Abstract
Purpose
In modern days, grand multiparity is confined to communities where contraception is not practiced because of social and religious beliefs. For this reason, it is quite prevalent in all GCC countries. Few studies have compared the outcomes between the three groups: low parity (2–4), grand multiparity (5–9), and great grand multiparity (10 and more) . This study intended to analyze the trends in the occurrence of various perinatal complications across these three groups.
Methods
This historical cohort study was conducted in Mafraq Hospital, Abu Dhabi between January 1, 2009 and December 31, 2011. There were 1,658 multipara, 1,198 grand multipara, and 160 great grand multipara.
Results
Different complications revealed different trends with increasing parity. Many antenatal and intrapartum complications like diabetes (overt and gestational), anemia, preterm delivery, malpresentation at term, postpartum hemorrhage, and macrosomia showed a linear increase with increasing parity, while some, like the need for labor augmentation and soft tissue injuries showed a declining trend with increasing parity. Interestingly, some complications like placenta praevia, need for induction of labor, cesarean delivery, and post-term delivery followed an inverted V curve, showing an increase in their occurrence up to parity nine but a decline thereafter with further increasing parity of ten or beyond.
Conclusion
Women in different parity groups were at risk of different complications. There are some complications which decrease with increasing parity, and perinatal mortality remains very low suggesting that in modern settings, with favorable socioeconomic conditions and access to high-quality healthcare, a satisfactory perinatal outcome can be expected with low morbidity and mortality.
Keywords: Grand multiparity, Antenatal, Perinatal complications
Introduction
Grand multiparity has almost disappeared in the western countries because of widespread acceptance of family planning methods. Thus, in modern times, it is confined only to communities where contraception is not practiced because of social taboos, cultural practices and religious beliefs. For this reason, it is quite prevalent in all GCC countries.
In United Arab Emirates, having large families is a norm rather than exception. The incidence of grand multiparity ranges between 31.7 and 36 % [1].
The issue of high parity as a risk factor in maternal and neonatal morbidity has been quite controversial for many decades. As the condition is not very common in developed countries, there is scant information in standard text books about the management of these women. The results of literature search are not consistent. This may partly be because the definition of grand multiparity used in different studies is different.
Most of the studies in the literature have compared the outcome between women of low parity (parity 2–4) and grand multiparty (parity 5–9), but only few studies have compared the outcome between the three groups as defined by International Federation of Gynecology and Obstetrics: lower parity (parity 2–4), grand multiparity (parity 5–9) and great grand multiparity (parity 10 and above).
Objective
The main purpose of this study was to examine the trends and patterns in the occurrence of various antenatal and perinatal complications with increasing parity across the three parity groups as described by International Federation of Gynecology and Obstetrics.
Study Design
A historical cohort study.
Setting
The study was conducted in Al Mafraq Hospital which is a tertiary care hospital in Abu Dhabi, United Arab Emirates (UAE), with an annual delivery rate of about 3000.
Duration of the Study
From January 1, 2009 to December 31, 2011.
Materials and Methods
A historical cohort comprising all those Emirati women (n = 3,016) who delivered between January 1, 2009 and December 31, 2011 in the hospital investigated was included in the study with the exception of following:
Primiparous women (n = 1,080);
Women under the age of 18 years (n = 124);
Women more than 35 years of age (n = 695); and
Women with multiple pregnancies (n = 98)
All the Emirati women who did not satisfy the exclusion criteria were included in the cohort to limit selection bias.
Information on the frequency and outcome of maternal and neonatal factors and complications was tracked down from the cohort of women delivering in the study setting as identified above and validated from various data sources like Antenatal Register, Maternity Register, and Computerized Hospital Information System.
Exposure misclassification which can be a limitation of cohort studies was controlled by excluding the subjects with incomplete data.
Maternal outcome variables analyzed were hypertensive disorders of pregnancy, gestational diabetes mellitus, placental abruption, placenta praevia, intrauterine growth restriction, need for induction of labor, mode of delivery, cesarean section rate, preterm delivery, and delivery beyond 41 completed weeks.
Neonatal outcome variables analyzed were birth weight less than 2.5 kg, birth weight more than 4 kg, Apgar score less than 7 at 5 min, congenital anomalies, admission to neonatal intensive care unit, respiratory distress syndrome, transient tachypnea of newborn, and shoulder dystocia.
