Abstract
According to current critical care management guidelines, the overall hemodynamic optimization process seeks to restore macrocirculatory oxygenation, pressure, and flow variables. However, there is increasing evidence demonstrating that, despite normalization of these global parameters, microcirculatory and regional perfusion alterations might occur, and persistence of these alterations has been associated with worse prognosis. Such observations have led to great interest in testing new technologies capable of evaluating the microcirculation. Near-infrared spectroscopy (NIRS) measures tissue oxygen saturation (StO2) and has been proposed as a noninvasive system for monitoring regional circulation. The present review aims to summarize the existing evidence on NIRS and its potential clinical utility in different scenarios of critically ill patients.
1. Introduction
Tissue hypoxia, as results of oxygen supply-demand imbalance at the cellular level, defines circulatory insufficiency or shock. Maintained over time, this situation might lead to cellular and organ dysfunction, organ damage, and the ultimate death of the individual. In our daily clinical practice, hemodynamic resuscitation of shock states aims to restore global tissue oxygenation markers, such as venous saturations (either central or mixed) or lactate. Including these endpoint variables in the management of shock has led to remarkable improvements in the survival of critically ill patients [1]. However, there is overwhelming evidence demonstrating that, despite normalization of these global tissue hypoxia markers, perfusion disorders might persist at the microcirculatory level [2, 3]. Importantly, persistence of these alterations has been independently associated with further development of multiple organ failure (MOF) and poor outcome [4, 5]. Consequently, over the last years there has been growing interest in developing new technologies capable of assessing the regional circulation and/or the microcirculation [6, 7].
Evaluating the microcirculation in the critically ill patients has been associated with more than a few technical problems, which have delayed their use at the bedside. In addition to the technical limitations, a clinically relevant issue has been finding the right place to monitor. Since any used technology can only assess the microvascular bed of a given sampled tissue, it is necessary to choose accessible territories and yet sufficiently representative of the whole body wellness. Currently, there are several technologies available for the evaluation of the microcirculation [6], which can be classified into two main groups: (a) firstly, direct methods, which allow the visualization of the microvascular bed (such as videomicroscopy); and (b) secondly, indirect methods based on measures of tissue oxygenation, as surrogates of microcirculatory perfusion. In the latter group we can include technologies such as gastric tonometry, tissue oxygen electrodes, sublingual capnometry, and near-infrared spectroscopy (NIRS). Due to its noninvasive nature and its easy applicability, NIRS technology has aroused increasing interest in the evaluation of the regional circulation. This review aims to summarize what, today, has shown this technology in the field of the critically ill patients.
2. Near-Infrared Spectroscopy (NIRS): Basic Principles
The concept of NIRS technology has already been available for many decades, and it has been developed for different purposes, ranging from chemical analysis in agriculture to pharmaceutical and medical applications. In the late seventies, first noninvasive NIRS devices were used to monitor cerebral and myocardial oxygenation status in living tissues [8], suggesting that the NIRS spectrum of light was perfectly suited for monitoring in vivo tissue oxygen provision and utilization. Since then, many studies in humans, along with the development of portable, noninvasive NIRS systems, account for the growing interest in this technology [9, 10].
NIRS technology is based on measuring the attenuation of light in the near-infrared spectrum (700–1000 nm wavelengths) to measure the chromophores, mainly hemoglobin, present in the sampled tissue. Although many other chromophores can influence the obtained NIRS signal (such as bilirubin, melanin, myoglobin, and cytochrome a,a3), choosing specific wavelengths allows for minimizing the impact of these substances, and the obtained signal is derived mainly from oxy- and deoxyhemoglobin. The equipment required for an NIRS system consists of a light source, optical bundles (optodes) for light emission and reception, a processor, and a display system [9]. The distance between the point of light entry and exit (optode separation) will determine the magnitude of sampled tissue. The NIRS signal is derived mainly from the hemoglobin contained in the entire vascular tree and mainly small vessels (arterioles, capillaries, and venules) present in the sampled area [9–13]. Finally, oxy- and deoxyhemoglobin measures permit calculating the overall saturation for tissue hemoglobin or tissue oxygen saturation (StO2) [13]. NIRS systems can also provide an estimation of the amount of hemoglobin contained in the sampled area, displayed as total tissue hemoglobin (HbT) or absolute tissue hemoglobin index (THI).
Although StO2 has been evaluated in several organs (brain, kidney, and liver), for resuscitation purposes, skeletal muscle StO2, due to its nonvital peripheral organ condition, has emerged as a potential early detector of occult hypoperfusion. This review will focus on the usefulness of StO2 derived from skeletal muscle in the critical patient. Several muscle locations have been used in the critical care setting. Since StO2 measurements derived from the NIRS signal might be altered by local factors such as edema and adipose tissue thickness, some authors have proposed the thenar eminence as a reliable site, less subject to inter- and intraindividual variabilities [13, 14]. Although the thenar eminence is the most widely tested area, interesting results have been obtained also when measuring StO2 on muscle locations, such as masseter, deltoid, and the knee area [15, 16]. In healthy basal conditions, the NIRS signal reflects predominantly the venous oxygenation, since an estimated 75% of the blood present in the skeletal muscle is located in the venous compartment [9]. In 700 healthy volunteers, the baseline StO2 value measured in the thenar eminence was 87% ± 6% [17]. Similar to mixed venous oxygen saturation, StO2 reflects the balance between local oxygen supply and consumption, and any measured change in StO2 could be interpreted in both directions: changes in local microcirculatory flow and/or changes in local consumption. Moreover, inversely proportional changes in local flow and consumption could lead to relatively stable values of StO2 [6].
