Abstract
Sudden sensorineural hearing loss (SSNHL) is usually unilateral and can be associated with tinnitus and vertigo. The most common causes of this disease are known to be the vascular and viral agents, but immune disorders are involved in the development of sudden deafness. The antiphospholipid syndrome (APS) is an acquired autoimmune system disorder, which is defined as the presence of antiphospholipid antibodies (APA) in the patient’s blood, then cause venous and/or arterial thrombosis in various organs of the body, for example, thrombosis can occur in the placenta and/or the inner ear. As a result, it can cause abortion and/or sudden deafness. Bilateral SSNHL following habitual abortion is a rare clinical event. Here, we report a case of 32-year-old woman who presented with bilateral sudden hearing loss following recurrent pregnancy loss (RPL) as the first manifestation of primary antiphospholipid syndrome. Combine the literature, the diagnosis, clinical implication and treatment are discussed.
Keywords: Sudden sensorineural hearing loss (SSNHL), autoimmune disease, habitual abortion, recurrent pregnancy loss (RPL), antiphospholipid syndrome (APS), antiphospholipid antibody (APA), anticardiolipin antibody (ACA), thrombosis
Introduction
The etiology of sudden sensorineural hearing loss (SSNHL) is still unknown [1], the most common causes are known to be the vascular and viral agents, but autoimmune disorders are involved in the development of sudden deafness [2]. The antiphospholipid syndrome (APS) is an autoimmune diseases, and APS can cause arterial or venous blood clots in various organ system, or pregnancy-related complications [3,4]. The disease can be associated with antiphospholipid antibodies (APA) or anticardiolipin antibody (ACA), which manifests with tissue and cellular alterations due to the deposition of antibodies and pathogenic immune complexes, a disorder of recurrent vascular thrombosis and thrombocytopenia associated with a persistent anticardiolipin test positivity [4,5]. Therefore, APS can cause thrombosis of the placenta and/or the inner ear vessels, and subsequent lead to abortion and/or sudden deafness.
Bilateral SSNHL following habitual abortion is a rare clinical event with poor prognosis. In this report, we describe the case of a young pregnant woman affected by recurrent pregnancy loss (RPL) and positive for ACA who was brought to our observation for a bilateral SSNHL. The relevant literature, diagnosis, clinical implication and treatment are discussed.
Case report
A 32-year-old Chinese woman, G4P0, with a remarkable past history of “habitual abortion” and “suspicious connective tissue diseases”, was admitted in the Department of Otolaryngology of Second Xiangya Hospital with the complaint of bilateral sudden deafness for 20 days. The patient was a primigravida, she was diagnosed as “intrauterine fetal death” at 16 weeks of gestation, and she underwent a abortion surgery in the local hospital before 21 days. she complained of fever and headache 8 hours after the operation. The next day, she started to experience bilateral severe sudden deafness, tinnitus and vertigo. Pure tone audiometry revealed a bilateral profound sensorineural hearing loss. She was admitted to the department of hematology and otolaryngology in the local hospital for internal medicine intervention,After 20 days therapy, her other symptoms were only slightly improved except for fever and headache, then she was transferred to our hospital for a further treatment. The patient has no genetic or allergic history.
After admitted to hospital, complete blood count revealed WBC 11.2 × 109/L (reference 4.0~10.0), RBC 3.1 × 1012/L (reference 3.5~5.0), HGB 95 g/L (reference 110~150) and platelet (PLT) 89 × 109/L (reference 100~300), erythrocyte sedimentation rate (ESR) was 28 mm/h (reference < 20). Blood coagulation function test showed activated partial thromboplastin time (APTT) 1.76 g/L (reference 0.80~1.20) and D-dimer was positive. ACA-IgG detection by ELISA was positive (30 IU/mL). Serological investigations showed positive to antinuclear antibody (ANA) (from 1:80~1:320), but anti-neutrophil cytoplasm antibody (ANCA) was negative. Coombs test was positive. Anti HIV and Widal reaction was negative. The bone marrow aspiration excluded a proliferative disease of the hematopoietic or lymphatic system. Determination of immunoglobulin was normal. General and neurologic examinations were normal except bilateral severe sudden sensorineural hearing loss. The bilateral external auditory canal and tympanic membranes were normal. Pure tone audiometry confirmed profound deafness in both ears (Figure 1). Auditory brainstem response (ABR) revealed 91 decibels (dB) hearing loss affecting bilateral ears, with normal waveforms at 100 dB sound pressure level. The tympanometry showed a normal tympanogram of Type A. Chest radiograph showed a mild pulmonary infection. ECG, the abdomen and blood vessels colour B-ultrasonography were normal. Cranial and temporal bone computed tomographic scan (CT) and magnetic resonance imaging (MRI) examination had no obvious abnormality.
