Abstract
Objective
To analyze the fatigue resistance, debonding force, and failure type of fiber-reinforced composite, polyethylene ribbon-reinforced, and braided stainless steel wire lingual retainers in vitro.
Methods
Roots of human mandibular central incisors were covered with silicone, mimicking the periodontal ligament, and embedded in polymethylmethacrylate. The specimens (N = 50), with two teeth each, were randomly divided into five groups (n = 10/group) according to the retainer materials: (1) Interlig (E-glass), (2) everStick Ortho (E-glass), (3) DentaPreg Splint (S2-glass), (4) Ribbond (polyethylene), and (5) Quad Cat wire (stainless steel). After the recommended adhesive procedures, the retainers were bonded to the teeth by using flowable composite resin (Tetric Flow). The teeth were subjected to 10,00,000 cyclic loads (8 Hz, 3 - 100 N, 45° angle, under 37 ± 3℃ water) at their incisoproximal contact, and debonding forces were measured with a universal testing machine (1 mm/min crosshead speed). Failure sites were examined under a stereomicroscope (×40 magnification). Data were analyzed by one-way analysis of variance.
Results
All the specimens survived the cyclic loading. Their mean debonding forces were not significantly different (p > 0.05). The DentaPreg Splint group (80%) showed the highest incidence of complete adhesive debonding, followed by the Interlig group (60%). The everStick Ortho group (80%) presented predominantly partial adhesive debonding. The Quad Cat wire group (50%) presented overlying composite detachment.
Conclusions
Cyclic loading did not cause debonding. The retainers presented similar debonding forces but different failure types. Braided stainless steel wire retainers presented the most repairable failure type.
Keywords: Lingual, Bonding, Relapse, Retention
INTRODUCTION
Lingual retainers are generally used for long-term retention.1 They are preferred particularly when the posttreatment intercanine width should be maintained and periodontal tissue support is lacking.1,2 However, breakage of the retainer material and debonding of the resin pad that attaches the retainer onto the tooth surface are commonly experienced in clinical practice.2-5 The main factors determining the longevity and success of lingual retainers are the type of retainer material, type of composite resin used for bonding, number of units included for bonding, and location of the retainer (i.e., maxillary or mandibular arch).2-5
The most frequently used retainer material is stainless steel wire, with varying stiffness and integral properties.2,5 Initially, lingual retainers were fabricated from relatively thick round wires (0.030 - 0.032 inch) bonded only to the ends of the retention area.3,4 With this type of retainer, the intercanine width could be well preserved and the retention area was easily accessible to oral hygiene instruments, but rotation of the interlying teeth was evident because they were not bonded to the retainer. Thinner multistranded wire (0.0195 - 0.0215 inch) bonded to each interlying tooth was introduced to overcome this problem.3,4 However, this retainer type increased the susceptibility to plaque accumulation and presented higher failure rates due to wire breakage and resin pad detachment.2,5 Subsequently, fiber-reinforced composite (FRC) was introduced to replace stainless steel wire, thus allowing chemical adhesion of the retainer to the bonding agent.6 FRC was expected to reinforce the resistance of the bonding agent by transferring the loads acting on the retainer complex to the glass fibers. Furthermore, the bonding interface of two materials with different physical properties (i.e., wire and composite resin) would be eliminated.6,7 Nevertheless, retainer failures still occurred and clinical survival studies did not reveal significant results. Therefore, multistranded stainless steel wire is still the most frequently used material for lingual retainers.1,2,5