3. Vascular Occlusion Test (VOT)
In addition to monitoring the absolute StO2 value in the thenar eminence, the StO2 response to a brief ischemic challenge has been explored, in order to obtain dynamic information on tissue performance. The so-called vascular occlusion test (VOT) consists in executing an arterial occlusion, proximal to the StO2 probe (usually by means of a tourniquet system on the forearm), until a given ischemic threshold is reached, and then the occlusion is released. This test allows generating some dynamic parameters and specially the initial Hb deoxygenation slope (or DeO2; expressed as % over time) in the phase of ischemia, followed by the Hb reoxygenation slope (or ReO2; also expressed in % over time) once the vascular occlusion is released (Figure 1).
Figure 1.
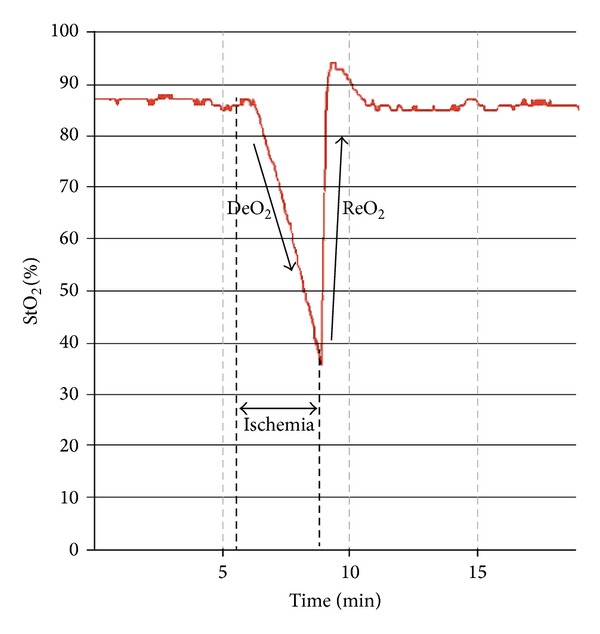
StO2 response to a vascular occlusion test (VOT). The transient ischemia generates two main parameters: the deoxygenation response (DeO2) and the reoxygenation response (ReO2). StO2: tissue oxygen saturation; DeO2: deoxygenation slope; ReO2: reoxygenation slope.
Since DeO2 represents the progressive Hb desaturation in a zero-flow situation, it has been proposed as a marker of local oxygen extraction. Correcting the DeO2 slope for the estimated local amount of Hb derives a parameter of local oxygen consumption, expressed as nirVO2, as proposed by Skarda et al. [21]: nirVO2 = (DeO2)−1/[ (THIstart + THIend)/2]. On the other hand, ReO2 reflects the Hb resaturation, and this will directly depend on blood inflow and capillary recruitment after the hypoxic stimulus. ReO2 has been named as a reflection of endothelial function; however, several observations have also correlated ReO2 to perfusion pressure [23, 24], and, thus, the resulting ReO2 seems to be derived from the interaction of perfusion pressure and endothelial integrity. In its recovery, absolute StO2 may temporarily raise the above previous baseline values, indicating postischemic vasodilation and capillary recruitment, also known as reactive hyperemia (Figure 1).
Different VOT methodologies have been described, some of them aimed at maintaining a fixed time of ischemia (3–5 minutes), and some of them sought for an ischemic threshold (StO2 drops until a specific value). The lack of standardization of the VOT has led to great difficulties when trying to compare results from different studies. This fundamental issue represents an important limitation of the test, along with the variety of sampled depths and sites used to measure the StO2 response to ischemia [14, 25]. According to the existing literature [14, 25], maintaining the ischemic stimulus until a determined StO2 value is achieved seems to minimize inter-individual variations, thus homogenizing ReO2 values for their comparison. Future consensus should also be applied to the location and depth of measurement of StO2 [14].
4. StO2 in the Critically Ill Patients
While the NIRS technology was developed several decades ago, the new noninvasive and portable NIRS systems emerged as an attractive technology for early detection of shock states in armed conflicts. Thus, initial efforts addressed mainly the value of these systems in hypovolemic shock. After some promising results, NIRS was also explored in other critical conditions and particularly in septic shock.
4.1. StO2 in Hypovolemic Shock
In low blood flow states secondary to hypovolemia (such as hemorrhagic shock) the activation of the sympathetic nervous system causes blood flow redistribution from the periphery to the central compartment, through vasoconstriction in certain territories, in order to maintain an optimal perfusion of vital organs [26]. This compensatory mechanism can mask significant hypovolemia associated with hypoperfusion in certain territories, with significant negative impact on outcome [1]. Accordingly, in situations of hypovolemia, a decrease in blood flow to skeletal muscle is expected, with increases in oxygen extraction and decreases in the content of hemoglobin at the regional level. Thus, hypothetically, the evaluation of peripheral perfusion by using StO2 seems highly interesting as an early marker of tissue hypoperfusion caused by hypovolemia [27].