These outcome variables were compared across three groups of parity: Group 1 with Groups 2 and 3. Comparison was also done between Groups 2 and 3 to understand and analyze the trends in the occurrence of these outcomes.
In bivariate analysis, frequency distributions were generated for each variable separately. Differences in percentages between the comparison groups were tested by χ2 test.
Relative risks (RRs) were calculated to quantify association between exposures: parity and an outcome. Estimates of standard errors and 95 % Confidence intervals (CI) were calculated by Cornfield method and Fisher’s exact method, respectively.
A p value of less than 0.05 was considered statistically significant. All analyses were carried out in STATA software 2009, version 10.1; and in Epi Info 2012, version 7.
Results
There were 1,658 multiparous women (parity 2–4), hereafter referred to as Group 1; 1,198 grand multiparous women (parity 5–9), hereafter referred to as Group 2; and 160 great grand multiparous women (parity 10 or more), hereafter referred to as Group 3.
A high proportion of previous spontaneous miscarriages was seen in Group 3 (69.8 %) and Group 2 (36.4 %) compared with Group 1 (25 %).
Comparisons of antenatal complications between the three groups are presented in Table 1.
Table 1.
Comparison of antenatal complications between the three parity groups
| Variable | Group 1 (n = 1658) % | Group 2 (n = 1198) % | Group 3 (n = 160) % | RRa (95 % CI) | P value | RRb (95 % CI) | P value | RRc (95 % CI) | P value |
|---|---|---|---|---|---|---|---|---|---|
| PIH | 75 (4.52) | 56 (4.67) | 8 (5.00) | 1.03 (0.73–1.44) | 0.849 | 1.10 (0.55–2.16) | 0.78 | 1.064 (0.54–2.06) | 0.85 |
| HTN | 12 (0.72) | 14 (1.16) | 2 (1.25) | 1.61 (0.74–3.47) | 0.216 | 1.63 (0.44–5.93) | 0.46 | 1.061 (0.28–3.91) | 0.92 |
| GDM | 88 (5.30) | 125 (10.4) | 30 (18.75) | 1.96 (1.51–2.55) | 0.0001*** | 3.32 (2.34–4.71) | 0.0001*** | 1.79 (1.24–2.56) | 0.001** |
| Diabetes | 6 (0.36) | 20 (1.66) | 7 (4.37) | 4.61 (1.85–11.45) | 0.0003*** | 6.35 (3.7–10.74) | 0.0001*** | 2.25 (1.17–4.34) | 0.021* |
| Anemia | 61 (3.67) | 100 (8.34) | 22 (13.75) | 2.26 (1.66–3.09) | 0.0001*** | 3.33 (2.25–4.93) | 0.0001*** | 1.61 (1.07–2.43) | 0.0001*** |
| Placenta praevia | 8 (0.48) | 25 (2.08) | 1 (0.62) | 4.32 (1.95–9.55) | 0.0001*** | 1.26 (0.19–8.07) | 0.80 | 0.32 (0.04–2.21) | 0.20 |
| Abnormalities of liquor volume | 13 (0.78) | 26 (2.17) | 7 (4.37) | 2.76 (1.42–5.36) | 0.0016** | 4.11 (2.22–7.61) | 0.0001*** | 1.83 (0.93–3.60) | 0.0001*** |
| Malpresentations | 23 (1.38) | 52 (4.34) | 13 (8.12) | 3.12 (1.92–5.08) | 0.0001*** | 4.37 (2.75–6.94) | 0.0001*** | 1.75 (1.05–2.92) | 0.03* |
| IUGR | 28 (1.68) | 43 (3.58) | 2 (1.25) | 2.12 (1.32–3.40) | 0.0013** | 0.75 (0.19–2.90) | 0.67 | 0.36 (0.09–1.44) | 0.12 |
* Statistically significant result; ** Statistically highly significant result; *** Statistically very highly significant result
aComparison between Groups 1 & 2
bComparison between Groups 1 & 3
cComparison between Groups 2 & 3
Risk of gestational diabetes mellitus (GDM) and incidence of anemia was found in an increasing frequency with increasing parity showing a two fold increase in women in Group 2 and more than threefold increase in Group 3 women compared with Group 1.
Established diabetes was more than four times commoner in Group 2 and more than six times commoner in Group 3 compared with Group 1.
