SUMMARY
OBJECTIVE
A substantial dropout from the first dose of diphtheria-tetanus-pertussis (DTP1) to the 3rd dose of DTP (DTP3) immunization has been recorded in Pakistan. We conducted a randomized controlled trial to assess the effects of providing substantially redesigned immunization card, center-based education, or both interventions together on DTP3 completion at six rural Expanded Programme on Immunization (EPI) centers in Pakistan.
METHODS
Mother-child units were enrolled at DTP1 and randomized to four study groups: redesigned card, center-based education, combined intervention, and standard care. Each child was followed-up for 90 days to record the dates of DTP2 and DTP3 visits. The study outcome was DTP3 completion by the end of follow-up period in each study group.
RESULTS
We enrolled 378 mother-child units in redesigned card group, 376 in center-based education group, 374 in combined intervention group, and 378 in standard care group. By the end of follow-up, 39% of children in standard care group completed DTP3. Compared to this, a significantly higher proportion of children completed DTP3 in redesigned card group (66%) (crude Risk Ratio [RR] = 1.7; 95% CI = 1.5, 2.0), center-based education group (61%) (RR = 1.5; 95% CI = 1.3, 1.8), and combined intervention group (67%) (RR = 1.7; 95% CI = 1.4, 2.0).
CONCLUSIONS
Improved immunization card alone, education to mothers alone, or both together were all effective in increasing follow-up immunization visits. The study underscores the potential of study interventions’ public health impact and necessitates their evaluation for complete EPI schedule at a large scale in the EPI system.
Introduction
The Expanded Programme on Immunization (EPI) offers a series of vaccines to children in Pakistan and many other World Health Organization (WHO) member states. These include Bacillus Calmette-Guérin (BCG) and oral polio vaccine (OPV) at birth, three doses of diphtheria-tetanus-pertussis (DTP)/OPV/hepatitis B virus (HBV) vaccines at 6, 10, and 14 weeks, and measles vaccine at 9 and 15 months after birth (WHO 2006). A countrywide network of EPI in Pakistan offers these vaccines to children at immunization centers at no cost; supplemented with outreach programs in some areas.
A principal indicator of immunization coverage levels by the WHO is the completion of three doses of DTP vaccine (DTP3). With some contribution from outreach programs, nationwide DTP3 coverage is primarily a function of the proportion of newborns that an immunization system brings in for the first immunization and the proportion of these children who return to the EPI centers for subsequent visits to complete DTP3. From 2002 to 2005, the WHO reported DTP3 coverage in Pakistan was 65%–72%. Socio-economically comparable countries in South-East Asia Region of the WHO have consistently achieved higher DTP3 levels than has Pakistan (WHO 2006). The BCG coverage (80%–82% during 2002–2005) in Pakistan suggests that a high proportion of newborns receive EPI services, but a substantial proportion of these children fail to return for subsequent immunization visits. Despite progress in last two decades, it is unclear whether the measures currently in place in Pakistan will be sufficient to reach the desired national DTP3 coverage of more than 80%.
In 2003–2004, we designed a reminder type immunization card and developed a center-based information and motivation session for mothers/caregivers (henceforth referred to as “mothers”) for a randomized controlled trial to assess the effectiveness of providing these interventions on DTP3 completion at urban EPI centers in Pakistan (Usman et al. 2009). In the urban trial we recorded 36% increase in DTP3 completion among children who received both redesigned card and center-based education to mothers and 26% increase among children who received redesigned card only, compared with standard care group. Encouraged from the results of the urban study and considering urban rural disparities in literacy rate and socio-ethnic distribution in Pakistan, we conducted a second randomized controlled trial in 2005–2006 to test the effectiveness of same interventions at rural EPI centers in Pakistan.
Methods
Setting
The trial was conducted at six EPI centers located in the rural peripheries of Karachi, the capital city of Sindh Province. Study centers were selected from all rural centers around Karachi based on the highest volume of children vaccinated for DTP1 immunizations in previous year.
Eligibility and Enrollment
All children visiting the selected EPI centers for DTP1 were eligible to participate in the study, provided that the mother had been living in the area for last six months or more. This criterion was used to exclude two groups of temporary residents. First, women relocated to mothers’ house for a few weeks to deliver their children and second, internally displaced families that had migrated to the study area to avoid the aftermath of 2005 earthquake in the north of Pakistan.