This hypothesis was initially tested in experimental conditions, in animal models of hemorrhagic shock. First observations correlated StO2 to global variables of flow and oxygen delivery [28–30], suggesting that regional oxygenation measured by NIRS would be able to noninvasively detect progressive hypovolemia. Crookes et al. [31], in a prospective model of resuscitation from hemorrhagic shock, concluded that StO2 was a better discriminator for survivors to hemorrhage than mixed venous oxygen saturation (SvO2), blood lactate, and base deficit. In human models of central hypovolemia in healthy subjects, StO2 and the tissue hemoglobin index (THI) fall have been shown to detect decreases in blood volume equivalent to 400–500 cc, even before the onset of tachycardia or hypotension [32–34]. In addition to its ability to detect progressive hypovolemia, StO2 has also been tested for its utility in guiding intravascular volume optimization. On that behalf, Cohn et al., in a prospective randomized pilot study in patients undergoing elective colorectal surgery, analyzed the impact of a standard versus restrictive fluid approach on tissue oxygenation and development of complications [35]. The authors concluded that the restrictive approach was not associated with lower StO2 values, suggesting that StO2 would be a useful parameter for guiding fluid administration during surgery, ensuring tissue wellness, and avoiding unnecessary fluid overload, which has repeatedly been associated to higher morbidity derived from surgery [36, 37].
In trauma patients, StO2 correlation to parameters of flow and oxygen delivery has been also verified [38]. Furthermore, the absolute value of StO2 has repeatedly demonstrated its prognostic value in this patient population. Low StO2 values during the initial approach to these patients have been associated with larger transfusion requirements [39–41], increased risk of infection [42], multiorgan failure [42, 43], and even higher mortality rates [43, 44]. Importantly, this predictive value was maintained in apparently stable hemodynamic conditions (defined as systolic blood pressure > 90 mmHg) [40, 41]. In addition to absolute StO2 values, dynamic variables derived from the VOT have also shown their prognosis in trauma patients [45, 46]. In a recent publication, Guyette et al. [45] demonstrated that early alterations in DeO2 were independently associated with the need for early interventions (red blood cell transfusion, emergent surgery, etc.). In this observational study, DeO2 was superior to absolute StO2 for predictive purposes. Once again, this association was independent and more sensitive than other physiological variables, such as heart rate or blood pressure. Despite the cumulative evidence on the prognostic value of StO2 in trauma, with its potential use for early identification of at-risk patients, to this day, there is a lack of prospective studies exploring the usefulness of StO2 in trauma resuscitation algorithms, either as a trigger for interventions or as a target in the hemodynamic resuscitation process.
4.2. StO2 in Severe Sepsis and Septic Shock
The value of StO2 has been also widely explored in patients with severe sepsis and septic shock. While absolute StO2 values have shown robust prognostic implications in trauma patients, in septic conditions this association appears to be more complex [15, 47, 48]. Although septic patients tend to show lower StO2 values than healthy subjects, there is a huge overlap between these populations [19]. These observations could be derived from the heterogeneous nature of microcirculatory alterations in sepsis (ischemic and highly oxygenated coexisting areas), with an overall “normal” oxygen content in a given sensed area [27]. The low sensitivity for these conditions would be a major limitation of absolute StO2. Nevertheless, dynamic StO2 VOT-derived variables have yielded much more promising results than the absolute StO2 in terms of prognosis.
Several authors have reported alterations in the StO2 response to the VOT in sepsis, and the magnitude of such alteration has been directly correlated with the development of organ failure, ICU length of stay, or even mortality [15, 18, 20, 23, 49] (Table 1). Alterations in DeO2, represented by lower deoxygenation rates, have been associated with poor prognosis. Since DeO2 reflects local oxygen consumption, it seems reasonable to hypothesize that patients with limited oxygen extraction will develop higher degrees of organ failure [18, 23]. This local oxygen consumption limitation may be due to two different but cumulative mechanisms: (a) a local supply-demand dependency on low flow or inadequate flow conditions or (b) a low oxygen extraction at the cellular level due to mitochondrial dysfunction and/or alteration of oxygen diffusion (interstitial edema) [23, 50]. Regrettably, the NIRS technology is unable to determine which of these two mechanisms presents greater contribution to the final DeO2. Regarding the ReO2 slope, it is also diminished in septic patients when compared to healthy subjects [19, 20, 22, 23, 48]. Moreover, the magnitude of ReO2 decreased slope has also been correlated to the severity of the episode, and some studies have even demonstrated association with mortality [19, 22, 48]. Not only the initial ReO2 value but the persistence of alterations in ReO2 during resuscitation has been associated with worse prognosis [19].
Table 1.