Incidence of abnormal liquor volumes, and malpresentation at the time of delivery likewise, showed a linear increase in frequency with increasing parity showing two–fourfold increase in Groups 2 and 3 compared with Group 1 (Table 1)
Risk of intrauterine growth restriction (IUGR) increased by more than twofolds in Group 2 women compared with Group 1 (RR 2.12, 95 % CI 1.32–3.40) but this risk dropped down with further increase in parity beyond parity nine and the risk in Group 3 was similar to that of Group 1 (RR 0.75, 95 % CI 0.19–2.90).Compared with Group 2 women, Group 3 women were 64 % less likely to have IUGR.
Placenta praevia was significantly more common in Group 2 compared with Group 1 (RR 4.32 95 % CI 1.95–9.55). However, compared with Group 2 women, incidence of placenta praevia in Group 3 women was 68 % less likely.
Incidence of preexisting hypertension (HTN) and pregnancy-induced hypertension (PIH) was found comparable in all groups.
Comparisons of labor characteristics between the three groups are presented in Table 2.
Table 2.
Comparison of labor characteristics between the three parity groups
| Variable | Group 1 (n = 1658) % | Group 2 (n = 1198) % | Group 3 (n = 160) % | RRa (95 % CI) | P value | RRb (95 % CI) | P value | RRc (95 % CI) | P value |
|---|---|---|---|---|---|---|---|---|---|
| Induction of labor | 56 (3.37) | 98 (8.18) | 6 (3.75) | 2.42 (1.75–3.33) | 0.0001*** | 1.10 (0.50–2.39) | 0.80 | 0.46 (0.21–1.03) | 0.04* |
| Labor augmentation | 99 (5.97) | 32 (2.67) | 2 (1.25) | 0.44 (0.30–0.66) | 0.0001*** | 0.21 (0.05–0.85) | 0.01* | 0.49 (0.12–1.90) | 0.27 |
| Meconium stained liquor | 152 (9.16) | 128 (10.68) | 17 (10.62) | 1.16 (0.93–1.45) | 0.17 | 1.16 (0.71–1.86) | 0.54 | 0.99 (0.62–1.59) | 0.98 |
| CTG abnormalities in labor | 87 (5.24) | 91 (7.59) | 6 (3.75) | 1.44 (1.08–1.92) | 0.01* | 0.72 (0.32–1.58) | 0.41 | 0.50 (0.23–1.11) | 0.07 |
| Preterm delivery | 43 (2.59) | 63 (5.25) | 14 (8.75) | 2.02 (1.38–2.96) | 0.0002*** | 2.96 (1.83–4.79) | 0.0001*** | 1.59 (0.96–2.62) | 0.07 |
| Post-term delivery | 48 (2.89) | 128 (10.68) | 5 (3.12) | 3.69 (2.67–5.09) | 0.0001*** | 1.07 (0.46–2.50) | 0.86 | 0.29 (0.12–0.71) | 0.002** |
* Statistically significant result; ** Statistically highly significant result; *** Statistically very highly significant result
aComparison between Groups 1 & 2
bComparison between Groups 1 & 3
cComparison between Groups 2 & 3
Need for augmentation of labor decreased linearly with increasing parity. Group 2 women were 56 % less likely and Group 3 women 79 % less likely to need labor augmentation compared with women in Group 1.
Groups 2 and 3 women were, respectively, two and three times more likely to deliver before 37 completed weeks of gestation, thus showing a linear increase in the risk of preterm delivery with increasing parity.
Need for induction of labor was the highest in Group 2, the need being 2.5 times higher in these women compared with Group 1; however, with further increase in parity beyond nine, need for induction of labor in Group 3 seemed to decline by 54 % in Group 3 compared with Group 2 women.
Incidence of prolonged pregnancy beyond 41 completed weeks showed an increase with increasing parity up to parity 5, Group 2 (RR 3.69, 95 % CI 2.67–5.09) compared with Group 1; interestingly, however, this risk seemed to decrease with further increase in parity. Women in Group 3 were 71 % less likely to have pregnancy going beyond 41 weeks compared with Group 2.
Cardiotocographic abnormalities in labor were 2.5 times more likely in Group 2 compared with Group 1 but this risk declined with further increase in parity. Women in Group 3 had 50 % less cardiotocographic abnormalities during labor compared with Group 2.
There was no statistically significant difference between the three groups with regard to the incidence of meconium staining of liquor during labor.