Given low literacy rates among women in rural Pakistan, a trained interviewer read out the consent form to the mother of each eligible child. For consenting mothers, the form was signed by the interviewer and a witness for enrollment. We used a pre-coded questionnaire at enrollment to record information from mothers on socio-demographic variables and factors potentially associated with immunization completion. The questionnaire addressed parents’ attributes (age at enrollment, education, occupation, monthly household income, ethnicity, family size, and mother’s age at marriage and first conception); child’s attributes (age at enrollment, sex, and number of siblings); dates of DTP1-3 immunizations; and mode of transport and travel time to reach the EPI center.
Randomization
The lead investigator provided a computer generated randomization list to each enrollment center. Each enrolled mother-child pair received an identification number (ID) from the randomization list and was assigned to the study group corresponding to the ID on the list. Because of the overt nature of interventions, neither the study participants nor the interviewers enrolling the study participants and recording the study outcome were blinded to the type of intervention received by the study participants.
Interventions
Redesigned card
The EPI card currently used in Pakistan has two main shortcomings. First, it is small (9 cm × 8.5 cm, when folded), hence the information on child’s identity, immunization schedule, information for mothers, and next immunization visit dates is crowded together and appears disorderly. Second, the next immunization date is hand written by the EPI staff, often in very small and irregular letters. As a result, less literate mothers have difficulties reading the date of their child’s next immunization. To address these issues, we designed a new simpler immunization card whose most important intended functions were to act as a constant reminder to mothers of the next immunization visit, and to make it easy for them to locate and read the date of the next immunization. Much larger than the existing EPI card (15.5cm × 11.5 cm when folded), the redesigned card was bright yellow in color, placed in a plastic jacket, and provided with a hanging string. On its outer sides, the card showed nothing but the next immunization date and day of the week for DTP2 and DTP3 visits written in a large font (Times New Roman 42, Microsoft Word®) using preprinted stickers. Dedicated boxes were included on the inner sides of the folded card to record the remainder of the information (name of the EPI center, card number, card’s date of issue, child’s name and address, complete immunization schedule dates, and instructions to the mothers). Despite a small purchase volume, the cost of each card including the plastic jacket was US$ 0.05 (Pakistani Rupees 3).
Center-based education
In Pakistan there is currently no standardized procedure describing how the EPI staff should inform mothers about subsequent immunization visits. Because mother’s lack of information might contribute to childhood immunization dropouts, the second intervention (center-based education) was designed as a 2–3 minutes conversation with mother to convey the importance of the completion of immunization schedule and to explain the potential adverse impact of incomplete immunization on child’s health. The session was in simple vocabulary in the local language (Urdu) and deliberately kept short in prevision of potential large-scale use by EPI staff in the future.
Trial Design
Mother-child pairs were randomly allocated to three intervention and one standard care groups. Interventions were provided in a private space to prevent contamination between study groups.
At enrollment in the first intervention group (“Redesigned card”), a trained interviewer pasted the upcoming date and day of DTP2 immunization on both outer sides of the card and showed it to the mother. Mother was asked to hang the card in her home at a frequently visible place and requested that she bring the card along on her next immunization visit to the EPI center. At DPT2 visit, the interviewer crossed out the date and day for DTP2 visit to avoid any confusion to the mothers; pasted the date and day for the upcoming DTP3 immunization visit on both sides of the card: and showed the information to the mother. Mothers in the second intervention group (“Center-based education”) received center-based education from trained study interviewers. Mothers in the third intervention group (“Combined intervention”) received both the redesigned card and center-based education in exactly the same way as described above. Finally, mothers of the fourth group (“Standard care”) underwent routine EPI center visit and received neither intervention.
Follow-up
We followed-up each study child at the EPI center for 90 days from the day of enrollment at DTP1. Because each DTP2 and DTP3 were scheduled at 30-days intervals after DTP1 by EPI schedule, both DTP2 and DTP3 could be completed ideally within 60 days after the DTP1 visit. During the study period, interviewers screened every child who visited their study centers and recorded DPT2 and DPT3 dates of study children.