Summarized prognostic studies on StO2 with VOT-derived parameters in septic patients.
| Study | Patient population (n) | Inclusion time | StO2 site/depth | VOT | MAP (mmHg) | DeO2
(%/min) |
ReO2
(%/sec) |
Mortality | Comments |
|---|---|---|---|---|---|---|---|---|---|
| Parežnik et al. [18] | SS (6) and SShock (6) | First 48 h (after stabilization) | TH 15 mm | StO2 40% | — | SS −10.4 (−7.8, −13.3) SShock −7 (−3.6, −11) |
— | No correlation to StO2-derived variables | DeO2 correlated to SOFA score |
|
| |||||||||
| Creteur et al. [19] | SS and SShock (72) | First 24 h | TH 25 mm | 3 min | 72 (67–79) | — | SShock 2 (1.2, 2.9) versus no SShock 3.2 (1.8, 4.5) (P < 0.05) |
ReO2 correlated to mortality SV 3.2 ± 1.3 NonSV 1.9 ± 1.3 (P < 0.05) |
AUC 0.797 ReO2 cut-off 2.55 (S 85%, E 73%) |
|
| |||||||||
| Doerschug et al. [20] | Sepsis (24) | First 24 h | TH 15 mm | 5 min | 69 (max 90, min 55) |
— | Moderate sepsis 3.6 ± 1.2 Severe sepsis 2.3 ± 1.5 |
ReO2 tended to be higher in SV than in NonSV 3.3 ± 1.4 versus 2.5 ± 1.5 (P 0.2) |
|
|
| |||||||||
| Skarda et al. [21] | SS and SShock (10) | ICU admission | TH 15 mm | 3 min | 73 ± 11 | −11.2 ± 2.4 | 2.3 ± 1.0 | No association between StO2 variables and mortality | |
|
| |||||||||
| Payen et al. [22] | SShock (43) | First 24 h (after vasopressors) | TH 25 mm | 3 min | 75 (65–82) | −18.6 (−28.2, −14.4) |
2.79 (1.75, 4.52) | ReO2 correlated to mortality SV 3.9 (2.2, 6.0) NonSV 1.9 (1.6, 2.8) (P 0.003) |
AUC 0.77 ReO2 cut-off 2.83 (S 87%, E 67%) |
|
| |||||||||
| Mesquida et al. [23] | SShock (33) | First 24 h, once MAP > 65 mmHg | TH 15 mm | StO2 40% | 79 ± 12 | −12.2 ± 4.2 SOFAimp −13.8 ± 4.3 SOFAnonimp −9.8 ± 2.9 |
3.02 ± 1.7 | DeO2 tended to be lower in NonSV than in SV (P ns) |
DeO2 associated with SOFA evolution and ICU-LOS ReO2 associated with ICU-LOS |
StO2: tissue oxygen saturation; VOT: vascular occlusion test; DeO2: StO2-deoxygenation slope; ReO2: StO2-reoxygenation slope; SS: severe sepsis; SShock: septic shock; TH: thenar; SOFA: sequential organ failure assessment; SV: survivors; NonSV: nonsurvivors; AUC: area under the curve; SOFAimp: SOFA improvers at day 2; SOFAnonimp: SOFA nonimprovers at day 2; LOS: length of stay.
5. Adding StO2 to Current Resuscitation Algorithms?
Although, as we have exposed, StO2 has consistently demonstrated its prognostic value in critically ill patients, there is still so much to explore in terms of its clinical applicability at the bedside. One of the major issues that needs to be faced is where to incorporate StO2 in hemodynamic resuscitation algorithms and, of course, testing whether StO2 incorporation is associated with improvement in outcomes.
5.1. Early
Due to its condition of noninvasive continuous measurement of regional oxygenation status, StO2 was initially explored in its ability to early detect hypoperfusion, and previously to monitor parameters that require invasive procedures or laboratory analysis. Some authors explored the correlation of StO2 with parameters of global oxygenation, such as central venous oxygen saturation (ScvO2) [51–55], demonstrating that low StO2 values (i.e., StO2 < 75% when measured on the thenar eminence) specifically predict extremely low ScvO2 values [15, 51, 52]. However, the sensitivity of StO2 variables to detect these situations of global hypoperfusion is considerably low, and therefore the absolute StO2 value has been proposed as an initial tool to rapidly and noninvasively detect hypoperfusion states, but only while other more sensitive variables are not available [23, 51, 52]. In conclusion, in situations of apparent hemodynamic stability in which we do not have invasive oxygenation parameters, NIRS-derived variables might be useful in the detection of at-risk patients, justifying the need for the beginning of the reanimation process, as well as a more aggressive monitoring [45, 51].