Comparisons of mode of delivery and maternal and fetal complications of delivery are presented in Table 3.
Table 3.
Comparison of maternal and fetal complications of labor between the three parity groups
| Variable | Group 1 (n = 1658) % | Group 2 (n = 1198) % | Group 3 (n = 160) % | RRa (95 % CI) | P value | RRb (95 % CI) | P value | RRc (95 % CI) | P value |
|---|---|---|---|---|---|---|---|---|---|
| Normal delivery | 1479 (89.21) | 971 (81.05) | 139 (86.87) | 0.90 (0.87–0.93) | 0.0001*** | 0.81 (0.52–1.26) | 0.36 | 1.47 (0.95–2.29) | 0.73 |
| Instrumental vaginal delivery | 5 (0.3) | 7 (0.58) | 2 (1.25) | 1.93 (0.61–6.09) | 0.249 | 3.27 (0.005–10.66) | 0.06 | 1.89 (0.55–6.49) | 0.32 |
| Cesarean section | 174 (10.49) | 220 (18.36) | 19 (11.97) | 1.74 (1.45–2.10) | 0.0001*** | 1.13 (0.71–1.78) | 0.58 | 0.63 (0.39–0.99) | 0.04* |
| Placental abruption | 17 (1.02) | 16 (1.33) | 2 (1.25) | 1.30 (0.66–2.56) | 0.44 | 1.19 (0.32–4.48) | 0.78 | 0.94 (0.25–3.5) | 0.92 |
| Postpartum hemorrhage | 26 (1.56) | 47 (3.92) | 14 (8.75) | 2.50 (1.55–4.01) | 0.0001*** | 3.78 (2.41–5.93) | 0.0001*** | 2.03 (1.25–3.30) | 0.005** |
| Soft tissue injuries | 282 (17.00) | 121 (10.1) | 7 (4.37) | 0.59 (0.48–0.72) | 0.0001*** | 0.24 (0.11–0.51) | 0.0001*** | 0.43 (0.21–0.91) | 0.01* |
| Episiotomy | 16 (0.96) | 6 (0.5) | 1 (0.62) | 0.51 (0.20–1.32) | 0.161 | 0.66 (0.09–4.48) | 0.0001*** | 1.21 (0.19–7.49) | 0.83 |
* Statistically significant result; ** Statistically highly significant result; *** Statistically very highly significant result
aComparison between Groups 1 & 2
bComparison between Groups 1 & 3
cComparison between Groups 2 & 3
Significantly greater number of Group 2 women compared with Group 1 delivered by cesarean section (RR 1.74, 95 % CI 1.45–2.10). However, it was noted that in Group 3 women, the need for cesarean delivery dropped by 37 % in comparison with Group 2. The incidence in Group 3 remained similar to that of Group 1 (11.62 vs 10.49 %). Incidence of soft tissue injuries decreased with increasing parity (4.18 % in Group 3 vs 17 % in Group 1). There were no differences between the occurrences of placental abruption and instrumental vaginal delivery in the three groups. Postpartum hemorrhage showed a dramatic increase in incidence with increasing parity, and the risk was 2.5 times in Group 2 (RR 2.50, 95 % CI 1.55–4.01) and 3.5 times in Group 3(RR 3.78, 95 % CI 2.41–5.93) compared with Group 1. There were no cases of rupture of the uterus or maternal mortality during the study period.
Common indications for cesarean section are described in Table 4. Significantly, greater number of women in Groups 2 and 3 had cesarean sections for the indication of non-progress of labor in comparison with the women in Group 1. However, on comparing this outcome of Group 3 with Group 2, it was noted that the observed increment in risk was not statistically significant.
Table 4.