Study outcome
The study outcome was the immunization status of each child at the end of day 90 post enrollment. The immunization status was dichotomized into completion of both DTP2 and DTP3 (termed “DTP3 completed”) and all others (termed “DTP3 not completed”).
Statistical methods
Sample size was calculated for the comparison of two proportions. Assuming DTP3 completion of 75% in the standard care group, we calculated that a sample size of 375 subjects in each study group would be sufficient to detect ≥ 10% higher DTP3 completion in any one of the intervention groups than in the standard care group with 90% power and 5% unadjusted type-1 error.
All analyses were performed using SAS® version 9.1 (SAS Institute, Inc., Cary, NC, USA) and were by intention to treat. To determine how successful the randomization process had been, we compared frequencies and percentages of participants’ baseline characteristics across study groups. The main independent variable was the type of intervention with the four study group categories. The immunization status coded ‘1’ for “DTP3 completed” and ‘0’ for “DTP3 not completed” was the dependent variable. In primary analysis, we computed crude risk ratios (RRs) and their 95% confidence intervals (CIs) by univariate log-binomial regression (SAS® PROC GENMOD) to assess the effect of each intervention on DTP3 completion (Wacholder 1986; Zocchetti et al. 1995; Skov et al. 1998; Spiegelman & Hertzmark 2005).
Because of important socioeconomic, literacy, and cultural differences between Mohajir and non-Mohajir ethnicities, we evaluated the evidence of effect-measure modification by ethnicity on the effectiveness of interventions. The hypothesis for secondary analysis was conceived during the data analysis phase of the study. For this secondary analysis, we used log-binomial regression to compute crude and adjusted risk ratios separately among Mohajir and non-Mohajir ethnicities (Wacholder 1986; Zocchetti et al. 1995; Skov et al. 1998; Spiegelman & Hertzmark 2005). Because multivariable model constructed among Mohajirs failed to converge, the final model was reconstructed using multivariable Poisson regression with robust variance (Zou 2004; Spiegelman & Hertzmark 2005).
Approval for this study was obtained from the Ethical Review Committee (ERC) of the Aga Khan University (AKU), Karachi, Pakistan and the Institutional Review Board (IRB) of the University of Alabama at Birmingham (UAB).
Results
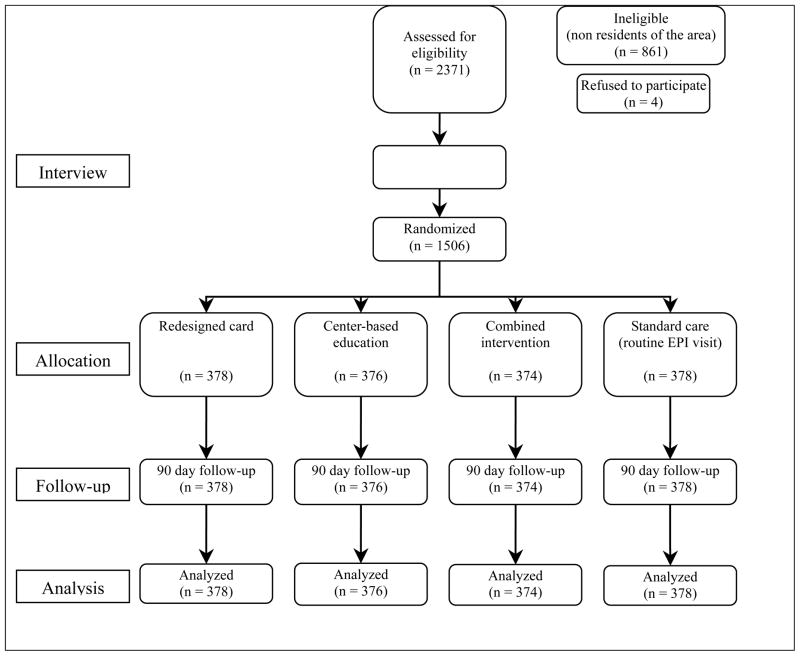
Of 2,371 mother-child pairs screened for eligibility between November 2005 and May 2006, 861 (36%) were excluded because they had arrived in the area within the past six months and four (0.2%) because they refused to participate (Figure 1). Enrollment was concluded after random allocation of 1506 study participants to four study groups. The follow-up of the last study child enrolled in the study was completed in August, 2006. Since the study participants who had not returned to the centers within 90 days of their DPT1 visit were considered DTP3 not completed, no study participant was considered lost to follow-up. In multivariable analysis, we excluded 15 children from the redesigned card group, 11 from the center-based education group, 7 from the combined intervention group, and 12 from the standard care group because of missing child’s age at enrollment.
