Introduction
Canada, admitting more than 200,000 new permanent residents every year, is a major destination for immigrants in the world. 266 These new immigrants have fewer chronic conditions and better health compared with the average for the Canadian-born population at the time of entry in the country - the healthy immigrant effect. 5, 116 However, as these immigrants are exposed to the physical, social, environmental and cultural effects of the new adopted country, they start losing this health advantage; the average health of immigrants’ starts becoming similar to the average health of the Canadian population - the convergence paradigm of acculturation. 4
Among the possible explanations for the adverse effects on health that lead to convergence is poor access to health care for new immigrants. Riedel has discussed three important types of barriers to health care access among immigrants: structural and institutional, financial, and personal and cultural. 131 However, while we can conceptually distinguish these barriers, in practice, things often do not operate singly. For instance, adjusting to a new country is in itself a stressful process, and understanding the inner workings of a new health care system can be even more challenging. This may be particularly true if individuals have arrived from a health care system vastly different than the one in the adopted country. These institutional and cultural barriers may be compounded by financial concerns, as it has also been shown that immigrants have lower income levels than the native born population on arrival, 9, 87 particularly if they are from developing countries. 88 Thus, upon immigration, economic stability may be a priority and these financial constraints may influence individual’s need for seeking health care. Further, personal beliefs, 140–141, 267 linguistic problems, 133, 268 and other cultural issues 142 may hamper health care access. A combination of these factors along with other barriers at the health-system level (e.g. racism) makes the visible minority immigrants particularly vulnerable for poor health access. 11, 132, 144, 269 However, as immigrants gradually ‘learn the ropes’ in the new society, their access should concomitantly improve. Thus, though immigrants may initially have lower access, it should potentially become similar to the Canadians over a period of time.
Previous research on health care access by immigrants in Canada has provided mixed results. While Laroche 203 did not find significant differences between health care utilisation by immigrants and Canadian-born adults, others have found differences between these populations, in both directions. For example, Wu and colleagues 230 found that immigrants had fewer unmet health care needs compared with the native born, and Newbold, 162 found greater use of health services by the immigrant population. In contrast, Wen and co-workers 159 found that immigrants, especially recent Asian immigrants, were less likely to report use of emergency services. Interestingly, Glazier and colleagues, 89 using the Census and administration data on hospitalizations in Toronto in 1996, found that hospital use and serious morbidity were highest in areas with high rates of recent immigration particularly in family class immigrants and refugees.
Study design may help explain some of these discrepancies. Indeed, the estimates for these analyses were primarily from cross-sectional data, pooled cross-sectional data, or the first event of health care utilisation. With time, however, the health care access may potentially change in individuals, particularly immigrants. However, the post-immigration changes may be experienced differently by male and female immigrants. 12, 200 Thus, a longitudinal design that accounts for these changes in individuals is therefore necessary to assess the differences in health care access of Canadians and immigrants over time.
To address these issues, we designed the present study to evaluate health care access over a 12-year period according to immigrant status in Canada (separately in males and females), and the socio-economic factors associated with it.
Methods
This study is a longitudinal analysis of secondary data originally collected by Statistics Canada as a part of the National Population Health Survey (NPHS). 228
Data Source
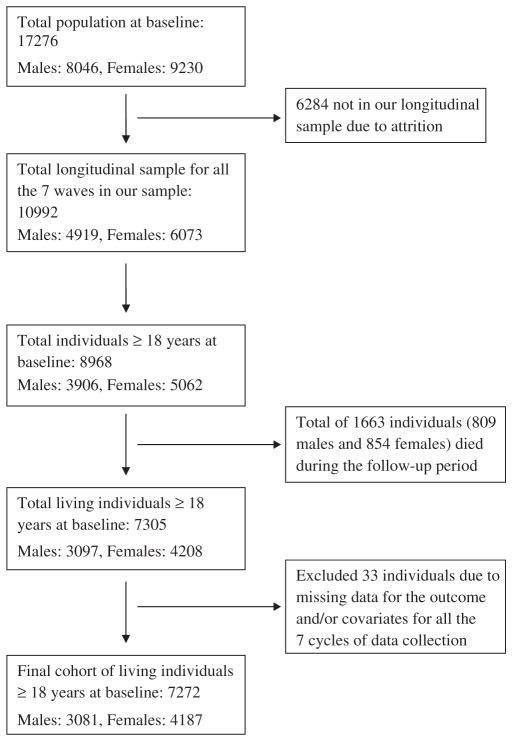
The target population for the NPHS was household residents of ten provinces in Canada; it excluded residents of health institutions, those living on the Canadian Forces bases, and those living on Indian Reserves and Crown lands and in remote areas of Ontario and Québec. Thus, it represents a nationally representative longitudinal survey of individuals, and provides information on social, demographic, economic, occupational, environmental, and health characteristics of these individuals. The first wave of data for NPHS was collected in 1994/95, and biennial surveys have been carried on since then, resulting in 12 years of follow-up (seven waves: 1994/95, 1996/97, 1998/99, 2000/01, 2002/03, 2004/5, and 2006/7). The households were selected in the first cycle (1994/95) and one individual above the age of 12 years was randomly selected from each household to be the longitudinal respondent for all the seven waves of the survey (they were traced for all the subsequent waves). The NPHS initial longitudinal panel composed of 17,276 individuals; the attrition rates (numbers) for cycles 1996/97, 1998/99, 2000/01, 2002/03, 2004/5, and 2006/7 (compared with the previous cycle) were 9.3% (1604), 6.6% (1041), 7.1% (1034), 7.6% (1038), 7.5% (940), and 5.4% (627) respectively. Thus, our initial longitudinal sample was of 10,992 individuals; of these 8968 were more than or equal to 18 years of age at baseline. We excluded 1663 individuals who died during the course of the follow-up and 33 individuals for whom there were no data for the variables included in the models in all the seven waves of data collection. Thus, a total of 3081 males and 4187 females were included for the present analysis (refer to as cohort for future discussion). We have described the details of the sample size in Figure 1. We had a total of 21567 observations (mean 6.3) for males and 29309 (mean 6.4) observations for females across the seven assessment times.