The causes of lingual retainer failures are still not clear. The most frequent problems of metal retainers are failure of the wire-composite interface, breakage of the wire, and detachment of the resin pads at the composite-enamel interface.1-4,7 Wire-composite interface failure is attributable to two main factors. First, the composite covering the retainer, usually a small resin pad, becomes thinner and weaker because of abrasion caused by brushing and food consumption. This, in turn, results in detachment of the retainer from the resin pad, which stays stable on the tooth surface.1-4,7 Second, propagation of internal cracks due to constant movement of the retainer between the overlying and the underlying resin pads during physiological tooth movement is linked to wire-composite interface failure.1,2,7 This is also a possible reason for breakage of the retainer due to the stress accumulation at bending points.3,4 On the other hand, composite-enamel interface failure is attributable to adhesion failure of the resin pad. Debonding of the resin pad from the tooth surface is mostly associated with deficient bonding procedures, such as inadequate moisture control or mishandling of the resin material.1,3,7 Furthermore, increased tooth mobility due to a widened periodontal ligament space or lack of bone support could cause deterioration of the adhesion at the composite-enamel interface.1
The in vivo failure and survival rates of lingual retainers, in vitro testing of different retainer material complexes, and interpretation of the results are highly controversial.5,8-16 In a recent clinical report of metal and FRC retainers, the conventional multistranded wire retainers were suggested to remain the gold standard for orthodontic retention and the use of FRC retainers was discouraged because of their high failure rate (12% vs 51%, respectively).14 Similarly, multistranded wire retainers were reported to be significantly superior to polyethylene ribbon-reinforced retainers.13 On the other hand, a recent 6-year clinical follow-up study showed no significant differences between FRC and multistranded wire retainers; the results indicated that FRC retainers could be a viable alternative to multistranded wire retainers.15 Two recent clinical studies showed a 37.9% failure rate in a 6-month period with multistranded wire retainers11 and a 94.8% survival rate in a 4.5-year period with FRC retainers.16 From the adhesion perspective, the debonding force of FRC retainers was not found to be dependent on the type of bonding agent used.17 Contrarily, superior adhesion has been reported with the use of a specific lingual retainer adhesive instead of a flowable composite resin.18 The disagreement among such studies is highlighted in a review by Littlewood et al.,5 implying that further research for retainer comparisons is necessary.17
The objective of this in vitro study was to analyze the fatigue resistance, debonding force, and failure type of FRC, polyethylene ribbon-reinforced, and braided stainless steel wire lingual retainers. The null hypotheses were that the fatigue resistance of the FRC and polyethylene ribbon-reinforced retainers would not be greater and their debonding forces would not be higher than those of the braided stainless steel wire retainer.
MATERIALS AND METHODS
Specimen preparation
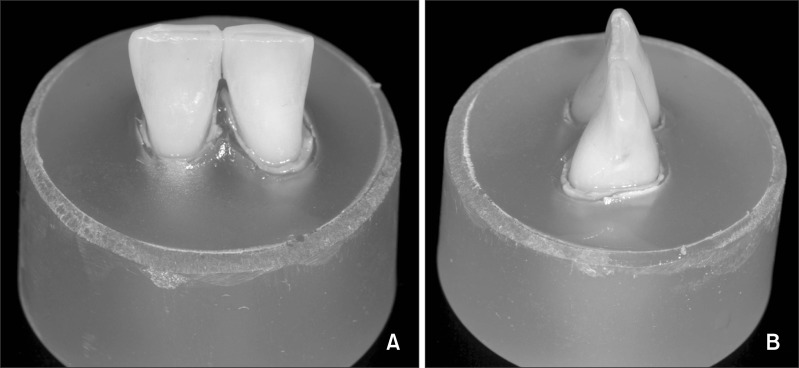
Hundred caries-free human mandibular central incisors stored in 0.1% thymol solution at 4℃ up to 6 months were selected under blue-light transillumination to ensure that the enamel was free of cracks. The roots of pairs (i.e., right and left) of the selected teeth were dipped in hot liquid wax (Modern Materials utility wax; Heraeus Kulzer GmbH, Hanau, Germany) and embedded in silicone impression material (Adisil® blau 9:1; Böhme & Schöps GmbH, Goslar, Germany) in a plastic mold with axial contact. After the impression material had set, the same process was repeated with polymethylmethacrylate (Vertex 2 SMS, 24 × 24 × 33 mm; Vertex-Dental B.V., Zeist, The Netherlands). The wax layer was removed with hot water (100℃) and the created space was filled with light-body silicone (Pro Fill; Heraeus Kulzer GmbH) to mimic the periodontal ligament, supposedly allowing some physiological movement during cyclic loading.19,20 The roots of the teeth were then inserted into the silicone (Figure 1). Fifty specimens, each containing a pair of incisors, were used for the experiments.