Figure 1.
Flow of study participants
The majority of informants in all study groups (77%–81%) were mothers; most of the other interviewees were other female caretakers, including grandmothers and aunts. The distribution of participants’ socio-demographic characteristics at enrollment was similar (p > 0.05) across study groups except for maternal age (p = 0.03; Table 1).
Table 1.
Distribution of socio-demographic characteristics of study participants at enrollment among study groups (Pakistan, 2005–2006)
| Variables | Redesigned card | Center-based education | Combined intervention | Standard care |
|---|---|---|---|---|
|
| ||||
| n = 378 | n = 376 | n = 378 | n = 376 | |
|
| ||||
| Column % | Column % | Column % | Column % | |
| EPI center of enrollment | ||||
| A | 25 | 25 | 25 | 25 |
| B | 17 | 20 | 18 | 19 |
| C | 7 | 6 | 5 | 5 |
| D | 28 | 28 | 33 | 30 |
| E | 6 | 5 | 3 | 4 |
| F | 17 | 16 | 17 | 17 |
| Mother of child as respondent | 77 | 81 | 79 | 80 |
| Ethnicity | ||||
| Mohajir | 15 | 14 | 13 | 16 |
| Pashto | 33 | 31 | 33 | 32 |
| Punjabi | 13 | 16 | 14 | 11 |
| Hindko | 19 | 19 | 20 | 18 |
| Sindhi | 9 | 9 | 11 | 13 |
| Others | 11 | 12 | 9 | 11 |
| Child’s age at enrollment (days) | ||||
| ≤ 60 | 58 | 57 | 64 | 57 |
| > 60 | 38 | 40 | 34 | 40 |
| Missing | 4 | 3 | 2 | 3 |
| Boys enrolled | 51 | 49 | 53 | 49 |
| Total number of living children in the family | ||||
| One | 28 | 22 | 24 | 28 |
| Two | 25 | 20 | 27 | 21 |
| Three or more | 47 | 57 | 49 | 51 |
| Mother’s age at enrollment (years) | ||||
| ≤ 19 | 10 | 6 | 9 | 8 |
| 20 – 29 | 70 | 64 | 64 | 68 |
| > 29 | 20 | 30 | 27 | 24 |
| Mother’s years of formal schooling | ||||
| ≥ 6 | 26 | 27 | 26 | 26 |
| 1 – 5 | 18 | 17 | 19 | 17 |
| 0 | 56 | 57 | 55 | 57 |
| Mother a housewife | 96 | 99 | 98 | 98 |
| Father’s years of formal schooling | ||||
| ≥ 6 | 53 | 49 | 56 | 54 |
| 1 – 5 | 15 | 17 | 11 | 13 |
| 0 | 32 | 35 | 32 | 33 |
| ≤ 5 household members | 28 | 27 | 23 | 23 |
| Monthly household income | ||||
| 0 – 5000 | 64 | 55 | 62 | 60 |
| > 5000 | 36 | 45 | 38 | 40 |
| Television in home | 57 | 53 | 56 | 54 |
| Mode of transport to EPI center | ||||
| Public bus system | 5 | 9 | 6 | 6 |
| Privately owned or rented motor | 10 | 8 | 6 | 7 |
| On foot | 85 | 84 | 88 | 87 |
| ≥ 5 minutes to reach EPI center from home | 20 | 22 | 19 | 17 |
By the end of follow-up, 39% of children in the standard care group completed DTP3 (Table 2). Compared to this, a significantly higher proportion of children completed DTP3 in the redesigned card group (66%) (crude Risk Ratio [RR] = 1.7; 95% CI = 1.5, 2.0), the center-based education group (61%) (RR = 1.5; 95% CI = 1.3, 1.8), and the combined intervention group (67%) (RR = 1.7; 95% CI = 1.4, 2.0).