Figure 1.
The sample size for this study to assess the health-care access in Canadians according to immigrant status over a 12-year period, National Population Health Survey, Canada (1994–2006).
Outcomes
We used two measures of health care access as outcome variables: 1) whether or not the respondent had a regular doctor, 2) self-reported perceived unmet health care need in the past 12 months. Both outcomes were measured as binary indicators (yes/no). The independent variable of primary interest was the Canadian-born or immigrant status of the individual. Immigrants were further categorised as White and Non-white.
Independent variables
Based on the acculturation framework described by Berry, 10 we included the following socio-demographic independent variables in the statistical models: age (categorised as 18/34 years, 35/54 years, 55/74 years. ≥ 75 years), education (primary, secondary, post-secondary, and graduate), income adequacy category (classified by Statistics Canada into four categories according to the total household income and total number of individuals in the household as: highest, upper middle, lower middle, and lowest), living conditions (single, with a partner, family with both parents, family with single parent, and other types) marital status (single, married, separated [included widowed or divorced]), province of residence (Ontario, Québec, British Columbia, and others), and a binary indicator of linguistic minority (individuals living in Québec and unable to speak/understand French, individuals living in other provinces and unable to speak/understand English). The behavioural variables were: alcohol intake (never, regular, or former), smoking pattern (never, daily, occasional, or former), and physical activity (infrequent, occasional, and regular). In addition, presence of a chronic condition was used as a covariate in the models. For the unmet health care need outcome, we added ‘having a regular doctor’ as an explanatory variable in the model. A calendar ‘time’ variable measured in years since 1994 was also included in the models to account for the longitudinal changes across the seven cycles during the 12 year follow-up period. Finally, we estimated models that included only the immigrant sub-population to assess the effect of time since immigration on the health care access outcomes. Since ‘time-since-immigration’ would have had no value for Canadian born individuals, the variable could not be used in the models that included all the individuals.
Statistical Analyses
We stratified all analyses by gender. Descriptive statistics compared the frequency of reporting of the two outcome variables in the immigrant sub-groups, socio-demographic categories and distribution of lifestyle variables for each cycle of data.
We used random effects (RE) extensions of multiple logistic regression models to analyse this longitudinal dataset for repeated measures binary outcomes. RE models can estimate both within-individual and between-individual effects, accounting for correlation of the repeated outcomes in the same individual. 251 This is a better model than the conventional logistic regression models, which may underestimate variance from data with repeated within-subject measures over time. The RE models for the two health care access outcomes were built in the following sequence: 1) null model with no explanatory variables for level-2 residual variance (at the level of individuals in our study); 2) simple unifactorial models that yielded unadjusted estimates of association of the health care outcomes with each explanatory variable separately, and: 3) a complete model with all the variables. These RE models accounted for random intercepts i.e. for an individual’s systematically higher or lower probability of a specific outcome. We performed linear contrast tests across the four income categories. 270 This test assessed the trend of increased (or decreased) odds for these income categories. We also tested the interaction between immigrant status and ‘time’ to assess if the differences in health care outcomes between these three groups varied over the 12-year period of data collection. For each model, the intra-class correlation (ICC) was estimated using the formula described by Snijders and Bosker 251 (τ2/[τ2 + π2/3]); here, the τ2 represents the variance of the random intercept. The ICC indicates the proportion of variance explained by the group level; however, this definition may also indicate the intraclass correlation controlled for the effects of the independent variables as discussed by the authors. 251 We used the Akaike Information Criteria (AIC) to assess the fit of various logistic RE models (such as the null model, unifactorial models, and the complete model, model with interaction terms). 252
In our cohort about 91% of observations in males and in females had complete values, for all the variables included in these models. Among males, 7.8% observations had one, 0.5% had two, and 1.0% had between three and seven missing values; among females, 7.5% observations had one, 0.4% had two and 1.1% had between three and nine missing values. To account for missing information in the remaining 9% of observations, we performed 20 imputations of the dataset (using all seven waves), using the ‘Multiple Imputations with Chained Equations’ (MICE) method. 253–254 The difference of the estimates between the models with imputed values and the original analyses with missing data was < 0.5*standard error, for each of the primary independent variable of interest. Therefore, we are only reporting the results from the original analysis with missing data. Finally, we performed sensitivity analyses including males and females who had died during the course of data collection.
We used Stata (version 10) (StataCorp, College Station, Texas, USA) for all the analyses (xtlogit for the longitudinal data), including the imputations (using the ice command). 255–257
The study was approved by the Institutional Review Board of McGill University.
Results
Descriptive data
In our sample of 3081 males, 2703 (88%) were non-immigrants, 266 (9%) were white immigrants, and 112 (4%) were non-white immigrants. Among the 4187 females, 3696 (88%) were non-immigrants, 377 (9%) were white immigrants, and 114 (3%) were non-white immigrants. Among the 226 non-white immigrants; 34% were ethnically South Asian, 29% were ethnically Chinese, and 22% were ethnically Black. Certain baseline demographic characteristics of Canadian born individuals and immigrants are presented in Table 1.
Table 1.