Figure 1.
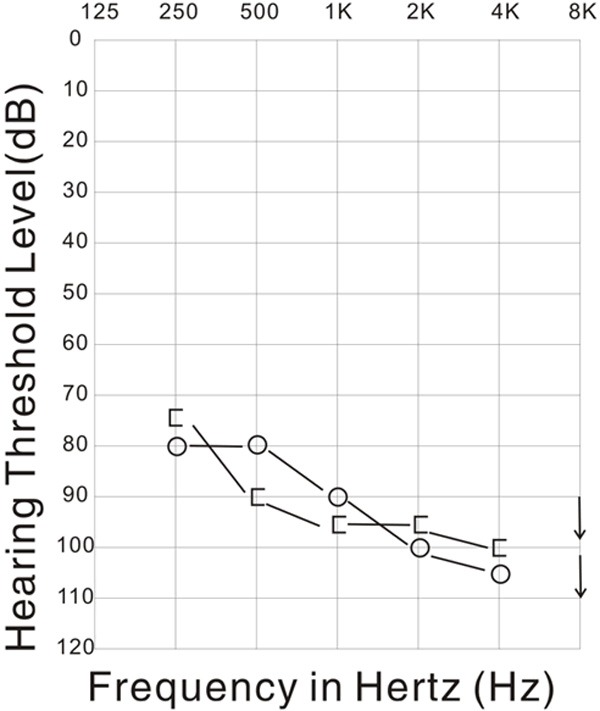
Audiogram showed profound sensorineural hearing loss in the right ear (○) and left ear (□).
The diagnosis of bilateral SSNHL was made, and other diagnosis were considered on the basis of these findings, including APS, habitual abortion and coagulant function abnormality. Warfarin (4 mg/day) and low molecular heparin (0.4 mL/day for 3 days) were used for anticoagulate. At the same time, dexamethasone (10 mg/day) was used for 3 days by intravenous and hyperbaric oxygen therapy. Warfarin therapy for this disease was both efficient and safe when INR (International normalization ratio) maintained between 1.8~2.5. Mean hearing thresholds were expressed as the average of the 0.5-, 1.0-, 2.0- and 4.0-kHz hearing thresholds (4-tone average). However, there was no obvious improvement of the hearing loss after 1 week treatment. Therefore, we changed the treatment plan: with intratympanic dexamethasone (ITD) [6,7]. This procedure was carried out 5 times, every other day, with a total dexamethasone dose of 10 mg. Her bilateral hearing improved significantly after 2 months, audiogram (4-tone average) prompted about hearing loss of 73 dB (right ear) and 75 dB (left ear) (Figure 2). No other ischemic attack, any systemic findings or audiovestibular complaint have been seen for 2 years, and she had been wearing digital hearing aids.
Figure 2.
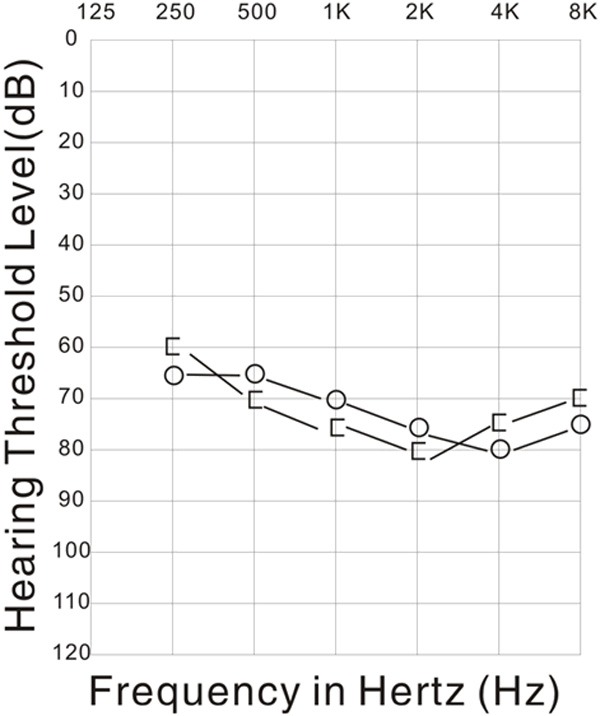
Audiogram showed hearing improved after treatment, hearing threshold is 73 dB in the right ear (○) and 75 dB in the left ear (□).