5.2. Late
Cumulative evidence on the association between microcirculatory alterations persistence, despite normalization of macrohemodynamic variables, and poor prognosis [1] has led to the idea that evaluating regional oxygenation parameters should be performed at the end of conventional “global” resuscitation. In addition to several in vivo videomicroscopy studies, Lima et al. recently found, in a population of septic patients, that alterations in StO2 values at the end of the Early Goal-Directed Therapy (EGDT) were associated with higher degrees of organ failure and mortality [16]. Some other studies have also shown consistent data regarding StO2 parameters and prognosis despite macrohemodynamic normalization [16, 23]. Unfortunately and once again, there is a lack of prospective interventional studies analyzing the usefulness of adding StO2 to the resuscitation algorithm. The fact that whether StO2 might be used instead of or complementary to current global tissue oxygenation endpoints, such as ScvO2 and lactate, deserves further investigation. In a small pilot study, Nardi et al. [56] attempted to incorporate the StO2 measured at three different locations as an endpoint parameter for resuscitation in septic patients. In their protocol, once ScvO2 values were normalized according to the Surviving Sepsis Campaign guidelines, StO2 goals were pursued in the treatment group. The authors found no benefit in the inclusion of StO2 in the resuscitation algorithm. However, the small sample size, the use of the absolute value of StO2 instead of dynamic parameters (DeO2 or ReO2), and the fact that a large percentage of patients in the treatment group did not even normalize the endpoint ScvO2 values might account for the lack of differences observed in the evolution of the patients.
One might conclude that prospective studies are needed to evaluate the usefulness of adding StO2 to our current macrohemodynamic approach to resuscitation. This major limitation would be applied, to date, to every single regional or microcirculatory monitoring system.
6. Further StO2 Applications in Intensive Care
In addition to its potential application in shock states, the StO2 may have utility in other clinical scenarios in critical care. Continuous StO2 monitoring has shown encouraging results in cardiovascular performance challenges, as in weaning from mechanical ventilation [57]. In a recent study, our group noted that changes in DeO2 within a 30-minute spontaneous breathing trial discriminated patients who would succeed in from those who would fail the disconnection from mechanical ventilation process [57], supporting the role of StO2 as a monitoring system for detecting limited cardiovascular reserve.
7. Technology Limitations
Several limiting factors deserve mention, as they might interfere in StO2 values and/or interpretation [58, 59]: (a) exogenous factors, such as changes in environment temperature; (b) endogenous factors such as age, obesity, body temperature, tissue edema, vascular diseases, and agitation; (c) drugs that modify vascular tone [24]. We already commented on the fact that the heterogeneous nature of microcirculatory alterations in septic shock might limit the value of some of the data obtained using the NIRS technology [27]. Finally, it is important to account for an important consideration about this technique: NIRS is a relatively new technology for monitoring the regional circulation in critical care, where no “gold standard” has been validated. However, instead of representing a limitation, the latter might stand for an “everything needs to be done” in regional perfusion and microcirculation in the critically ill patients.
8. Conclusions
In conclusion, StO2 and its dynamic variables derived from the VOT have demonstrated their prognostic value in several critical scenarios. The lack of randomized controlled trials analyzing their inclusion in the resuscitation process is the main constraint to the use of this technology at the present time. In addition to its potential value in resuscitation, StO2 variables might be useful in other clinical settings, where cardiovascular performance needs to be challenged, such as weaning from mechanical ventilation.
References
- 1.Mesquida J, Borrat X, Lorente JA, Masip J, Baigorri F. Objectives of hemodynamic resuscitation. Medicina Intensiva. 2011;35(8):499–508. doi: 10.1016/j.medin.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 2.den Uil CA, Lagrand WK, van der Ent M, et al. Impaired microcirculation predicts poor outcome of patients with acute myocardial infarction complicated by cardiogenic shock. European Heart Journal. 2010;31(24):3032–3039. doi: 10.1093/eurheartj/ehq324. [DOI] [PubMed] [Google Scholar]
- 3.de Backer D, Creteur J, Preiser J, Dubois M, Vincent J. Microvascular blood flow is altered in patients with sepsis. American Journal of Respiratory and Critical Care Medicine. 2002;166(1):98–104. doi: 10.1164/rccm.200109-016oc. [DOI] [PubMed] [Google Scholar]