Certain baseline demographic characteristics according to immigrant status in 3081 males and 4187 females (1994), Canada
| Characteristics | Canadian born (N = 6399) | White immigrants (N = 643) | Non-white immigrants (N = 226) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Mean age (SD), years | 42.8 (15.5) | 50.9 (15.3) | 39.8 (11.9) |
| Sex | |||
| Males | 2703 (42) | 266 (41) | 112 (50) |
| Females | 3696 (58) | 377 (59) | 114 (50) |
| Marital status | |||
| Single | 1335 (21) | 60 (9) | 49 (22) |
| Married | 4011 (63) | 448 (70) | 152 (67) |
| Separated* | 1053 (16) | 135 (21) | 25 (11) |
| Education | |||
| Primary | 1504 (24) | 131 (20) | 35 (16) |
| Secondary | 991 (15) | 102 (16) | 35 (16) |
| Postsecondary | 1684 (26) | 163 (25) | 55 (24) |
| Graduate | 2209 (35) | 247 (38) | 100 (44) |
| Missing | 11 (0.2) | 0 (0) | 1 (0.4) |
| Income adequacy category‡ | |||
| Highest | 888 (14) | 128 (21) | 21 (10) |
| Upper middle | 2393 (37) | 217 (35) | 77 (36) |
| Lower middle | 1798 (28) | 175 (29) | 72 (33) |
| Lowest | 1088 (17) | 93 (15) | 46 (21) |
| Missing | 232 (4) | 30 (5) | 10 (4) |
Includes widowed or divorced.
Income adequacy was according to the categorisation by Statistics Canada based on the total household income and number of people in the household.
Access to a regular doctor
The unadjusted estimates demonstrated higher odds of access to a regular doctor in male immigrants (white and non-white) and female white immigrants than for Canadian born individuals. However, after adjusting for all covariates, immigrant men and women (white and non-white) had similar odds of having a regular doctor as the Canadian born individuals. The estimates for the unifactorial and complete models are shown in Table 2. In general, men and women in higher age groups were more likely to have a regular doctor. Men in the lowest income category had a similar odds of having a regular doctor as those in highest income category (OR: 1.09, 95% CI: 0.84–1.42). In contrast, women in the lowest income category were less likely to have a regular doctor than those in the highest income category (OR: 0.66, 95% CI: 0.50 – 0.87); and the odds of having a regular doctor decreased with decreasing income (p < 0.001, for test of trend). Men and women living in the province of Québec had the lowest odds of access to a regular doctor.
Table 2.
Random effects models showing the unadjusted and adjusted estimates of odds ratios (OR) and their 95% confidence intervals (C.I.) for ‘having a regular doctor’ in 3081 males and 4187 females in Canada (1994–2006)
| Unadjusted estimates
|
Adjusted estimates
|
|||
|---|---|---|---|---|
| Males OR (95% C.I.) | Females OR (95% C.I.) | Males OR (95% C.I.) | Females OR (95% C.I.) | |
| Immigrant status | ||||
| Canadian born | Reference | Reference | Reference | Reference |
| White immigrants | 2.52 (1.69–3.76) | 1.91 (1.32–2.79) | 1.32 (0.89–1.94) | 1.14 (0.78. 1.66) |
| Non-white immigrants | 2.14 (1.19–3.64) | 1.61 (0.85–3.04) | 1.28 (0.73–2.23) | 1.23 (0.64–2.36) |
| Age categories (years) | ||||
| 18–34 | Reference | Reference | Reference | Reference |
| 35–54 | 2.61 (2.24–3.06) | 1.31 (1.10–1.55) | 2.25 (1.89–2.68) | 1.05 (0.87–1.27) |
| 55–74 | 6.94 (5.57–8.66) | 2.76 (2.20–3.46) | 6.58 (5.06–8.55) | 2.21 (1.69–2.91) |
| ≥ 75 | 7.27 (4.96–10.67) | 3.89 (2.73–5.51) | 11.36 (6.79–19.01) | 2.86 (1.85–4.42) |
| Time | 1.06 (1.05–1.07) | 1.04 (1.02–1.05) | 1.01 (0.99–1.02) | 1.00 (0.98–1.02) |
| Education | ||||
| Primary | Reference | Reference | Reference | Reference |
| Secondary | 0.86 (0.61–1.20) | 0.89 (0.65–1.24) | 1.10 (0.80–1.53) | 1.05 (0.75–1.46) |
| Postsecondary | 0.74 (0.56–0.97) | 0.79 (0.60–1.03) | 0.86 (0.66–1.13) | 0.88 (0.67–1.17) |
| Graduate | 0.75 (0.58–0.97) | 0.74 (0.57. 0.95) | 0.87 (0.66–1.13) | 0.80 (0.60–1.05) |
| Income category | ||||
| Highest | Reference | Reference | Reference | Reference |
| Upper middle | 0.84 (0.73–0.96) | 0.92 (0.77–1.10) | 1.06 (0.91–1.24) | 0.95 (0.79–1.13) |
| Lower middle | 0.65 (0.55–0.78) | 0.77 (0.63–0.94) | 0.89 (0.73–1.08) | 0.74 (0.59–0.92) |
| Lowest | 0.67 (0.53–0.85) | 0.70 (0.55–0.88) | 1.09 (0.84–1.42) | 0.66 (0.50–0.87)* |
| Marital status | ||||
| Single | Reference | Reference | Reference | Reference |
| Married | 2.54 (2.12–3.06) | 2.08 (1.69–2.55) | 1.36 (1.05–1.76) | 1.82 (1.34–2.48) |
| Separated | 1.58 (1.21–2.05) | 2.68 (2.08–3.45) | 1.01 (0.76–1.35) | 1.64 (1.24–2.17) |
| Province | ||||
| Other provinces | Reference | Reference | Reference | Reference |
| Ontario | 1.93 (1.52–2.47) | 2.06 (1.61–2.64) | 1.79 (1.40–2.28) | 1.82 (1.42–2.36) |
| Quebec | 0.37 (0.29–0.48) | 0.32 (0.25–0.40) | 0.44 (0.33–0.58) | 0.32 (0.25–0.42) |
| British Columbia | 1.27 (0.92–1.76) | 1.18 (0.87–1.61) | 1.21 (0.87–1.68) | 1.10 (0.81–1.51) |
| Linguistic major | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 2.29 (1.79–2.91) | 2.26 (1.76–2.90) | 1.31 (0.99–1.74) | 1.21 (0.91–1.61) |
| Has a chronic condition | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 2.32 (2.05–2.62) | 2.31 (2.02–2.65) | 1.95 (1.71. 2.22) | 2.13 (1.84–2.47) |
| Intra-class correlation (rho) | 0.70 | 0.70 | ||
| AIC | 12 938.75 | 11 651.63 | ||
| Interaction terms | ||||
| White immigrant × time | 1.01 (0.96–1.07) | 0.99 (0.93–1.05) | ||
| Non-white immigrant × time | 0.97 (0.90–1.05)‡ | 1.09 (0.98–1.21)‡ | ||
AIC, Akaike Information Criteria.