Figure 1.
Representative photographs of human mandibular central incisor pairs embedded in polymethylmethacrylate up to the cementoenamel junction to receive bonded lingual retainers: A, lingual and B, proximal views.
Before the bonding procedures, the lingual surfaces of the embedded teeth were polished with fluoride-free pumice (Zircate Prophy Paste; Dentsply Caulk, Milford, DE, USA) by using a prophylaxis brush (Hawe Prophy Cup and Brush, latch-type; Kerrhawe Sa, Bioggio Svizzera, Switzerland) for 20 seconds, rinsed with water, and air-dried. The mesiodistal dimensions of the two teeth in each specimen were measured and the midpoint 3 mm below the incisal edges was marked as the area for bonding by using a permanent marker.
Retainer materials
The specimens were randomly divided into five groups (n = 10 per group) according to the main retainer materials: (1) E-glass (Interlig; Angelus Ltd., Londrina, Brazil), (2) E-glass (everStick Ortho; Stick Tech Ltd., Turku, Finland), (3) S2-glass (DentaPreg Splint; ADM a.s., Brno, Czech Republic), (4) polyethylene (Ribbond; Ribbond Inc., Seattle, WA, USA), and (5) stainless steel (Quad Cat wire; GAC International Inc., Islandia, NY, USA).
Retainer placement
Braided stainless steel wires (0.022 × 0.016 inch) were adapted to the lingual surfaces of the teeth in each specimen and ultrasonically cleaned in ethyl alcohol (Vitasonic; Vita Zanhfabrik H. Rauter GmbH & Co. KG, Bad Säckingen, Germany) for 20 seconds. The marked bonding area was then etched with 38% H3PO4 (Top Dent; DAB Dental, Tillverkare, Sweden) for 20 seconds, rinsed with water for 20 seconds, and air-dried. An adhesive resin (Heliobond; Ivoclar Vivadent, Schaan, Liechtenstein) was applied by using a microbrush (Apply-Tip; Hager & Werken, Oisterwijk, The Netherlands), gently air-blown, and photo-polymerized for 20 seconds on each tooth surface with an LED polymerization lamp (Ortholux LED curing light, light output = 400 mW/cm2; 3M Unitek, Landsberg am Lech, Germany). A thin layer of flowable composite resin (Tetric Flow, Cavifill 210, shade A3; Ivoclar Vivadent) was applied and the retainer was placed in the composite resin. After initial polymerization, the composite resin was applied to cover the retainer surface and photo-polymerized for 40 seconds on each tooth surface. The irradiation distance between the light-source tip and the resin surface was maintained at 2 mm.
Retainers fabricated from standard lengths of the FRCs and polyethylene ribbon were bonded in exactly the same manner as described for the stainless steel wire retainers.
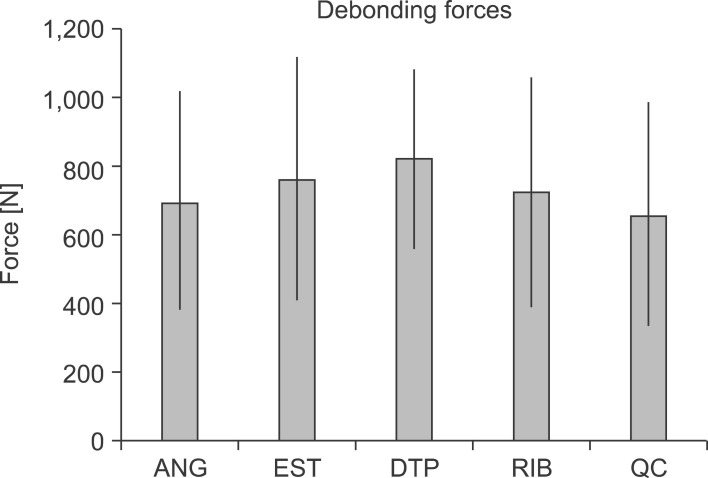
The brand names, abbreviations, compositions, manufacturer details, and batch numbers of the tested materials are listed in Table 1.