Discussion
Recurrent pregnancy loss (RPL) or habitual abortion is that the occurrence of 3 or more pregnancies end in miscarriage of the fetus at the same time before viability, It affects about 1% of the child-bearing population and presents couples with this disorder a formidable challenge in successfully having a family [8]. There are 3 main causes for RPL: chromosome disease, reproductive factors and immune factors [9,10]. APS is a condition defined by the presence of abnormal antibodies and a tendency to form blood clots or to have miscarriages. APS occurs in isolation (primary APS) or in association with another immune disorder (secondary APS), such as lupus, an infection or the use of a medication, particularly systemic lupus erythematosus [11,12].
SSNHL has been defined as sensorineural hearing loss of at least 30 dB over at least 3 contiguous audiometric frequencies, occurring over an interval of less than 3 days [13]. It is usually unilateral and can be associated with tinnitus and vertigo. In most cases the pathogenesis of SSNHL remains an enigma [1], although various infective, vascular, and immune causes have been proposed [12,14,15]. This is mainly because a direct investigation of labyrinthine tissue in the patient is not yet possible without permanent damage of the inner ear. Therefore, indirect diagnostic tools such serologic testing for different agents are used to unravel the cause of SSNHL [3,16]. Now, a series of studies have confirmed that SSNHL can be associated with autoimmune diseases [5]. Many otologic research activities has focused on the role of autoantibodies against antigens of labyrinthine tissue, which are assumed to play an important role in SSNHL [3,11].
Bilateral SSNHL following habitual abortion is a rare event. Here, we report a case with primary APS who had bilateral SSNHL. The patient’s symptoms are bilateral sudden deafness, tinnitus, fever and headache after the operation of habitual abortion. Blood examination reveal APTT is prolonged and PLT is decreased, serological investigation show positive to ACA-IgG and ANA, while negative to p-ANCN. Unlike previous reports, our patients meet the criteria for primary APS, because there are no clinical and serologic evidences that SLE or other autoimmune disease ever happened. In 1998, Hishashi et al. firstly reported the association of SSNHL and ACA in a patient [11,17]. However, the pathogenic role of APA in the development of thrombosis has not been fully elucidated. Studies have shown that ACA and β2-glycoprotein (β2GPI) can be produced in the process of thrombosis, while β2GPI is a “natural anticoagulant”, and APA can neutralize β2GPI and leads to thrombosis [3,5,18]. The thrombi generally occur in large veins and arteries, but any part of the vascular system may be affected. Hanly JG reported that arterial thrombosis involves the brain in up to 50% of cases, causing migraine-like headache, even transient ischemic attack or stroke [19], our patient also had the similar symptom of headache. In our case, the thrombi occur in small vascular of the placenta and the inner ear. Thrombosis of the placenta add APA or ACA, which in turn damage the placenta, both reasons subsequent lead to miscarriage, while thrombosis of the labyrinthine vessels subsequent damage the inner ear resulting in SSNHL [8-10].
The use of anticoagulant and antiplatelet should be considered without any delay. Treatment of hearing impairment in patients with autoimmune disorders is known to be a difficult problem. Intratympanic dexamethasone (ITD) injection as a salvage treatment demonstrate better results than systemic steroids reapplication or no salvage treatment in refractory SSNHL. ITD can be considered a valuable therapeutic option for SSNHL patients in whom traditional treatment failed [6,7,12].
In conclusion, we want to emphasize that SSNHL can be happened in RPL patient with primary APS. Our patient supports direct association between ACA and SSNHL, of course, further studies are necessary to determine how the entity of APA or ACA contributes to the prognosis or outcome of SSNHL.
Disclosure of conflict of interest
None.