- 4.de Backer D, Donadello K, Sakr Y, et al. Microcirculatory alterations in patients with severe sepsis: impact of time of assessment and relationship with outcome. Critical Care Medicine. 2013;41(3):791–799. doi: 10.1097/CCM.0b013e3182742e8b. [DOI] [PubMed] [Google Scholar]
- 5.Trzeciak S, McCoy JV, Dellinger RP, et al. Early increases in microcirculatory perfusion during protocol-directed resuscitation are associated with reduced multi-organ failure at 24 h in patients with sepsis. Intensive Care Medicine. 2008;34(12):2210–2217. doi: 10.1007/s00134-008-1193-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Backer D, Ospina-Tascon G, Sagado D, Favory R, Creteur J, Vincent J. Monitoring the microcirculation in the critically ill patient: current methods and future approaches. Intensive Care Medicine. 2010;36(11):1813–1825. doi: 10.1007/s00134-010-2005-3. [DOI] [PubMed] [Google Scholar]
- 7.de Backer D, Donadello K, Cortes DO. Monitoring the microcirculation. Journal of Clinical Monitoring and Computing. 2012;26:361–366. doi: 10.1007/s10877-012-9383-8. [DOI] [PubMed] [Google Scholar]
- 8.Jobsis FF. Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science. 1977;198(4323):1264–1267. doi: 10.1126/science.929199. [DOI] [PubMed] [Google Scholar]
- 9.Simonson SG, Piantadosi CA. Near-infrared spectroscopy: clinical applications. Critical Care Clinics. 1996;12(4):1019–1029. doi: 10.1016/s0749-0704(05)70290-6. [DOI] [PubMed] [Google Scholar]
- 10.Boushel R, Piantadosi CA. Near-infrared spectroscopy for monitoring muscle oxygenation. Acta Physiologica Scandinavica. 2000;168(4):615–622. doi: 10.1046/j.1365-201x.2000.00713.x. [DOI] [PubMed] [Google Scholar]
- 11.Mancini DM, Bolinger L, Li H, Kendrick K, Chance B, Wilson JR. Validation of near-infrared spectroscopy in humans. Journal of Applied Physiology. 1994;77(6):2740–2747. doi: 10.1152/jappl.1994.77.6.2740. [DOI] [PubMed] [Google Scholar]
- 12.Taylor DE, Simonson SG. Use of near-infrared spectroscopy to monitor tissue oxygenation. New Horizons. 1996;4(4):420–425. [PubMed] [Google Scholar]
- 13.Myers DE, Anderson LD, Seifert RP, et al. Noninvasive method for measuring local hemoglobin oxygen saturation in tissue using wide gap second derivative near-infrared spectroscopy. Journal of Biomedical Optics. 2005;10(3):p. 034017. doi: 10.1117/1.1925250. [DOI] [PubMed] [Google Scholar]
- 14.Gómez H, Mesquida J, Simon P, et al. Characterization of tissue oxygen saturation and the vascular occlusion test: influence of measurement sites, probe sizes and deflation thresholds. Critical Care. 2009;13(supplement 5, article S3) doi: 10.1186/cc8001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Colin G, Nardi O, Polito A, et al. Masseter tissue oxygen saturation predicts normal central venous oxygen saturation during early goal-directed therapy and predicts mortality in patients with severe sepsis. Critical Care Medicine. 2012;40(2):435–440. doi: 10.1097/CCM.0b013e3182329645. [DOI] [PubMed] [Google Scholar]
- 16.Lima A, van Bommel J, Jansen TC, Ince C, Bakker J. Low tissue oxygen saturation at the end of early goal-directed therapy is associated with worse outcome in critically ill patients. Critical Care. 2009;13, article S13 doi: 10.1186/cc8011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crookes BA, Cohn SM, Bloch S, et al. Can near-infrared spectroscopy identify the severity of shock in trauma patients? Journal of Trauma. 2005;58(4):806–816. doi: 10.1097/01.ta.0000158269.68409.1c. [DOI] [PubMed] [Google Scholar]
- 18.Parežnik R, Knezevic R, Voga G, Podbregar M. Changes in muscle tissue oxygenation during stagnant ischemia in septic patients. Intensive Care Medicine. 2006;32(1):87–92. doi: 10.1007/s00134-005-2841-8. [DOI] [PubMed] [Google Scholar]
- 19.Creteur J, Carollo T, Soldati G, Buchele G, de Backer D, Vincent J. The prognostic value of muscle StO2 in septic patients. Intensive Care Medicine. 2007;33(9):1549–1556. doi: 10.1007/s00134-007-0739-3. [DOI] [PubMed] [Google Scholar]
- 20.Doerschug KC, Delsing AS, Schmidt GA, Haynes WG. Impairments in microvascular reactivity are related to organ failure in human sepsis. American Journal of Physiology. 2007;293(2):H1065–H1071. doi: 10.1152/ajpheart.01237.2006. [DOI] [PubMed] [Google Scholar]
- 21.Skarda DE, Mulier KE, Myers DE, Taylor JH, Beilman GJ. Dynamic near-infrared spectroscopy measurements in patients with severe sepsis. Shock. 2007;27(4):348–353. doi: 10.1097/01.shk.0000239779.25775.e4. [DOI] [PubMed] [Google Scholar]
- 22.Payen D, Luengo C, Heyer L, et al. Is thenar tissue hemoglobin oxygen saturation in septic shock related to macrohemodynamic variables and outcome? Critical Care. 2009;13(supplement 5, article S6) doi: 10.1186/cc8004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mesquida J, Espinal C, Gruartmoner G, et al. Prognostic implications of tissue oxygen saturation in human septic shock. Intensive Care Medicine. 2012;38:592–597. doi: 10.1007/s00134-012-2491-6. [DOI] [PubMed] [Google Scholar]