Table 1.
Details of the retainer materials tested in this study.
GMA, Glycidyl methacrylate; PMMA, polymethyl methacrylate.
Cyclic loading and debonding force testing
The specimens were subjected to 10,00,000 cyclic loading. The load was applied at the incisoproximal contact of the tooth pair from the lingual side to the labial side by using a jig (Figure 2). The force vector formed an approximately 45° angle with the long axis of the tooth pair. The load frequency was 8 Hz and alternated from 3 N to 100 N. The specimens were kept in 37 ± 3℃ water during the procedure.21
Figure 2.
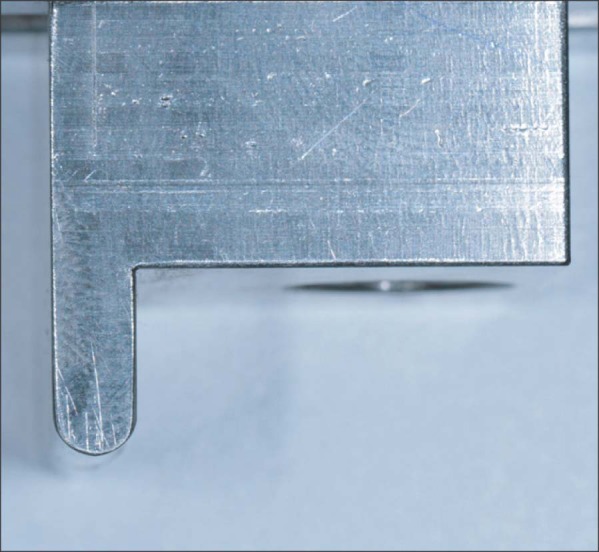
The loading jig used for measuring the debonding force of the bonded lingual retainers.
Following fatigue formation, the specimens were tested for the debonding force by using a universal testing machine (Z2.5MA, 18-1-3/7; Zwick GmbH & Co. KG, Ulm, Germany) at a crosshead speed of 1 mm/min. The debonding force was applied with the same settings and jig as in the cyclic loading experiment until debonding occurred. Only the maximum force causing debonding of the retainers was recorded.
Failure analysis
Failure sites were examined under a stereomicroscope at varying magnifications (up to ×40). After the initial evaluation of the specimens, four types of failure were categorized, as follows: type 1, complete adhesive debonding of the retainer from the tooth surface; type 2, partial adhesive detachment of the retainer from one of the teeth; type 3, retainer did not debond from the tooth surface but fractured; and type 4, retainer did not debond from the tooth surface but the overlying composite detached.
Statistical analysis
Statistical analysis was performed by using Statistix 8.0 for Windows (Analytical Software Inc., Tallahassee, FL, USA). Means were analyzed by one-way analysis of variance (ANOVA). p-values less than 0.05 were considered significant.