References
- 1.Furuhashi A, Matsuda K, Asahi K, Nakashima T. Sudden deafness: long-term follow-up and recurrence. Clin Otolaryngol. 2002;27:458–463. doi: 10.1046/j.1365-2273.2002.00612.x. [DOI] [PubMed] [Google Scholar]
- 2.Toubi E, Ben-David J, Kessel A, Halas K, Sabo E, Luntz M. Immune-mediated disorders associated with idiopathic sudden sensorineural hearing loss. Ann Otol Rhinol Laryngol. 2004;113:445–449. doi: 10.1177/000348940411300605. [DOI] [PubMed] [Google Scholar]
- 3.Bachor E, Kremmer S, Kreuzfelder E, Jahnke K, Seidahmadi S. Antiphospholipid antibodies in patients with sensorineural hearing loss. Eur Arch Otorhinolaryngol. 2005;262:622–626. doi: 10.1007/s00405-004-0877-y. [DOI] [PubMed] [Google Scholar]
- 4.Tincani A, Bompane D, Danieli E, Doria A. Pregnancy, lupus and antiphospholipid syndrome (Hughes syndrome) Lupus. 2006;15:156–160. doi: 10.1191/0961203306lu2279rr. [DOI] [PubMed] [Google Scholar]
- 5.Bir LS, Eşmeli FO, Ardiç FN. Sudden sensorineural hearing loss in a patient with primary antiphospholipid syndrome. J Thromb Thrombolysis. 2006;21:277. doi: 10.1007/s11239-006-6156-6. [DOI] [PubMed] [Google Scholar]
- 6.Moon IS, Lee JD, Kim J, Hong SJ, Lee WS. Intratympanic dexamethasone is an effective method as a salvage treatment in refractory sudden hearing loss. Otol Neurotol. 2011;32:1432–1436. doi: 10.1097/MAO.0b013e318238fc43. [DOI] [PubMed] [Google Scholar]
- 7.Wang YW, Ren JH, Lu YD, Yin TF, Xie DH. Evaluation of intratympanic dexamethasone for treatment of refractory sudden sensorineural hearing loss. J Zhejiang Univ Sci B. 2012;13:203–208. doi: 10.1631/jzus.B1100248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kutteh WH. Recurrent pregnancy loss: an update. Curr Opin Obstet Gynecol. 1999;11:435–439. doi: 10.1097/00001703-199910000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Faussett MB, Branch DW. Autoimmunity and pregnancy loss. Semin Reprod Med. 2000;18:379–392. doi: 10.1055/s-2000-13728. [DOI] [PubMed] [Google Scholar]
- 10.Blank M, Shoenfeld Y. Antiphospholipid antibody-mediated reproductive failure in antiphospholipid syndrome. Clin Rev Allergy Immunol. 2010;38:141–147. doi: 10.1007/s12016-009-8146-x. [DOI] [PubMed] [Google Scholar]
- 11.Naarendorp M, Spiera H. Sudden sensorineural hearing loss in patients with systemic lupus erythematosus or lupus-like syndromes and antiphospholipid antibodies. J Rheumatol. 1998;25:589–592. [PubMed] [Google Scholar]
- 12.Haynes DS, O’Malley M, Cohen S, Watford K, Labadie RF. Intratympanic dexamethasone for sudden sensorineural hearing loss after failure of systemic therapy. Laryngoscope. 2007;117:3–15. doi: 10.1097/01.mlg.0000245058.11866.15. [DOI] [PubMed] [Google Scholar]
- 13.Wilson WR, Byl FM, Laird N. The Efficacy of Steroids in the Treatment of Idiopathic Sudden Hearing LossA Double-blind Clinical Study. Arch Otolaryngol. 1980;106:772–776. doi: 10.1001/archotol.1980.00790360050013. [DOI] [PubMed] [Google Scholar]
- 14.Ho HG, Lin HC, Shu MT, Yang CC, Tsai HT. Effectiveness of intratympanic dexamethasone injection in sudden-deafness patients as salvage treatment. Laryngoscope. 2004;114:1184–1189. doi: 10.1097/00005537-200407000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Aimoni C, Bianchini C, Borin M, Ciorba A, Fellin R, Martini A, Scanelli G, Volpato S. Diabetes, cardiovascular risk factors and idiopathic sudden sensorineural hearing loss: a case-control study. Audiol Neurootol. 2010;15:111–115. doi: 10.1159/000231636. [DOI] [PubMed] [Google Scholar]
- 16.Gagnebin J, Maire R. Infection Screening in Sudden and Progressive Idiopathic Sensorineural Hearing Loss: A Retrospective Study of 182 Cases. Otol Neurotol. 2002;23:160–162. doi: 10.1097/00129492-200203000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Wang JG, Xie QB, Yang NP, Yin G. Primary antiphospholipid antibody syndrome: a case with bilateral sudden sensorineural hearing loss. Rheumatol Int. 2009;29:467–468. doi: 10.1007/s00296-008-0696-3. [DOI] [PubMed] [Google Scholar]
- 18.Galli M, Luciani D, Bertolini G, Barbui T. Anti-beta 2-glycoprotein I, antiprothrombin antibodies, and the risk of thrombosis in the antiphospholipid syndrome. Blood. 2003;102:2717–2723. doi: 10.1182/blood-2002-11-3334. [DOI] [PubMed] [Google Scholar]
- 19.Hanly JG. Antiphospholipid Syndrome: An overview. CMAJ. 2003;168:1675–1682. [PMC free article] [PubMed] [Google Scholar]