- 24.Georger J, Hamzaoui O, Chaari A, Maizel J, Richard C, Teboul J. Restoring arterial pressure with norepinephrine improves muscle tissue oxygenation assessed by near-infrared spectroscopy in severely hypotensive septic patients. Intensive Care Medicine. 2010;36(11):1882–1889. doi: 10.1007/s00134-010-2013-3. [DOI] [PubMed] [Google Scholar]
- 25.Mayeur C, Campard S, Richard C, Teboul J. Comparison of four different vascular occlusion tests for assessing reactive hyperemia using near-infrared spectroscopy. Critical Care Medicine. 2011;39(4):695–701. doi: 10.1097/CCM.0b013e318206d256. [DOI] [PubMed] [Google Scholar]
- 26.Bonanno FG. Physiopathology of shock. Journal of Emergencies, Trauma and Shock. 2011;4(2):222–232. doi: 10.4103/0974-2700.82210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lipcsey M, Woinarski N, Bellomo R. Near infrared spectroscopy (NIRS) of the thenar eminence in anesthesia and intensive care. Annals of Intensive Care. 2012;2, article 11 doi: 10.1186/2110-5820-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rhee P, Langdale L, Mock C, Gentilello LM. Near-infrared spectroscopy: continuous measurement of cytochrome oxidation during hemorrhagic shock. Critical Care Medicine. 1997;25(1):166–170. doi: 10.1097/00003246-199701000-00030. [DOI] [PubMed] [Google Scholar]
- 29.Cohn SM, Varela JE, Giannotti G, et al. Splanchnic perfusion evaluation during hemorrhage and resuscitation with gastric near-infrared spectroscopy. Journal of Trauma. 2001;50(4):629–635. doi: 10.1097/00005373-200104000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Beilman GJ, Groehler KE, Lazaron V, Ortner JP. Near-infrared spectroscopy measurement of regional tissue oxyhemoglobin saturation during hemorrhagic shock. Shock. 1999;12(3):196–200. doi: 10.1097/00024382-199909000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Crookes BA, Cohn SM, Burton EA, Nelson J, Proctor KG. Noninvasive muscle oxygenation to guide fluid resuscitation after traumatic shock. Surgery. 2004;135(6):662–670. doi: 10.1016/j.surg.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 32.Soller BR, Ryan KL, Rickards CA, et al. Oxygen saturation determined from deep muscle, not thenar tissue, is an early indicator of central hypovolemia in humans. Critical Care Medicine. 2008;36(1):176–182. doi: 10.1097/01.CCM.0000295586.83787.7E. [DOI] [PubMed] [Google Scholar]
- 33.Bartels SA, Bezemer R, de Vries FJW, et al. Multi-site and multi-depth near-infrared spectroscopy in a model of simulated (central) hypovolemia: lower body negative pressure. Intensive Care Medicine. 2011;37(4):671–677. doi: 10.1007/s00134-010-2128-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Soller BR, Yang Y, Soyemi OO, et al. Noninvasively determined muscle oxygen saturation is an early indicator of central hypovolemia in humans. Journal of Applied Physiology. 2008;104(2):475–481. doi: 10.1152/japplphysiol.00600.2007. [DOI] [PubMed] [Google Scholar]
- 35.Cohn SM, Pearl RG, Acosta SM, et al. A prospective randomized pilot study of near-infrared spectroscopy-directed restricted fluid therapy versus standard fluid therapy in patients undergoing elective colorectal surgery. American Surgeon. 2010;76(12):1384–1392. [PubMed] [Google Scholar]
- 36.Lobo DN, Bostock KA, Neal KR, Perkins AC, Rowlands BJ, Allison SP. Effect of salt and water balance on recovery of gastrointestinal function after elective colonic resection: a randomised controlled trial. The Lancet. 2002;359(9320):1812–1818. doi: 10.1016/S0140-6736(02)08711-1. [DOI] [PubMed] [Google Scholar]
- 37.Nisanevich V, Felsenstein I, Almogy G, Weissman C, Einav S, Matot I. Effect of intraoperative fluid management on outcome after intraabdominal surgery. Anesthesiology. 2005;103(1):25–32. doi: 10.1097/00000542-200507000-00008. [DOI] [PubMed] [Google Scholar]
- 38.McKinley BA, Marvin RG, Cocanour CS, Moore FA. Tissue hemoglobin O2 saturation during resuscitation of traumatic shock monitored using near infrared spectrometry. Journal of Trauma. 2000;48(4):637–642. doi: 10.1097/00005373-200004000-00009. [DOI] [PubMed] [Google Scholar]
- 39.Moore FA, Nelson T, McKinley BA, et al. Massive transfusion in trauma patients: tissue hemoglobin oxygen saturation predicts poor outcome. Journal of Trauma. 2008;64(4):1010–1023. doi: 10.1097/TA.0b013e31816a2417. [DOI] [PubMed] [Google Scholar]
- 40.Smith J, Bricker S, Putnam B. Tissue oxygen saturation predicts the need for early blood transfusion in trauma patients. American Surgeon. 2008;74(10):1006–1011. [PubMed] [Google Scholar]
- 41.Beekley AC, Martin MJ, Nelson T, et al. Continuous noninvasive tissue oximetry in the early evaluation of the combat casualty: a prospective study. Journal of Trauma. 2010;69(supplement 1):S14–S25. doi: 10.1097/TA.0b013e3181e42326. [DOI] [PubMed] [Google Scholar]