Common indications for cesarean section in three parity groups
| Variable | Group 1 (n = 1658) % | Group 2 (n = 1198) % | Group 3 (n = 160) % | RRa (95 % CI) | P value | RRb (95 % CI) | P value | RRc (95 % CI) | P value |
|---|---|---|---|---|---|---|---|---|---|
| Fetal distress | 36 (2.17) | 41 (3.42) | 4 (2.50) | 1.57 (1.01–2.45) | 0.041* | 1.13 (0.44–2.92) | 0.78 | 0.74 (0.29–1.92) | 0.54 |
| Non progress of labor | 25 (1.5) | 67 (5.60) | 10 (6.25) | 3.70 (2.35–5.83) | 0.0001*** | 3.39 (1.96–5.86) | 0.0001*** | 1.10 (0.61–2.01) | 0.73 |
| Malpresentations | 23 (1.38) | 52 (4.34) | 13 (8.12) | 3.12 (1.92–5.08) | 0.0001*** | 4.37 (2.75–6.94) | 0.0001*** | 1.75 (1.05–2.92) | 0.03* |
| Placenta praevia | 5 (0.30) | 23 (1.91) | 1 (0.62) | 6.36 (2.42–16.69) | 0.0001*** | 1.89 (0.31–11.43) | 0.49 | 0.34 (0.05–2.39) | 0.24 |
| Previous two or more cesarean sections | 22 (1.32) | 50 (4.17) | 5 (3.12) | 3.14 (1.91–5.16) | 0.0001*** | 2.13 (0.95–4.78) | 0.07 | 0.76 (0.32–1.78) | 0.52 |
* Statistically significant result; *** Statistically very highly significant result
aComparison between Groups 1 & 2
bComparison between Groups 1 & 3
cComparison between Groups 2 & 3
Neonatal outcomes and their comparisons across three groups are depicted in Table 5.
Table 5.
Comparison of neonatal outcomes in three parity groups
| Variable | Group 1 (n = 1658) % | Group 2 (n = 1198) % | Group 3 (n = 160) % | RRa (95 % CI) | P value | RRb (95 % CI) | P value | RRc (95 % CI) | P value |
|---|---|---|---|---|---|---|---|---|---|
| Birth weight >4 kg | 30 (1.80) | 49 (4.09) | 13 (8.12) | 2.26 (1.44–3.53) | 0.0002*** | 3.65 (2.25–5.89) | 0.0001*** | 1.84 (1.11–3.06) | 0.02* |
| Low birth weight | 68 (4.10) | 66 (5.50) | 6 (3.75) | 1.34 (0.96–1.86) | 0.079 | 0.91 (0.42–2.00) | 0.82 | 0.69 (0.31–1.51) | 0.35 |
| 5 min Apgar score <7 | 11 (0.66) | 125 (10.4) | 1 (0.62) | 1.13 (0.47–2.72) | 0.78 | 0.94 (0.14–6.21) | 0.95 | 0.84 (0.13–5.4) | 0.86 |
| NICU admission | 79 (4.76) | 9 (0.75) | 7 (4.37) | 1.13 (0.82–1.56) | 0.42 | 0.92 (0.44–1.90) | 0.82 | 0.81 (0.39–1.67) | 0.57 |
| Congenital anomalies | 13 (0.78) | 65 (5.42) | 3 (1.87) | 1.38 (0.64–2.97) | 0.40 | 2.15 (0.76–6.03) | 0.15 | 1.60 (0.57–4.49) | 0.34 |
| Respiratory distress syndrome | 6 (0.36) | 7 (0.58) | 1 (0.62) | 1.61 (0.54–4.79) | 0.38 | 1.62 (0.26–10.04) | 0.60 | 1.06 (0.16–6.67) | 0.94 |
| Transient tachypnoea of newborn | 5 (0.54) | 7 (0.58) | 1 (0.62) | 1.07 (0.40–2.88) | 0.88 | 1.13 (0.17–7.34) | 0.89 | 1.06 (0.16–6.67) | 0.94 |
| Shoulder dystocia | 3 (0.18) | 9 (0.75) | 1 (0.62) | 4.15 (1.12–15.30) | 0.02* | 2.85 (0.51–15.6) | 0.25 | 0.84 (0.13–5.47) | 0.86 |
* Statistically significant result; *** Statistically very highly significant result
aComparison between Groups 1 & 2
bComparison between Groups 1 & 3
cComparison between Groups 2 & 3
The RR of delivering a fatter baby weighing more than 4 kg was greater than twice in Group 2 women and greater than 3.5 times in Group 3 women in comparison with Group 1.
The RR of shoulder dystocia in Group 2 was greater than four times compared with Group 1. When Group 3 was compared with Group 2, it was found that Group 3 women were 26 % less likely to have shoulder dystocia compared with Group 2.
Risk of congenital anomalies, admission to neonatal intensive care unit (NICU), low Apgar scores, respiratory distress syndrome, and transient tachypnea of newborn were not significantly different across the three groups. Overall perinatal mortality was low, and it was similar in all the three groups.