The adjusted models also include living conditions and behavioural variables (smoking, alcohol use and physical exercise).
Test for trend: P < 0.001.
The interaction terms were not significant in both men and women.
The interaction between immigrant category and time of data collection was not significant, indicating that the association did not change with time across different immigrant categories.
Unmet health care need in the past 12 months
All the estimates for unifactorial and complete models of unmet health care need, are shown in Table 3. White male immigrants were less likely to report an unmet health care need in the past 12 months compared with Canadian born men (OR: 0.66, 95% CI: 0.47–0.95) once adjustment for all the other characteristics were made for; however, there was no significant difference between non-white immigrant and Canadian born men. The relationship was reversed in women, where only non-white immigrant women reported fewer unmet health care needs than Canadian women (OR: 0.32, 95% CI: 0.17–0.59), a feature not seen in white immigrant women. Overall, unmet health care needs at any assessment time were lower in older than younger subjects (both for men and women). However, the odds increased with increasing calendar time in both men and women. Thus, between-subject comparison suggested that older subjects are less likely to have unmet needs in a given year, whereas the ‘time’ effect suggested secular trends toward increasing odds of unmet needs among subjects of the same age. The interaction terms between immigrant categories and time of data collection were not significant, suggesting that the secular trends in unmet health care needs did not differ by immigrant category. Men and women in the lowest income category were more likely to have an unmet health care need than those in the highest income category; and there was a significant trend for higher odds of unmet health care needs with decreasing income in both men and women (test for trend p < 0.01). Individuals who did not have a regular doctor were more likely to report having an unmet health care need in the past 12 months.
Table 3.
Random effects models showing the unadjusted and adjusted estimates of odds ratios (OR) and their 95% confidence intervals (C.I.) for reporting an unmet healthcare need in 3081 males and 4187 females in Canada (1994–2006)
| Unadjusted estimates
|
Adjusted estimates
|
|||
|---|---|---|---|---|
| Males OR (95% C.I.) | Females OR (95% C.I.) | Males OR (95% C.I.) | Females OR (95% C.I.) | |
| Immigrant status | ||||
| Canadian born | Reference | Reference | Reference | Reference |
| White immigrants | 0.59 (0.42–0.82) | 0.78 (0.60–1.02) | 0.66 (0.47–0.95) | 0.93 (0.71–1.22) |
| Non-white immigrants | 0.74 (0.46–1.20) | 0.31 (0.17–0.55) | 0.78 (0.48–1.28) | 0.32 (0.17–0.59) |
| Age categories (years) | ||||
| 18–34 | Reference | Reference | Reference | Reference |
| 35–54 | 1.19 (0.99–1.43) | 1.22 (1.05–1.43) | 0.90 (0.73–1.11) | 0.91 (0.77–1.08) |
| 55–74 | 0.94 (0.75–1.18) | 0.97 (0.80–1.17) | 0.58 (0.44–0.76) | 0.58 (0.46–0.73) |
| ≥ 75 | 0.61 (0.41–0.91) | 0.84 (0.64–1.09) | 0.28 (0.17–0.45) | 0.38 (0.27–0.54) |
| Time | 1.08 (1.06–1.09) | 1.09 (1.08–1.10) | 1.09 (1.07–1.11) | 1.09 (1.08–1.11) |
| Education | ||||
| Primary | Reference | Reference | Reference | Reference |
| Secondary | 0.85 (0.63–1.15) | 0.99 (0.77–1.28) | 0.90 (0.66–1.24) | 0.95 (0.73–1.25) |
| Postsecondary | 1.34 (1.05–1.70) | 1.63 (1.33–2.01) | 1.26 (0.97–1.63) | 1.44 (1.15–1.81) |
| Graduate | 1.14 (0.91–1.43) | 1.59 (1.30–1.94) | 1.21 (0.94–1.56) | 1.39 (1.11–1.74) |
| Income category | ||||
| Highest | Reference | Reference | Reference | Reference |
| Upper middle | 0.91 (0.77–1.08) | 0.83 (0.71–0.96) | 1.11 (0.93–1.33) | 1.03 (0.88. 1.21) |
| Lower middle | 0.92 (0.75–1.12) | 0.79 (0.67–0.94) | 1.26 (1.00–1.57) | 1.12 (0.92–1.35) |
| Lowest | 1.13 (0.87–1.47) | 1.05 (0.87–1.28) | 1.58 (1.21–2.17)* | 1.59 (1.26–2.01)** |
| Marital status | ||||
| Single | Reference | Reference | Reference | Reference |
| Married | 0.89 (0.73–1.10) | 0.86 (0.72–1.04) | 0.96 (0.70–1.33) | 0.84 (0.63–1.13) |
| Separated | 1.32 (1.00–1.74) | 1.06 (0.86–1.32) | 1.13 (0.84–1.53) | 0.98 (0.78–1.24) |
| Province | ||||
| Others | Reference | Reference | Reference | Reference |
| Ontario | 0.91 (0.74–1.13) | 0.95 (0.79–1.14) | 1.01 (0.81–1.27) | 1.01 (0.84–1.22) |
| Quebec | 0.92 (0.72–1.16) | 1.15 (0.94–1.41) | 0.84 (0.62–1.12) | 1.02 (0.81–1.30) |
| British Columbia | 1.09 (0.82–1.45) | 1.33 (1.05–1.68) | 1.17 (0.86–1.57) | 1.40 (1.10–1.78) |
| Linguistic major | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 0.90 (0.69–1.19) | 0.78 (0.62–0.99) | 0.82 (0.58–1.16) | 0.81 (0.61–1.08) |
| Has a chronic condition | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 2.36 (2.02–2.75) | 2.81 (2.41–3.28) | 2.34 (2.00–2.79) | 2.69 (2.29–3.17) |
| Does not have a regular doctor | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 1.25 (1.05–1.49) | 1.74 (1.46–2.08) | 1.27 (1.05–1.54) | 1.83 (1.51–2.21) |
| Intra-class correlation (rho) | 0.55 | 0.57 | ||
| AIC | 8804.80 | 13 513.44 | ||
| Interaction terms | ||||
| White immigrant × time | 0.98 (0.92–1.05) | 0.99 (0.95–1.04) | ||
| Non-white immigrant × time | 1.02 (0.93–1.12)‡ | 1.10 (0.97–1.26)‡ | ||
AIC, Akaike Information Criteria.
