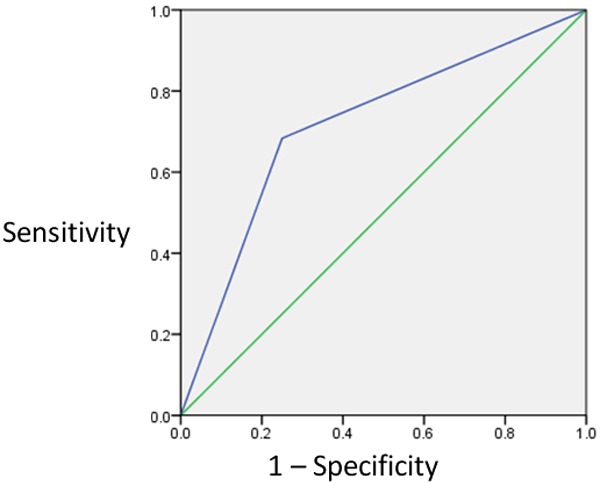
ROC of planar QRS-T angle>90°.
Although spatial QRS-T angle could be incorporated in electrocardiographic reports by modern computer-based electrocardiograph machines, it is currently not generally available and most clinical users are not familiar with this measurement. In contrast, QRS and T axes are routinely reported, and the frontal plane QRS-T angle can be easily calculated from them. Both QRS-T angles were significant when considered jointly; therefore, frontal plane QRS-T angle gives additional information and is a convenient substitute for spatial QRS-T angle for identification of increased risk of incident CHD and death.
Recent studies have demonstrated that the planar QRS-T angle as an easily derived risk measure is a suitable clinical substitute for the spatial QRS-T angle for risk prediction [5,6]. Recently, Zhang et al [7] evaluated the predictive value of the spatial QRS-T angle in 13,973 participants from the Atherosclerosis Risk In Communities Study, The median follow-up time was 14.3 years, everyone has high-risk factor of atherosclerosis, for example hypertension, diabetes and so on. The primary end point include incident CHD events and all-cause mortality. It demonstrated that the planar QRS-T angle has the same predictive value with the spatial QRS-T angle for incident CHD. We can easily obtain the planar QRS-T angle from a standard 12-lead ECG by visual examination and don’t have profound cardiac electrophysiological knowledge, heart rate are very few influences for its measurement, and has high accuracy and good repeatability.
About the normal range of planar QRS-T angle, generally, a planar QRS-T angle<45° has been described normal, and a planar QRS-T angles>45° to 60° has been considered as abnormal, but may be present in specialized athlete or hypertension patients [8-11]. This article took planar QRS-T angle>90° as abnormal.
Through the partial correlation analysis, the results demonstrated that the planar QRS-T angle and LVEF of patients with old myocardial infarction is negative correlation, the larger the planar QRS-T angle is, the lower the LVEF is. When LVEF<50%, the planar QRS-T angle increases every time 13.8°, LVEF reduces 5%. This result is concord with international documents about the planar QRS-T angle. Behzad et al [2] selected 455 patients with nonischemic dilated cardiomyopathy in the DEFINITE trial, analyzed that the planar QRS-T angle was a significant predictor of a composite of death, appropriate ICD shock (in the group randomized to ICD), or resuscitated cardiac arrest (HR, 1.05 for each 10° increase in QRS-T angle; P=0.013), the cardiac function is worse, the planar QRS-T angle is larger. With the improvement of cardiac function, the planar QRS-T angle decreases gradually, from NYHA III/IV to NYHA I. This study also showed that the planar QRS-T angle has closely relation with LVEF, the QRS duration. LVEF decrease 5% between the LVEF range of 30% to 40%, the QRS-T angle widened 5° (P<0.001). The QRS duration increases 10 ms, the QRS-T angle widens 6±1.3° (P<0.001).
Through the ROC curve analysis in our study, the planar QRS-T angle>90° has the best sensitivity and specificity for diagnosing of LVEF decreasing in patients with myocardial infarction. The planar QRS-T angle and LVEF of patients with old myocardial infarction are negative correlation, the larger the planar QRS-T angle, the lower the LVEF. The planar QRS-T angle may be an easy and feasible index for assessing cardiac dysfunction in patients with old myocardial infarction.