Discussion
Babinszki and Thomas [2] in their study have compared multipara with grand multipara and grand multipara with great grand multipara. Their study is the closest to the present study in design. However, in our study, we also compared the results between multipara and great grand multipara in addition to the groups mentioned in their study. Such comparison helped us in understanding the trends in the occurrences of various obstetric and neonatal complications, and in identifying also the particular risks to which each group was exposure prone.
As the women younger than 18 years and women older than 35 years were excluded from the study population, we have removed the possible contribution of extremes of reproductive age on obstetrical and neonatal outcomes.
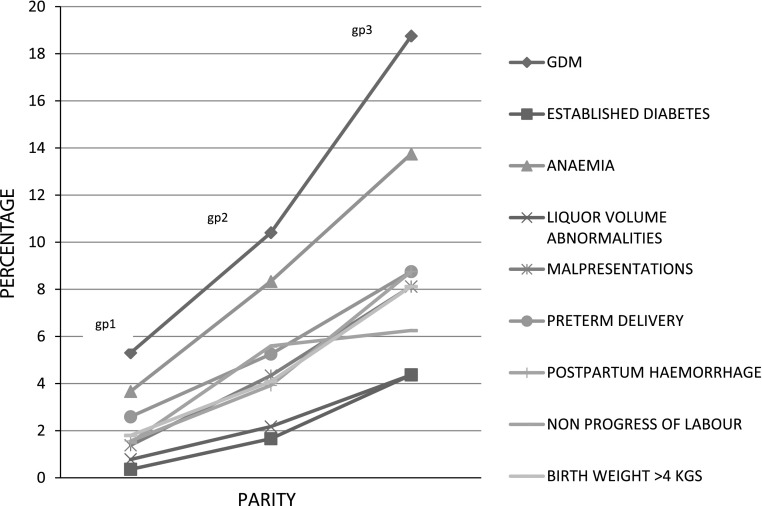
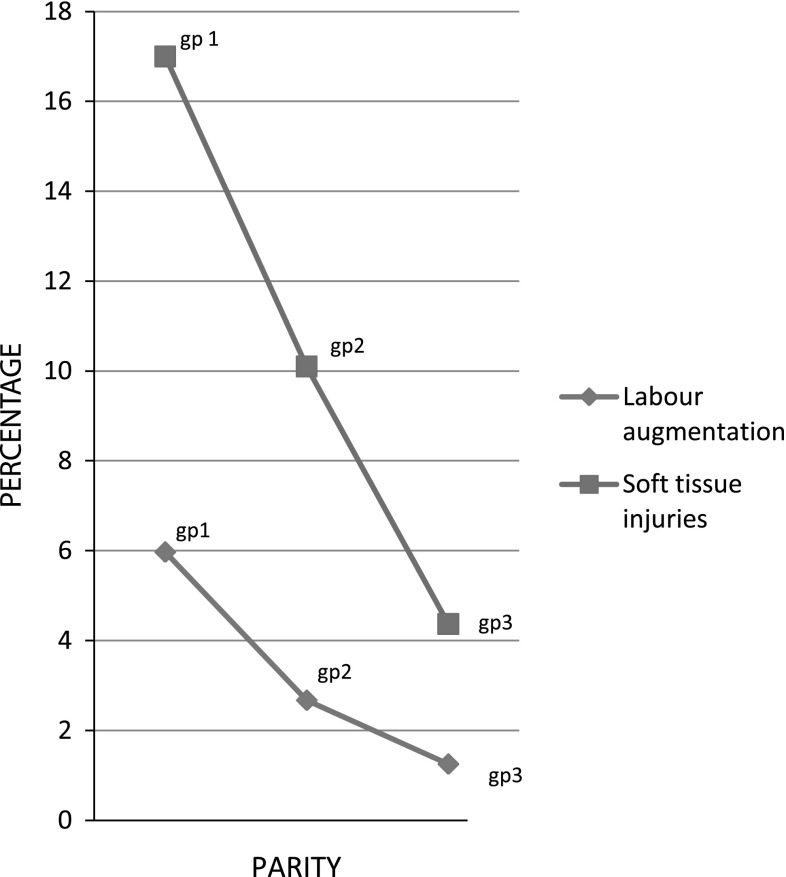
An important finding of this study is that in this population, different complications revealed different trends with increasing parity. While many antenatal and intrapartum complications like diabetes (overt and gestational), anemia, preterm delivery, malpresentation at term, postpartum hemorrhage, macrosomia showed a significant linear increase with increasing parity as indicated by χ2 test for linear trend (Fig. 1) as also reported by many other studies [3–9]; there were some, like the need for labor augmentation with its attendant risks specially in women of higher parity and soft tissue injuries, which showed a significantly declining trend with increasing parity as indicated by χ2 test for linear trend (Fig. 2). Similar observation has also been reported by Ezimokhai et al. [1].