Table 2.
Crude Risk Ratios (RRs) and 95% Confidence Intervals (CIs) for DTP3 completion by intervention group (Pakistan, 2005–2006)
| Study groups | Total | DTP3 completed during 90 days follow-up
|
Crude RR* | 95% CI** | |
|---|---|---|---|---|---|
| n | (%) | ||||
| Redesigned card | 378 | 252 | (67) | 1.7 | (1.5, 2.0) |
| Center-based education | 376 | 228 | (61) | 1.5 | (1.3, 1.8) |
| Combined intervention | 374 | 245 | (66) | 1.7 | (1.4, 2.0) |
| Standard care | 378 | 149 | (39) | 1.0† | |
RR = Risk Ratio
CI = Confidence Interval
A risk ratio of 1.0 indicates the reference category
In secondary analysis, after adjusting for child’s age at enrollment and mother’s formal years of schooling, a significantly higher proportion of Mohajir children completed DTP3 in the redesigned card group (Adjusted Risk Ratio [Adj. RR] = 3.0; 95% CI = 1.7, 5.3), the center-based education group (Adj. RR = 3.3; 95% CI = 1.9, 5.8), and the combined intervention group (Adj. RR = 3.0; 95% CI = 1.7, 5.4) compared with the standard care group (Table 3). Although interventions were also effective among non-Mohajir children, the individual or combined effects of interventions on DTP3 completion were much weaker than among Mohajir children.
Table 3.
Crude and adjusted Risk Ratios (RRs) with 95% Confidence Intervals (CIs) for DTP3 completion by intervention group among Mohajirs and non-Mohajirs children (Pakistan, 2005–2006)
| Study groups | Total | DTP3 completed during 90 days follow-up
|
Crude RR* | 95% CI** | Adjusted RR* | 95% CI** | |||
|---|---|---|---|---|---|---|---|---|---|
| n | (%) | ||||||||
| Mohajir | Redesigned card | 56 | 46 | (82) | 3.0 | (2.0, 4.7) | 3.0 | (1.7, 5.3) | |
| Center-based education | 51 | 46 | (90) | 3.3 | (2.2, 5.1) | 3.3 | (1.9, 5.8) | ||
| Combined intervention | 49 | 40 | (82) | 3.0 | (1.9, 4.7) | 3.0 | (1.7, 5.4) | ||
| Standard care | 59 | 16 | (27) | 1.0† | 1.0† | ||||
|
| |||||||||
| Non-Mohajir | Redesigned card | 322 | 206 | (64) | 1.5 | (1.3, 1.8) | 1.5 | (1.3, 1.8) | |
| Center-based education | 325 | 182 | (56) | 1.3 | (1.1, 1.6) | 1.3 | (1.1, 1.6) | ||
| Combined intervention | 325 | 205 | (63) | 1.5 | (1.3, 1.8) | 1.5 | (1.3, 1.7) | ||
| Standard care | 319 | 133 | (42) | 1.0† | 1.0† | ||||
Multivariable model adjusted for child’s age at enrollment and mother’s years of formal schooling. Child’s age at enrollment was not available for one child each in Group 1, Group 2, and Group 3 among Mohajirs and 14 children in Group 1, 10 in Group 2, 6 in Group 3, and 12 in Group 4 among non-Mohajirs.
RR = Risk Ratio
CI = Confidence Interval
A risk ratio of 1.0 indicates the reference category
Note: All pairwise comparisons: p<0.01
Discussion
This study suggests that providing an inexpensive reminder type immunization card or a short center-based education to mothers are both effective interventions for increasing subsequent immunization visits to the EPI centers. We found no evidence that providing both interventions in combination was superior to providing the redesigned immunization card alone.
Compared to our urban trial (Usman et al. 2009), study interventions were more effective at rural EPI centers and resulted in higher percentage increase in DTP3 completion in all three intervention groups. In a resource constraint setting such as Pakistan, policy makers may prefer implementing the proposed interventions first in rural areas. However, the implementation of these interventions at a large scale may be more cost-effective in urban areas due to lower administrative and training costs for comparatively high volume and geographically closer urban EPI centers.