RESULTS
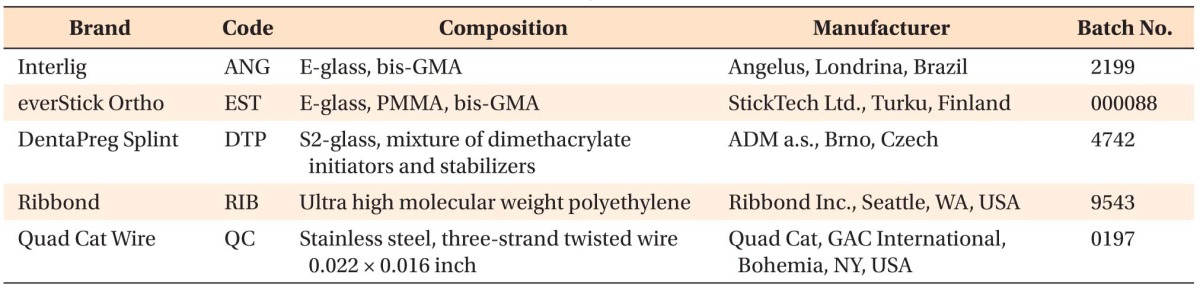
All the specimens survived the cyclic loading. The mean debonding forces were 706 ± 312 N, 772 ± 348 N, 830 ± 258 N, 731 ± 329 N, and 670 ± 323 N in the Interlig, everStick Ortho, DentaPreg Splint, Ribbond, and Quad Cat wire groups, respectively, without significant differences (p > 0.05) (Figure 3).
Figure 3.
Mean and standard deviation of the debonding force of the bonded lingual retainers. See Table 1 for a detailed description of the groups.
According to the failure analysis, the highest incidence of type 1 failure occurred in the DentaPreg Splint group (eight specimens) followed by the Interlig group (six specimens). The everStick Ortho group presented predominantly type 2 failure (eight specimens) and the Quad Cat wire group showed type 4 failure in five specimens (Table 2).
Table 2.
Frequencies (%) of failure of the bonded lingual retainers subjected to cyclic loading
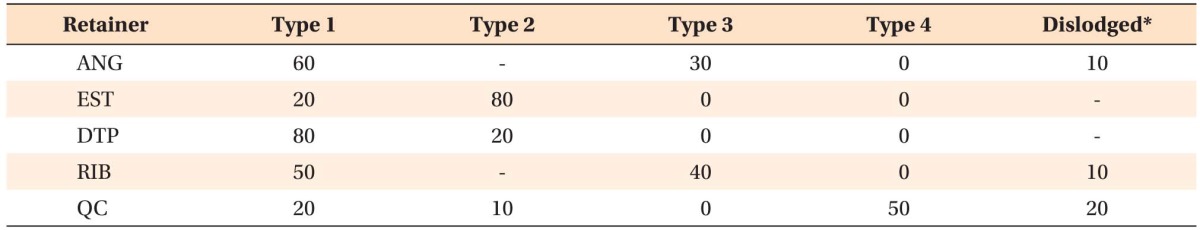
Type 1, Complete adhesive debonding of the retainer from the tooth surface; type 2, partial adhesive detachment of the retainer from one of the teeth; type 3, retainer did not debond from the tooth surface but fractured; type 4, retainer did not debond from the tooth surface but the overlying composite detached. See Table 1 for a detailed description of the groups.
*Each specimen consisted of a pair of teeth.
DISCUSSION
In this study, none of the retainers failed during cyclic loading and all the tested materials showed similar debonding forces. However, their failure types varied. The null hypotheses that the fatigue resistance of the FRC and polyethylene ribbon-reinforced retainers would not be superior to that of the stainless steel wire retainer and they would not have higher debonding forces were accepted.
Under clinical conditions, lingual retainers are subjected to cyclic stresses because of mastication, occlusion, and intraoral habits.22-24 This repeated subcritical loading induces fatigue and may cause partial or total failure of one or more components of the retainer complex. These forces are usually below the maximum debonding forces in in vitro studies, but they may have the destructive effect of high-magnitude sudden impacts that seldom occur in real life.22-24 Therefore, fatigue tests are expected to clarify the clinical durability better than static tests.22-24 However, the degree of fatigue necessary to induce failure in initially intact specimens cannot be easily predicted.