Fig. 1.
Complications showing linear increasing trends with increasing parity
Fig. 2.
Complications showing decreasing trends with increasing parity
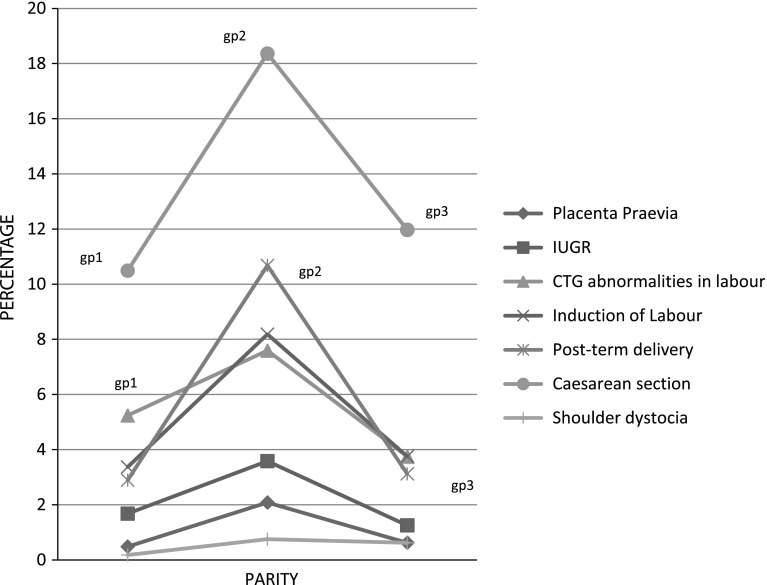
A really interesting observation of this study was that some complications indeed followed an inverted V curve, showing an increase in their occurrence up to parity nine but decline after that with further increase in parity of ten or beyond. These complications were placenta praevia, intrauterine growth restriction, need for induction of labor, cesarean delivery, delivery beyond 41 weeks, CTG abnormalities in labor, and shoulder dystocia (Fig. 3). However, keeping in mind the limitation of cohort studies for outcomes with rare occurrences, and since the sample size in Group 3 is not so large, it is difficult to convincingly conclude about some such outcomes like shoulder dystocia. Nonetheless, this study does provide an evidence for possible associations between these complications and parity in Emirati women, which need to be confirmed further with the help of a larger study.
Fig. 3.
Complications showing an inverted V curve with increasing parity
This paradoxical observation of inverted V curve may indicate contribution of self-selection and filtering effect wherein women who develop obstetrical complications in their initial few pregnancies may end their childbearing at lower parities and thus are filtered out from the healthier counterparts who have had uncomplicated pregnancies and who thus proceed further in their reproductive potential to become great grand multipara [10]. Whether this observation of inverted V curve of many obstetrical complications is due to this “healthy person effect” remains a matter of indirect assumptive conclusion.
Significantly greater number of women in grand and great grand multiparity group undergoing cesarean sections for the indication of non progress of labor may indicate a need for better understanding of labor curves of women of higher parity. As Edith D Gurewitsch has observed in his study on labor curves of grand multiparous women, it is noteworthy to keep in mind that while progressing from low parity to grand multiparity, the average labor curve continues to change, but not toward an ever improved progress [11]. His study points out that the average labor curve of the grand multiparous women overlaps that of nulliparous women initially and overlaps that of the low parity women in the final phase but it clearly remains distinguishable from both in the middle portion, which is from dilation of 4–6 cm when the grand multiparous women still is in latent phase. Thus, non progress or poor progress beyond the dilatation of 4 cm should not be considered abnormal in grand multiparous women because she is likely to be still in the latent phase and may not accelerate the labor until 6-cm dilatation is reached. Keeping this observation in mind, intrapartum care should be provided to these women and this might help in reducing the number of cesarean deliveries performed for the indication of non progress of labor.