The adjusted models also include living conditions and behavioural variables (smoking, alcohol use, and physical exercise). Test for trend:
P = 0.002,
P < 0.001.
The interaction terms were not significant in both men and women.
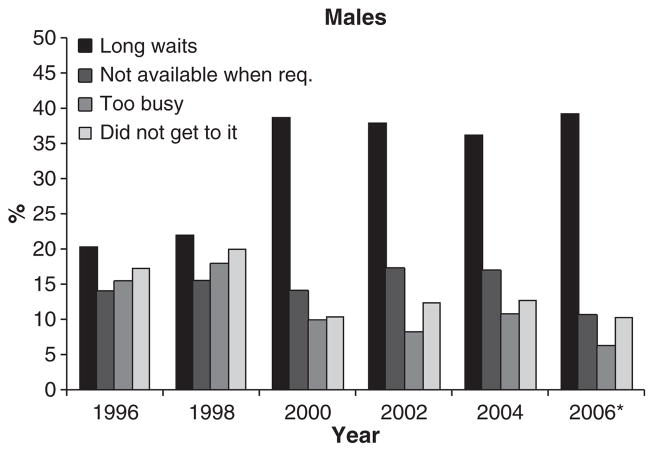
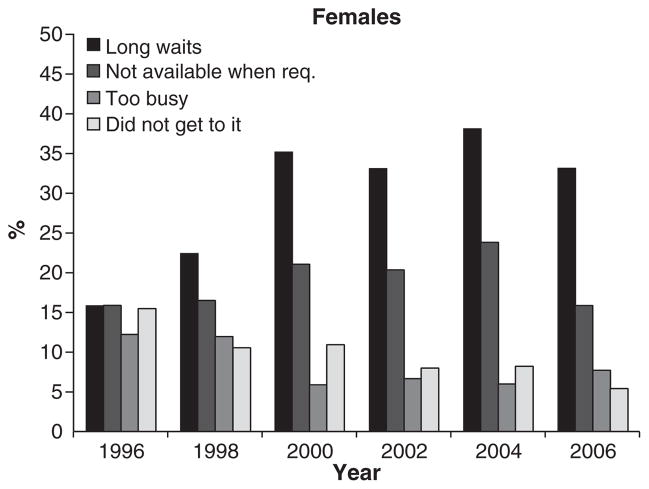
Among men, care for physical health (range 68% to 78%) and injuries (range 8% to 22%) were the most common types of unmet needs over these 12 years; in women it was care for physical health (range 66% to 79%) and mental health (range 9% to 15%). Detailed reasons for having unmet health care needs were collected from the 1996 wave onwards. Some of these reasons were: long waiting times and care not available when required. We have shown some important reasons for unmet health needs (1996–2006) in Figures 2 and 3.
Figure 2.
Common reasons for unmet healthcare needs among those reporting an unmet care need in 3081 men (1996–2006), Canada. *The number of women reporting unmet health needs who were ‘too busy’ was <15; hence exact number could not be reported as per Statistics Canada guidelines. The value for ‘too busy’ at this data point is <6%.
Figure 3.
Common reasons for unmet healthcare needs among those reporting an unmet care need in 4187 women (1996–2006), Canada.
In our sensitivity analyses, the difference in the estimates for each of the primary variable of interest between the models with dead individuals and our original models without dead individuals (both males and females) was less than one standard error; the odds ratios in the models with dead individuals changed in both directions i.e. increased and decreased for different outcomes (data not shown).
Immigrant only models
White and non-white immigrants reported similar access to a regular doctor (OR for non-white immigrants: 1.06, 95% CI: 0.54–2.09). However, increasing time since immigration was associated with better access to a regular doctor (OR per year after immigration: 1.02, 95% CI: 1.00 – 1.04). As with the general population, immigrants in Québec were less likely to report having a regular doctor (OR: 0.30, 95% CI: 0.11–0.80) than immigrants in other provinces. Female immigrants were more likely to have a regular doctor than males (OR: 2.25, 95% CI: 1.33–3.83). Immigrants living in Ontario had less frequent unmet health care needs compared to other provinces (OR: 0.59, 95% CI: 0.38–0.91). Similar to the findings observed in the general population, the odds of unmet health needs increased in immigrants with every additional year of data collection (OR: 1.09, 95% CI: 1.05–1.13). None of the interactions between time-since-immigration and sex, age, and immigrant categories were statistically significant.