The two main factors determining the effect of fatigue on composite materials are (1) the factors associated with the cyclic load (i.e., quantity, magnitude, and direction of load application) and (2) the factors associated with the test material (e.g., type of reinforcement, filler-matrix ratio, and interfacial strength). The cyclic load quantity in previous fatigue studies ranged from 20,000 to 2,000,000, showing great variation.7,24 Supposedly, 2,000,000 cycles correspond to approximately 4 years of normal occlusal and masticatory activities.24 Although merely an estimation, 1,000,000 cycles, as applied in this study, would correspond to approximately 2 years of clinical service. This quantity was used on the basis of the outcomes of clinical studies in which retainer failures due to debonding were reported within this period.2-4,9 Another factor affecting fatigue formation is the magnitude of the load acting on the test material. In previous studies, constant or varying forces between 40 and 600 N were applied.21-25 In the present study, a load ranging from 3 N to 100 N was applied at a frequency of 8 Hz. In reality, the applied force is considered zero in the absence of occlusal contact or function; however, to maintain the contact of the load cell on the specimen, 3 N was applied as the minimum load. Nevertheless, a standard method for fatigue tests has not been established, because chewing cycles vary in every individual as well as experimental settings. Therefore, these tests still present limitations and their outcomes should be interpreted with caution.
The adverse effect of fatigue on materials with similar physical properties is more predictable, because cyclic loading will have an equal impact on them.21-25 Therefore, elimination of wires in the retainer complex by using FRC might improve stability and reduce fatigue formation, because adhesion would rely only on bonding of the flowable composite resin or resin matrix of the FRC to the etched enamel. However, in the present study, none of the retainers failed during fatigue formation and no significant differences were observed in terms of the debonding force. These results are attributable to the specimen properties, where only two units were included, forming a very short retainer complex compared with that used clinically. However, the cyclic load could not be applied on 4- or 6-unit retainer specimens because of the experimental settings and design.
From the chemical perspective, hydrolysis, which can break the covalent bonds in the resin,25 and plasticization, which can diminish the mechanical resistance of the polymer,26 were possibly not effective enough to cause failure during fatigue formation. This lack of an effect might be attributable to the relatively stable water temperature (37 ± 3℃) in which the specimens were kept during fatigue formation; clinically, higher temperatures are encountered. Future studies should incorporate temperature alterations in the fatigue formation procedures for testing lingual retainers.
The lack of debonding during cyclic loading and the insignificant difference in the debonding forces of the retainers may initially suggest that all the tested materials behaved similarly. Interestingly, even the stainless steel wire retainer, with its smaller bonding area than that of the FRC retainers, demonstrated a similar debonding force. The extent of fatigue created in this design cannot be determined, and the failure types deserve more attention than the performance of the tested materials. The failure types should be evaluated with regard to not only the adhesion quality but also the clinical reversibility, with the least damage to enamel during removal or repair of the failed retainer. The FRC retainers themselves showed various failure types. Those composed of Interlig (60%) and DentaPreg Splint (80%) mainly presented complete adhesive debonding. Given that the same bonding agent was used in all the groups, this failure type indicates that the interfacial strength between the tested material and the bonding resin exceeded the adhesion between the bonding resin and enamel. In contrast, the everStick Ortho retainers (80%) presented partial adhesive debonding from one of the teeth. The Ribbond retainers presented adhesive failure and material breakage in 50% and 40% of the specimens, respectively. Resin adhesion to polyethylene FRCs was less favorable in previous in vitro studies mainly because of the difficulty in plasma coating, silanization, and impregnation of the polyethylene fibers.7 Such combinations of failure types may not cause direct enamel damage but will necessitate removal of the attached retainers by using rotary instruments and renewal of the bonding procedure. The potential detrimental effects of debonding a retainer from enamel during either bracket debonding or retainer removal present an iatrogenic problem. Therefore, all these material options cannot be considered durable and favorable.