Conclusion
Our study findings suggest that in the Emirati population, women in different parity groups are experiencing risk of different antenatal and neonatal complications with different magnitudes. Nevertheless, there are some complications which show decrease with increasing parity. Perinatal mortality in the study populations remains very low, which suggest that in modern settings, where socioeconomic conditions are favorable and women have access to high-quality healthcare, a satisfactory maternal and fetal/neonatal outcome can be expected with low morbidity and mortality independent of their parity status.
Bethel Solomon’s concerns as expressed in his article “The dangerous multipara” in 1934 were found to be genuine about the risks associated with grand multiparity [7]. The risks definitely exist in women of grand multiparity, but it might be unreasonable to attribute all the risks to parity. Instead, the risk should be assessed based on the woman’s past obstetric and medical history. Having moved forward in the provision of modern and refined maternity care in most developing countries, these risks can be mitigated by careful antenatal risk factor identification, careful intrapartum care, judicious use of oxytocics, active management of third stage, and more frequent involvement of consultant in making the decisions for induction of labor and operative delivery.
Acknowledgments
The authors sincerely acknowledge the contribution by Dr. Suresh Ughade, PhD, FRSS, INCLEN Fellow, Faculty in Clinical Epidemiology Unit, Government Medical College, Nagpur, India to this research and thank him for his immense help with statistical analysis.
References
- 1.Rizk DEEE, Khalfan M, Ezimokhai M. Obstetric outcome in grand multipara in the United Arab Emirates: a case control study. Arch Gynecol Obstet. 2001;264:194–198. doi: 10.1007/s004040000107. [DOI] [PubMed] [Google Scholar]
- 2.Babinszki A, Thomas K. Perinatal outcome in grand and great-grand multiparity: effects of parity on obstetric risk factors. Am J Obstet Gynecol. 1999;181(3):669–4. (http://www.ncbi.nlm.nih.gov/pubmed/10486482). [DOI] [PubMed]
- 3.Evaldson GR. The grand multipara in modern obstetrics. Gynecol Obstet Invest. 1990;30(4):217–3. (http://www.ncbi.nlm.nih.gov/pubmed/2289702). [DOI] [PubMed]
- 4.Juntunen K, Kirkinen P, Kauppila A. The clinical outcome in pregnancies of grand grand multiparous women. Acta Obstet Gynecol Scand. 1997;76(8):755–9. (http://www.ncbi.nlm.nih.gov/pubmed/9348253). [DOI] [PubMed]
- 5.Fuchs K, Peretz BA, Marcovici R, et al. The “grand multipara” is it a problem? A review of 5785 cases. Int J Gynecol Obstet. 1985;23(4):321–326. doi: 10.1016/0020-7292(85)90027-X. [DOI] [PubMed] [Google Scholar]
- 6.Mwambingu FT, Al Meshari AA, Akiel A. The problem of grandmultiparity in current obstetric practice. Int J Gynaecol Obstet. 1988;26:355–9. [DOI] [PubMed]
- 7.Bugg GJ, Atwal GS, Maresh M. Grandmultiparae in a modern setting. Br J Obstet Gynecol. 2002;109:249–253. doi: 10.1111/j.1471-0528.2002.01058.x. [DOI] [PubMed] [Google Scholar]
- 8.Toohey JS, Keegan KA Jr, Morgan MA. Obstetrics: the “dangerous multipara”: fact or fiction? Am J Obstet Gynecol. 1995;172(2):683–6. (http://www.ncbi.nlm.nih.gov/pubmed/7856706). [DOI] [PubMed]
- 9.Roman H, Robillard P-Y. Obstetric and neonatal outcomes in grand multiparity. Obstet Gynecol. 2004;103(6):1294–99. [DOI] [PubMed]
- 10.Simonsen SM, Lyon JL, Alder SC, et al. Effect of grand multiparity on intrapartum and newborn complications in young women. Obstet Gynecol. 2005;106:454. (http://www.ncbi.nlm.nih.gov/pubmed/16135573). [DOI] [PubMed]
- 11.Edith DG, Paul D. The labor curve of the grand multipara: does progress of labor continue to improve with additional childbearing? Am J Obstet Gynecol. 2002;186(6):1331–1338. doi: 10.1067/mob.2002.122448a. [DOI] [PubMed] [Google Scholar]