Discussion
Immigrant men and women (white and non-white) reported better access to a regular doctor than did the Canadian born individuals in our population, over the 12-year period; with access increasing with duration of stay in Canada for all immigrants. White male immigrants and non-white female immigrants reported fewer unmet health care needs in the past 12 months.
Having a regular doctor may be considered a measure of ‘potential health care access’, meaning that those who have a regular doctor may be more likely to access care. 271–272 Our data showed some evidence of higher access to a regular doctor in immigrants; however, these effects were not statistically significant. Thus, immigrants in our sample reported similar, if not better, access to a regular doctor as the Canadian born population over these 12 years. But, in contrast, Lasser and co-workers 157 had reported slightly lower access to a regular doctor among immigrants in a cross-sectional national telephone survey in Canadians in 2002/03. In our data, access to a regular doctor improved in immigrants as the length of stay in Canada increased. Recent immigrants are less likely to have a regular doctor - a feature highlighted by immigrant women in Ontario. 145 Certain visible minority immigrants may prefer having health care professionals of their own ethnicity or who speak their language; 240 such preferences may potentially explain some delay in finding a regular doctor for these immigrants. However, after adjusting for time since immigration, we found that white and non-white immigrants had similar access to a regular doctor. Nevertheless, linking new immigrants to a regular doctor early on in their immigration process is potentially an important intervention point and may facilitate easy transition to a new health care system. It will also increase immigrants’ knowledge about health programmes in Canada and help in maintenance of their health and ultimately the health of the Canadian population in the long term.
Concerning unmet health needs, Wu and co-workers, 230 using the 2000/2001 cycle of Canadian Community Health Survey, found that fewer immigrants reported unmet health care needs compared to non-immigrants, as was also reported by Dunn & Dyck. 161 This finding was also replicated in our study, albeit only among white male immigrants and non-white female immigrants. Although previous qualitative studies and reports have shown that visible minority immigrant women report difficulties in accessing care, and are not satisfied about the care received, 142, 145, 273–274 we found that they reported fewer unmet health care needs. Shi & Stevens275 in the United States found that visible minority women (African-American, Asian, and Hispanic) were less likely to report a delayed or an unmet health care need. It is plausible that non-white immigrant women may actually have fewer unmet health care needs in Canada particularly if they migrate from countries with poor health care infrastructure or low gender equality ratios. However, it is also possible that these women have lower expectations of the health care systems, poor health literacy, or they tend to understate the lack of appropriate health care. Canadian born women and certain white immigrants who potentially are more aware of their health needs and vocal about the lack of it may therefore report higher unmet health needs. 275 Generally, long waiting times was one of the most common reasons for having an unmet health need - an issue that has been previously highlighted as one of the structural hindrances for accessing health. 149 However, personal reasons as ‘being too busy’ or ‘never got around it’ also featured in our population over these years; these were also reported as important barriers in a population study in Ontario. 276
Although immigrants in the province of Québec were less likely to have a regular doctor compared to immigrants in other provinces, this mirrored the reports of the general population of men and women in Québec in our study. This suggests that lack of access to a regular doctor may be a structural issue in Québec. 277 This would accord with reports that there is a doctor shortage in Québec; about 25% of Québec residents do not have a regular doctor as compared to the national average of 15%. 146 Despite a lack of access to a regular doctor, individuals in Québec did not report proportionally higher unmet health care needs than residents of other provinces. This may be due to the presence in Québec of alternative resources to access health care such as Centre de Santé et de Services Sociaux and Family Medicine Groups. 278 Nevertheless, in general we did find that after adjusting for all covariates, individuals who did not have a regular doctor were more likely to report an unmet health care need. This may be due to the ‘gate-keeping’ role of the primary physician.
As with other studies, this one also had its limitations. The sample size, especially for immigrants, was small. In addition, we had to aggregate heterogeneous groups of immigrants particularly non-white immigrants (e.g. Asian, South Asian, African, etc.) because of the small sample size. Thus, we recommend that future general population Canadian surveys should oversample visible minority immigrants: this will help us understand the differences within these groups. Further, we did not have information on the ‘class of immigration’ i.e., the type of immigrant category on which that had entered Canada (such as Economic class, Family class, Refugees to name some), so refugees, economic class, and family class were all treated as one group. Potentially, refugees are typically more disadvantaged than economic class immigrants when they enter Canada; however, they are typically provided with health care access, which may introduce a bias in our analyses.
This study has several strengths. First, our analyses take into account the within- and between-subject correlation over time, thus adding the longitudinal component to existing literature on health care access; this analyses period of 12-years is the maximum period for this national dataset. Second, we compared two measures of health care access (potential access and realised access) in the same group of individuals; thus providing a broader picture of health care access over the 12-year period. We find that immigrants (both white and non-white) have at least similar, if not better, access to a regular doctor as the Canadian born throughout the period of data collection. The access to a regular doctor in immigrants, improved with the duration of stay in Canada for both white and non-white immigrants throughout the 12 year period. An interesting finding was that, non-white female immigrants were the least likely to report an unmet health care need; however, it could not be ascertained whether it was due to excellent health coverage or lower expectations of the health care system 275 - an issue that needs to be explored further among visible minority women.
Contributor Information
Amélie Quesnel-Vallée, Department of Sociology, McGill University, Department of Epidemiology, Biostatistics, and Occupational Health, McGill University, Montreal, Canada.
Maninder S. Setia, Department of Epidemiology, Biostatistics, and Occupational Health, McGill University, Montreal, Canada
Michal Abrahamowicz, Department of Epidemiology, Biostatistics, and Occupational Health, McGill University, Montreal, Canada.
Pierre Tousignant, Department of Epidemiology, Biostatistics, and Occupational Health, McGill University, Montreal, Canada.