The Quad Cat wire group presented type 4 failure in 50% of the specimens. This result implies that either the adhesion at the composite-enamel interface was superior to the adhesion at the composite-wire interface or the cyclic load weakened the latter. This type of failure could surely allow repair of the detached composite part without removal of the remnants. Therefore, it could be considered a reversible situation and perhaps more favorable than the other failure types. Reinforcement of the composite in the other materials might have been accomplished, but the lack of flexibility eventually led to different failure types in the Quad Cat wire group.
CONCLUSION
1. Fatigue created by cycling loading did not cause failure of the lingual retainer materials tested.
2. All the tested materials performed similarly in terms of the debonding force following fatigue formation.
3. The failure types varied among the materials. The braided stainless steel wire retainer presented the most repairable failure type.
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Renkema AM, Renkema A, Bronkhorst E, Katsaros C. Long-term effectiveness of canine-to-canine bonded flexible spiral wire lingual retainers. Am J Orthod Dentofacial Orthop. 2011;139:614–621. doi: 10.1016/j.ajodo.2009.06.041. [DOI] [PubMed] [Google Scholar]
- 2.Bearn DR. Bonded orthodontic retainers: a review. Am J Orthod Dentofacial Orthop. 1995;108:207–213. doi: 10.1016/s0889-5406(95)70085-4. [DOI] [PubMed] [Google Scholar]
- 3.Dahl EH, Zachrisson BU. Long-term experience with direct-bonded lingual retainers. J Clin Orthod. 1991;25:619–630. [PubMed] [Google Scholar]
- 4.Artun J, Spadafora AT, Shapiro PA. A 3-year follow-up study of various types of orthodontic canine-to-canine retainers. Eur J Orthod. 1997;19:501–509. doi: 10.1093/ejo/19.5.501. [DOI] [PubMed] [Google Scholar]
- 5.Littlewood SJ, Millett DT, Doubleday B, Bearn DR, Worthington HV. Orthodontic retention: a systematic review. J Orthod. 2006;33:205–212. doi: 10.1179/146531205225021624. [DOI] [PubMed] [Google Scholar]
- 6.Burstone CJ, Kuhlberg AJ. Fiber-reinforced composites in orthodontics. J Clin Orthod. 2000;34:271–279. [Google Scholar]
- 7.Foek DL, Ozcan M, Krebs E, Sandham A. Adhesive properties of bonded orthodontic retainers to enamel: stainless steel wire vs fiber-reinforced composites. J Adhes Dent. 2009;11:381–390. [PubMed] [Google Scholar]
- 8.Lumsden KW, Saidler G, McColl JH. Breakage incidence with direct-bonded lingual retainers. Br J Orthod. 1999;26:191–194. doi: 10.1093/ortho/26.3.191. [DOI] [PubMed] [Google Scholar]
- 9.Lie Sam Foek DJ, Ozcan M, Verkerke GJ, Sandham A, Dijkstra PU. Survival of flexible, braided, bonded stainless steel lingual retainers: a historic cohort study. Eur J Orthod. 2008;30:199–204. doi: 10.1093/ejo/cjm117. [DOI] [PubMed] [Google Scholar]
- 10.Lee KD, Mills CM. Bond failure rates for V-loop vs straight wire lingual retainers. Am J Orthod Dentofacial Orthop. 2009;135:502–506. doi: 10.1016/j.ajodo.2007.04.037. [DOI] [PubMed] [Google Scholar]
- 11.Taner T, Aksu M. A prospective clinical evaluation of mandibular lingual retainer survival. Eur J Orthod. 2012;34:470–474. doi: 10.1093/ejo/cjr038. [DOI] [PubMed] [Google Scholar]
- 12.Cooke ME, Sherriff M. Debonding force and deformation of two multi-stranded lingual retainer wires bonded to incisor enamel: an in vitro study. Eur J Orthod. 2010;32:741–746. doi: 10.1093/ejo/cjq017. [DOI] [PubMed] [Google Scholar]