In both urban and rural trials, providing redesigned card alone was more effective than education alone in increasing DTP3 completion. Further, combining two interventions at urban centers resulted in even higher DTP3 completion. However at rural centers, combined effect of two interventions was not higher than the effect of redesigned card alone. This may indicate that a structural intervention such as the redesigned immunization card is best suited for lower literacy rural areas and can achieve the maximum benefit even if implemented without the center-based education to mothers.
In developing countries, successful supply-side interventions have used different approaches to improve staff performance such as enhanced monitoring and supervision (van Zwanenberg & Hull 1988), training in a classroom (Main et al. 2001), or training by peers in the field (Robinson et al. 2001), Other effective supply-side approaches focused on increasing access to immunization by making modifications to the vaccination schedule (e.g., delivering vaccines earlier or at shorter intervals) (Chen 1976; Chen 1989; Maher et al. 1993), reorganizing clinic procedures to shorten waiting times (Ekunwe 1984), and bringing immunization services closer to the people using outreach teams (Dominguez Uga 1988; Coetzee et al. 1993; San Sebastian et al. 2001), or community health workers (Alto et al. 1989).
Interventions that have proved effective in stimulating the demand in resource poor settings for vaccination among children with incomplete immunization include reminders sent to the home of target children (Kuhn & Zwarenstein 1990) and door-to-door household visits to notify parents that their child is late for a vaccine (Cutts et al. 1990; Brugha & Kevany 1996). Redesigning the immunization card for reducing immunization dropouts has not received attention in developing countries. Articles, reviewing published studies (Pegurri et al. 2005) and the grey literature (Batt et al. 2004), on strategies to improve childhood immunization coverage in low and middle-income countries could not identify any study attempting to redesign the immunization card and evaluating its impact on immunization visits. Interventions assessed in our published urban trial (Usman et al. 2009) and this rural trial attempted to increase demand by targeting children who are already in the EPI system. We believe that these studies are a major step forward in demonstrating potential large scale impact of proposed interventions to the policy makers.
The redesigned immunization card tested in this study has several characteristics that make it an appealing and viable option to improve the vaccine delivery system in rural Pakistan. Because the new card was designed considering the sparse level of EPI staffing and the additional cost incurred to the EPI system, we believe that the large scale implementation of the new card in the EPI system would not require any additional work from EPI staff and only minimally add to the cost per child immunized. Based on our study estimates of DTP3 completion among the redesigned card and standard care groups (Table 2), a country wide implementation of the redesigned card in rural areas could potentially translate into more than half a million additional children immunized for DTP3 in an annual rural Pakistani birth cohort of 2.8 million children (Pakistan 2001). Another spinoff benefit of using the redesigned card in the EPI system could be that mothers may retain the new card for a longer period due to its plastic jacket and larger size; resulting in more accurate estimation of immunization coverage by cross-sectional surveys. At present, these surveys rely heavily on mother’s recall as the existing EPI card is usually not available with the majority of mothers at the time of interview (Mukanga & Kiguli 2006; Torun & Bakirci 2006).
In secondary analysis, we observed that the effects of redesigned card and center based education on DTP3 completion were substantially stronger among Mohajir than non-Mohajir ethnicities (Table 3). The underlying reason for this effect-measure modification by ethnicity is unclear. We explored if higher years of schooling among Mohajir mothers might have played a role in responding more positively to the interventions. However, adjusting for mother’s years of formal schooling did not affect the differences in the effect of interventions between the two ethnic groups. Future studies should further explore this differential responsiveness of ethnic groups to such interventions.
A limitation of our study is that the follow-up of study children for return visits was carried out only at the study centers for a limited period of 90 days. There is a chance that a small proportion of children might have returned to the study centers after the follow up period or visited non-study EPI centers for DTP2 or DTP3. Nonetheless, we don’t have any evidence suggesting higher occurrence of this in standard care group given the randomized design of our study, and assume that it did not affect the internal validity of the study. Additionally, survival curves of days to DTP3 for each study group (data not shown) indicated a plateau at around 80 days of follow-up making it unlikely that a large number of children might have returned for DTP3 after 90 days.