- 42.Ikossi DG, Knudson MM, Morabito DJ, et al. Continuous muscle tissue oxygenation in critically injured patients: a prospective observational study. Journal of Trauma. 2006;61(4):780–788. doi: 10.1097/01.ta.0000239500.71419.58. [DOI] [PubMed] [Google Scholar]
- 43.Cohn SM, Nathens AB, Moore FA, et al. Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock resuscitation. Journal of Trauma. 2007;62(1):44–54. doi: 10.1097/TA.0b013e31802eb817. [DOI] [PubMed] [Google Scholar]
- 44.Sagraves SG, Newell MA, Bard MR, et al. Tissue oxygenation monitoring in the field: a new EMS vital sign. Journal of Trauma. 2009;67(3):441–444. doi: 10.1097/TA.0b013e3181b88de7. [DOI] [PubMed] [Google Scholar]
- 45.Guyette FX, Gomez H, Suffoletto B, et al. Prehospital dynamic tissue oxygen saturation response predicts in-hospital lifesaving interventions in trauma patients. Journal of Trauma and Acute Care Surgery. 2012;72(4):930–935. doi: 10.1097/TA.0b013e31823d0677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gómez H, Torres A, Polanco P, et al. Use of non-invasive NIRS during a vascular occlusion test to assess dynamic tissue O2 saturation response. Intensive Care Medicine. 2008;34(9):1600–1607. doi: 10.1007/s00134-008-1145-1. [DOI] [PubMed] [Google Scholar]
- 47.Leone M, Blidi S, Antonini F, et al. Oxygen tissue saturation is lower in nonsurvivors than in survivors after early resuscitation of septic shock. Anesthesiology. 2009;111(2):366–371. doi: 10.1097/ALN.0b013e3181aae72d. [DOI] [PubMed] [Google Scholar]
- 48.Shapiro NI, Arnold R, Sherwin R, et al. The association of near-infrared spectroscopy-derived tissue oxygenation measurements with sepsis syndromes, organ dysfunction and mortality in emergency department patients with sepsis. Critical Care. 2011;15(5, article R223) doi: 10.1186/cc10463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ait-Oufella H, Joffre J, Boelle PY, et al. Knee area tissue oxygen saturation is predictive of 14-day mortality in septic shock. Intensive Care Medicine. 2012;38:976–983. doi: 10.1007/s00134-012-2555-7. [DOI] [PubMed] [Google Scholar]
- 50.de Blasi RA, Palmisani S, Alampi D, et al. Microvascular dysfunction and skeletal muscle oxygenation assessed by phase-modulation near-infrared spectroscopy in patients with septic shock. Intensive Care Medicine. 2005;31(12):1661–1668. doi: 10.1007/s00134-005-2822-y. [DOI] [PubMed] [Google Scholar]
- 51.Mesquida J, Gruartmoner G, Martínez ML, et al. Thenar oxygen saturation and invasive oxygen delivery measurements in critically ill patients in early septic shock. Shock. 2011;35(5):456–459. doi: 10.1097/SHK.0b013e3182094ab9. [DOI] [PubMed] [Google Scholar]
- 52.Mesquida J, Masip J, Gili G, Artigas A, Baigorri F. Thenar oxygen saturation measured by near infrared spectroscopy as a noninvasive predictor of low central venous oxygen saturation in septic patients. Intensive Care Medicine. 2009;35(6):1106–1109. doi: 10.1007/s00134-009-1410-y. [DOI] [PubMed] [Google Scholar]
- 53.Podbregar M, Možina H. Skeletal muscle oxygen saturation does not estimate mixed venous oxygen saturation in patients with severe left heart failure and additional severe sepsis or septic shock. Critical Care. 2007;11, article R6 doi: 10.1186/cc5153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mulier KE, Skarda DE, Taylor JH, et al. Near-infrared spectroscopy in patients with severe sepsis: correlation with invasive hemodynamic measurements. Surgical Infections. 2008;9(5):515–519. doi: 10.1089/sur.2007.091. [DOI] [PubMed] [Google Scholar]
- 55.Možina H, Podbregar M. Near-infrared spectroscopy during stagnant ischemia estimates central venous oxygen saturation and mixed venous oxygen saturation discrepancy in patients with severe left heart failure and additional sepsis/septic shock. Critical Care. 2010;14(2, article R42) doi: 10.1186/cc8929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nardi O, Polito A, Aboab J, et al. StO2 guided early resuscitation in subjects with severe sepsis or septic shock: a randomised trial. Journal of Clinical Monitoring and Computing. 2013;27(3):215–221. doi: 10.1007/s10877-013-9432-y. [DOI] [PubMed] [Google Scholar]
- 57.Gruartmoner G, Mesquida J, Masip J, et al. Thenar oxygen saturation (StO2) during weaning from mechanical ventilation: an observational study. doi: 10.1183/09031936.00126312. European Respiratory Journal. In press. [DOI] [PubMed] [Google Scholar]
- 58.Annane D. Thenar tissue oxygen saturation monitoring: noninvasive does not mean simple or accurate! Critical Care Medicine. 2011;39(7):1828–1829. doi: 10.1097/CCM.0b013e31821b8153. [DOI] [PubMed] [Google Scholar]
- 59.Lima A, van Genderen ME, Klijn E, Bakker J, van Bommel J. Peripheral vasoconstriction influences thenar oxygen saturation as measured by near-infrared spectroscopy. Intensive Care Medicine. 2012;38:606–611. doi: 10.1007/s00134-012-2486-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