- 13.Rose E, Frucht S, Jonas IE. Clinical comparison of a multistranded wire and a direct-bonded polyethylene ribbon-reinforced resin composite used for lingual retention. Quintessence Int. 2002;33:579–583. [PubMed] [Google Scholar]
- 14.Tacken MP, Cosyn J, De Wilde P, Aerts J, Govaerts E, Vannet BV. Glass fibre reinforced versus multistranded bonded orthodontic retainers: a 2 year prospective multi-centre study. Eur J Orthod. 2010;32:117–123. doi: 10.1093/ejo/cjp100. [DOI] [PubMed] [Google Scholar]
- 15.Bolla E, Cozzani M, Doldo T, Fontana M. Failure evaluation after a 6-year retention period: a comparison between glass fiber-reinforced (GFR) and multistranded bonded retainers. Int Orthod. 2012;10:16–28. doi: 10.1016/j.ortho.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Kumbuloglu O, Saracoglu A, Ozcan M. Pilot study of unidirectional E-glass fibre-reinforced composite resin splints: up to 4.5-year clinical follow-up. J Dent. 2011;39:871–877. doi: 10.1016/j.jdent.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 17.Meiers JC, Kazemi RB, Donadio M. The influence of fiber reinforcement of composites on shear bond strengths to enamel. J Prosthet Dent. 2003;89:388–393. doi: 10.1067/mpr.2003.87. [DOI] [PubMed] [Google Scholar]
- 18.Scribante A, Cacciafesta V, Sfondrini MF. Effect of various adhesive systems on the shear bond strength of fiber-reinforced composite. Am J Orthod Dentofacial Orthop. 2006;130:224–227. doi: 10.1016/j.ajodo.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 19.Fokkinga WA, Le Bell AM, Kreulen CM, Lassila LV, Vallittu PK, Creugers NH. Ex vivo fracture resistance of direct resin composite complete crowns with and without posts on maxillary premolars. Int Endod J. 2005;38:230–237. doi: 10.1111/j.1365-2591.2005.00941.x. [DOI] [PubMed] [Google Scholar]
- 20.Ozcan M, Valandro LF. Fracture strength of endodontically-treated teeth restored with post and cores and composite cores only. Oper Dent. 2009;34:429–436. doi: 10.2341/08-110. [DOI] [PubMed] [Google Scholar]
- 21.Baldissara P, Ozcan M, Melilli D, Valandro LF. Effect of cyclic loading on fracture strength and microleakage of a quartz fiber dowel with different adhesive, cement and resin core material combinations. Minerva Stomatol. 2010;59:407–414. [PubMed] [Google Scholar]
- 22.McCabe JF, Carrick TE, Chadwick RG, Walls AW. Alternative approaches to evaluating the fatigue characteristics of materials. Dent Mater. 1990;6:24–28. doi: 10.1016/0109-5641(90)90040-l. [DOI] [PubMed] [Google Scholar]
- 23.Ruse ND, Shew R, Feduik D. In vitro fatigue testing of a dental bonding system on enamel. J Biomed Mater Res. 1995;29:411–415. doi: 10.1002/jbm.820290316. [DOI] [PubMed] [Google Scholar]
- 24.Grandini S, Chieffi N, Cagidiaco MC, Goracci C, Ferrari M. Fatigue resistance and structural integrity of different types of fiber posts. Dent Mater J. 2008;27:687–694. doi: 10.4012/dmj.27.687. [DOI] [PubMed] [Google Scholar]
- 25.Sahafi A, Peutzfeldt A, Ravnholt G, Asmussen E, Gotfredsen K. Resistance to cyclic loading of teeth restored with posts. Clin Oral Investig. 2005;9:84–90. doi: 10.1007/s00784-004-0299-7. [DOI] [PubMed] [Google Scholar]
- 26.De Munck J, Van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Braem M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res. 2005;84:118–132. doi: 10.1177/154405910508400204. [DOI] [PubMed] [Google Scholar]