Acknowledgements
This study is funded by High Level Health Technical Personnel Training Plan (2009-3-48) of Beijing Health Bureau.
Disclosure of conflict of interest
None.
References
- 1.Scherptong RW, Henkens IR, Man SC, Le Cessie S, Vliegen HW, Draisma HH, Maan AC, Schalij MJ, Swenne CA. Normal limits of the spatial QRS-T angle and ventricular gradient in 12-lead electrocardiograms of young adults: dependence on sex and heart rate. J Electrocardiol. 2008;41:648–655. doi: 10.1016/j.jelectrocard.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 2.Pavri BB, Hillis MB, Subacius H, Brumberg GE, Schaechter A, Levine JH, Kadish A. Prognostic value and temporal behavior of the planar QRS-T angle in patients with nonischemic cardiomyopathy. Circulation. 2008;117:3181–3186. doi: 10.1161/CIRCULATIONAHA.107.733451. [DOI] [PubMed] [Google Scholar]
- 3.Kors JA, Kardys I, van der Meer IM, van Herpen G, Hofman A, van der Kuip DA, Witteman JC. Spatial QRS-T angle as a risk indicator of cardiac death in an elderly population. J Electrocardio. 2003;36(Suppl):113–4. doi: 10.1016/j.jelectrocard.2003.09.033. [DOI] [PubMed] [Google Scholar]
- 4.Rautaharju PM, Kooperberg C, Larson JC, LaCroix A. Electrocardiographic predictors of incident congestive heart failure and all-cause mortality in postmenopausal women: the Women’s Health Initiative. Circulation. 2006;113:481–489. doi: 10.1161/CIRCULATIONAHA.105.537415. [DOI] [PubMed] [Google Scholar]
- 5.Sur S, Han L, Tereshchenko LG. Comparison of sum absolute QRST integral, and temporal variability in depolarization and repolarization, measured by dynamic vectorcardiography approach, in healthy men and women. PLoS One. 2013;8:e57175. doi: 10.1371/journal.pone.0057175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tereshchenko LG, McNitt S, Han L, Berger RD, Zareba W. ECG maker of adverse electrical remodeling post-myocardial infarction predicts outcomes in MADIT II study. PLoS One. 2012;7:e51812. doi: 10.1371/journal.pone.0051812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang ZM, Prineas RJ, Case D, Soliman EZ, Rautaharju PM. Comparison of the prognostic significance of the electrocardiographic QRS/T angles in predicting incident coronary heart disease and total mortality (from the atherosclerosis risk in communities study) Am J Cardiol. 2007;100:844–849. doi: 10.1016/j.amjcard.2007.03.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wagner GS. Marriott’s Practical Electrocardiography. 10th edition. Baltimore, Md: Lippincott Williams & Wilkins; 2001. p. 60. [Google Scholar]
- 9.Herweg B, Fisher JD, Ilercil A, Martinez MR, Gross JN, Kim SG, Ferrick KJ. Cardiac memory after radiofrequency ablation of accessory pathways: the post-ablation T wave does not forget the pre-excited QRS. J Intervent Card Electrophysiol. 1999;3:263–272. doi: 10.1023/a:1009816228345. [DOI] [PubMed] [Google Scholar]
- 10.Malik M, Hnatkova K, Batchvarov VN. Post infarction risk stratification using the 3-D angle between QRS complex and T-wave vectors. J Electrocardiol. 2004;37(Suppl):201–208. doi: 10.1016/j.jelectrocard.2004.08.058. [DOI] [PubMed] [Google Scholar]
- 11.Hingra R, Ho Nam B, Benjamin EJ, Wang TJ, Larson MG, D’Agostino RB Sr, Levy D, Vasan RS. Cross 2 sectional relations of electrocardiographic QRS duration to left ventricular dimensions: the Framingham Heart Study. J Am Coll Cardiol. 2005;45:685. doi: 10.1016/j.jacc.2004.11.046. [DOI] [PubMed] [Google Scholar]