John Lynch, School of Health Sciences, University of South Australia, Adelaide, Australia, Department of Social Medicine, University of Bristol, Bristol, UK.
References
- Ahmad F, Shik A, Vanza R, Cheung AM, George U, Stewart DE. Voices of South Asian women: immigration and mental health. Women and Health. 2004;40:113–130. doi: 10.1300/j013v40n04_07. [DOI] [PubMed] [Google Scholar]
- Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19:716–723. [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Aroian KJ, Wu B, Tran TV. Health care and social service use among Chinese immigrant elders. Research in Nursing and Health. 2005;28:95–105. doi: 10.1002/nur.20069. [DOI] [PubMed] [Google Scholar]
- Asanin J, Wilson K. “I spent nine years looking for a doctor”: exploring access to health care among immigrants in Mississauga, Ontario, Canada. Social Science and Medicine. 2008;66:1271–1283. doi: 10.1016/j.socscimed.2007.11.043. [DOI] [PubMed] [Google Scholar]
- Barimah KB, Van Teijlingen ER. The use of traditional medicine by Ghanaians in Canada. BMC Complementary and Alternative Medicine. 2008;8:30. doi: 10.1186/1472-6882-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beiser M. The health of immigrants and refugees in Canada. Canadian Journal of Public Health Revue Canadienne de Sante Publique. 2005;96(Suppl 2):S30–S44. doi: 10.1007/BF03403701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beiser M, Hou F, Hyman I, Tousignant M. Poverty, family process, and the mental health of immigrant children in Canada. American Journal of Public Health. 2002;92:220–227. doi: 10.2105/ajph.92.2.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry J. Immigration acculturation and adaptation. Applied Psychology: An International Review. 1997;46:5–33. [Google Scholar]
- Bradshaw M, Tomany-Korman S, Flores G. Language barriers to prescriptions for patients with limited English proficiency: a survey of pharmacies. Pediatrics. 2007;120:e225–e235. doi: 10.1542/peds.2006-3151. [DOI] [PubMed] [Google Scholar]
- Carlin J, Galati J, Royston P. A new framework for managing and analyzing multiply imputed data in Stata. The Stata Journal. 2008;8:49–67. [Google Scholar]
- Chen J, Ng E, Wilkins R. The health of Canada’s immigrants in 1994–95. Health Reports. 1996;7:33–45. 37–50. [PubMed] [Google Scholar]
- Citizenship and Immigration Canada. Facts and Figures 2008 – Immigration Overview: Permanent and Temporary Residents. Ottawa, ON: 2009. [accessed on 14 August 2009]. [WWW document]. URL http://www.cic.gc.ca/english/resources/statistics/facts2008/permanent/01.asp. [Google Scholar]
- Deri C. Working Papers. Department of Economics, University of Ottawa; 2004. [accessed on 03 August 2009]. Understanding the ‘Health Immigrant Effect’ in Canada. [WWW document]. URL http://www.sciencessociales.uottawa.ca/eco/pdf/cahiers/0502E.pdf. [Google Scholar]
- Devoretz D, editor. Diminishing Returns: The Economics of Canada’s Recent Immigration Policy. C.D. Howe Institute; Toronto, ON: 1995. [Google Scholar]
- Duleep HO, Dowhan DJ. Research on immigrant earnings. Social Security Bulletin. 2008;68:31–50. [PubMed] [Google Scholar]
- Dunn JR, Dyck I. Social determinants of health in Canada’s immigrant population: results from the National Population Health Survey. Social Science and Medicine. 2000;51:1573–1593. doi: 10.1016/s0277-9536(00)00053-8. [DOI] [PubMed] [Google Scholar]
- Fédération Des Médecins Omnipraticiens Du Québec. [accessed on 26 May 2009];Énoncé de principes pour une politique nationale sur la médecine familiale. 2008 [WWW document]. URL http://www.fmoq.org/Documents/CommuniquesPresse/Politique%20nationale_FINALE.pdf.
- Glazier RH, Creatore MI, Cortinois AA, Agha MM, Moineddin R. Neighbourhood recent immigration and hospitalization in Toronto, Canada. Canadian Journal of Public Health Revue Canadienne de Sante Publique. 2004;95:I30–I34. doi: 10.1007/BF03403663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guend H, Tesseron A-L. Working papers, no 2009-04. Institut National de la Recherche Scientifique; Montreal: 2009. [accessed on 26 May 2009]. Unmet Needs for Primary Care in the Context of a Universal Healthcare System: The Case of Québec. [WWW document]. URL http://www.inrs-ucs.uQuebec.ca/pdf/inedit2009_04.pdf. [Google Scholar]
- Hyman I. [accessed on 20 February 2010];Racism as a determinant of immigrant health. 2009 [WWW document]. URL http://canada.metropolis.net/pdfs/racism_policy_brief_e.pdf.
- Lai D, Chappell N. Use of traditional Chinese medicine by older Chinese immigrants in Canada. Family Practice. 2007;24:56–64. doi: 10.1093/fampra/cml058. [DOI] [PubMed] [Google Scholar]
- Laroche M. Health status and health services utilization of Canada’s immigrant and non-immigrant populations. Canadian Public Policy. 2000;26:51–75. [PubMed] [Google Scholar]
- Lasser KE, Himmelstein DU, Woolhandler S. Access to care, health status, and health disparities in the United States and Canada: results of a cross-national population-based survey. American Journal of Public Health. 2006;96:1300–1307. doi: 10.2105/AJPH.2004.059402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llacer A, Zunzunegui MV, Del Amo J, Mazarrasa L, Bolumar F. The contribution of a gender perspective to the understanding of migrants’ health. Journal of Epidemiology and Community Health. 2007;61(Suppl 2):ii4–ii10. doi: 10.1136/jech.2007.061770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson CH, Park J. The nature and correlates of unmet health care needs in Ontario, Canada. Social Science and Medicine. 2006;62:2291–2300. doi: 10.1016/j.socscimed.2005.10.014. [DOI] [PubMed] [Google Scholar]
- Newbold B. Health status and health care of immigrants in Canada: a longitudinal analysis. Journal of Health Services Research & Policy. 2005;10:77–83. doi: 10.1258/1355819053559074. [DOI] [PubMed] [Google Scholar]
- Oxman-Martinez J, Hanley J, Lach L, Khanlou N, Weerasinghe S, Agnew V. Intersection of Canadian policy parameters affecting women with precarious immigration status: a baseline for understanding barriers to health. Journal of Immigrant Health. 2005;7:247–258. doi: 10.1007/s10903-005-5122-2. [DOI] [PubMed] [Google Scholar]
- Parchman M, Byrd T. Access to and use of ambulatory health care by a vulnerable Mexican American population on the U.S.-Mexico border. Journal of Health Care for the Poor and Underserved. 2001;12:404–414. doi: 10.1353/hpu.2010.0757. [DOI] [PubMed] [Google Scholar]
- Pineault R, Levesque J-F, Roberge D, Hamel M, Lamarche P, Haggerty J. Montreal: 2009. [accessed on 26 May 2009]. Accessibility and Continuity of Care: A Study of Primary Healthcare in Québec. [WWW document]. URL http://www.inspq.qc.ca/pdf/publications/911_ServicesPremLigneANGLAIS.pdf. [Google Scholar]
- Pitkin Derose K, Bahney BW, Lurie N, Escarce JJ. Review: immigrants and health care access, quality, and cost. Medical Care Research and Review. 2009;66:55–408. doi: 10.1177/1077558708330425. [DOI] [PubMed] [Google Scholar]
- Premji S, Messing K, Lippel K. Broken English, broken bones? Mechanisms linking language proficiency and occupational health in a Montreal garment factory. International Journal of Health Services. 2008;38:1–19. doi: 10.2190/HS.38.1.a. [DOI] [PubMed] [Google Scholar]
- Reitmanova S, Gustafson DL. “They can’t understand it”: maternity health and care needs of immigrant Muslim women in St John’s, Newfoundland. Maternal and Child Health Journal. 2008;12:101–111. doi: 10.1007/s10995-007-0213-4. [DOI] [PubMed] [Google Scholar]
- Riedel RL. Access to health care. In: Loue S, editor. Handbook of Immigrant Health. New York, NY, USA: Plenum Press; 1998. pp. 101–123. [Google Scholar]
- Royston P. Multiple imputation of missing values: update. The Stata Journal. 2005a;5:188–201. [Google Scholar]
- Royston P. Multiple imputation of missing values: update of ice. The Stata Journal. 2005b;5:527–536. [Google Scholar]
- Scheppers E, Van Dongen E, Dekker J, Geertzen J. Potential barriers to the use of health services among ethnic minorities: a review. Family Practice. 2006;23:325–348. doi: 10.1093/fampra/cmi113. [DOI] [PubMed] [Google Scholar]
- Shi L, Stevens GD. Vulnerability and unmet health care needs. The influence of multiple risk factors. Journal of General Internal Medicine. 2005;20:148–154. doi: 10.1111/j.1525-1497.2005.40136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snijders TAB, Bosker RJ. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. Sage Publication; London, UK: 1999. [Google Scholar]
- Statistics Canada. National Population Health Survey. Ottawa, ON: 2008. [accessed on 03 August 2009]. [WWW document]. URL http://www.statcan.ca/cgibin/imdb/p2SV.pl?Function=getSurvey&SurvId=3225&SurvVer=0&InstaId=15280&InstaVer=5&SDDS=3225&lang=fr&db=IMDB&dbl=E&adm=8&dis=2. [Google Scholar]
- The Lancet. Institutionalised racism in health care. Lancet. 1999;353:765. [PubMed] [Google Scholar]
- Van Buuren S, Oudshoorn K. Flexible Multivariate Imputation by MICE. Leiden, The Netherlands: 1999. [accessed on 15 February 2009]. (TNO Report PG/VGZ/99.054) [WWW document]. URL http://www.multiple-imputation.com/ [Google Scholar]
- Van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Statistics in Medicine. 1999;18:681–694. doi: 10.1002/(sici)1097-0258(19990330)18:6<681::aid-sim71>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Vissandjée B, Desmeules M, Cao Z, Abdool S, Kazanjian A. Integrating ethnicity and migration as determinants of Canadian women’s health. BMC Womens Health. 2004;4(Suppl 1):S32. doi: 10.1186/1472-6874-4-S1-S32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vittinghoff E, Glidden DV, Shiboski SC, Mcculloch CE. Regression Methods in Biostatistics. Springer Science+Business Media, Inc; New York, NY, USA: 2004. [Google Scholar]
- Wang L. Immigration, ethnicity, and accessibility to culturally diverse family physicians. Health Place. 2007;13:656–671. doi: 10.1016/j.healthplace.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Wen SW, Goel V, Williams JI. Utilization of health care services by immigrants and other ethnic/cultural groups in Ontario. Ethnicity & Health. 1996;1:99–109. doi: 10.1080/13557858.1996.9961775. [DOI] [PubMed] [Google Scholar]
- Wilson K, Rosenberg MW. Accessibility and the Canadian health care system: squaring perceptions and realities. Health Policy. 2004;67:137–148. doi: 10.1016/s0168-8510(03)00101-5. [DOI] [PubMed] [Google Scholar]
- Wu Z, Penning MJ, Schimmele CM. Immigrant status and unmet health care needs. Canadian Journal of Public Health Revue Canadienne de Sante Publique. 2005;96:369–373. doi: 10.1007/BF03404035. [DOI] [PMC free article] [PubMed] [Google Scholar]