The WHO reported coverage of 82% for DTP1 and 72% for DTP3 in Pakistan for 2005. This suggests that 88% (72/82*100) of children who received DTP1 went on to complete DTP3; in contrast, no more than 39% of the children enrolled in the standard care group of our study completed DTP3 in 90 days follow-up (Table 2). Comparison of these figures must be done with caution because our study estimates came from a cohort of children followed-up at EPI centers whereas the WHO estimates were calculated using DTP1 and DTP3 coverage. Additionally, dropouts in the rural areas where our study was conducted are also likely to be higher than the country level estimates reported by the WHO because of lower socio-economic conditions in rural areas of Pakistan. Nonetheless, the reasons discussed above might not fully explain the wide gap between the study and the WHO estimates and the possibility of WHO overestimating childhood immunization in Pakistan cannot be ruled out (Murray et al. 2003).
Due to limited time and resource, we tested the effect of study interventions only on two follow-up immunization visits (DTP2 and DTP3) scheduled after DTP1. Because complete EPI schedule in Pakistan has five follow-up visits (DTP1, DTP2, DTP3, measles 1, and measles 2) after BCG at birth, it is difficult to predict the effectiveness of proposed interventions for the complete EPI schedule. Furthermore, low immunization coverage cannot be effectively addressed solely by reducing the dropouts; interventions to bring more newborns in the EPI system are equally important.
In conclusion, this study offers strong evidence that redesigned immunization card was effective in enhancing subsequent infant vaccine visits. Because this low-cost intervention has the potential to yield considerable benefits for children, the next step will be to evaluate them for complete EPI schedule at a large scale in the EPI system.
Acknowledgments
This study was funded by the Sparkman Center for Global Health and NIH grant D43TW005497, the University of Alabama at Birmingham-Aga Khan University International Maternal and Child Health Research and Training (IMCHRT) program. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. We thank the EPI Sindh, Pakistan for granting permission and extending cooperation for this study.
Footnotes
Conflict of interest statement: None declared.
References
- Ekunwe EO. Expanding immunization coverage through improved clinic procedures. World Health Forum. 1984;5(4):361–3. [Google Scholar]
- [Accessed February 6, 2008];Pakistan demographic survey. 2001 Available at: http://www.statpak.gov.pk/depts/fbs/statistics/pds2001/pds2001.html.
- Alto WA, Alk S, Pinau D, Polume H. Improving immunization coverage, a comparison between traditional MCH teams and MCH teams plus aid post orderlies. P N G Med J. 1989;32:97–100. [PubMed] [Google Scholar]
- Batt K, Fox-Rushby JA, Castillo-Riquelme M. The costs, effects and cost-effectiveness of strategies to increase coverage of routine immunizations in low- and middle-income countries: systematic review of the grey literature. Bull World Health Organ. 2004;82:689–696. [PMC free article] [PubMed] [Google Scholar]
- Brugha RF, Kevany JP. Maximizing immunization coverage through home visits: a controlled trial in an urban area of Ghana. Bull World Health Organ. 1996;74:517–524. [PMC free article] [PubMed] [Google Scholar]
- Chen ST. The improvement of immunization coverage by early immunisation of children in Malaysia. Med J Malaysia. 1976;31:17–19. [PubMed] [Google Scholar]
- Chen ST. Influence of immunization schedule on immunization coverage. J Trop Med Hyg. 1989;92:386–390. [PubMed] [Google Scholar]
- Coetzee DJ, Ferrinho P, Reinach SG. A vaccination survey using the EPI methodology to evaluate the impact of a child health outreach programme in an urban area of South Africa. Bull World Health Organ. 1993;71:33–39. [PMC free article] [PubMed] [Google Scholar]
- Cutts FT, Phillips M, Kortbeek S, Soares A. Door-to-door canvassing for immunization program acceleration in Mozambique: achievements and costs. Int J Health Serv. 1990;20:717–725. doi: 10.2190/61V1-220G-4A4D-K8KN. [DOI] [PubMed] [Google Scholar]
- Dominguez Uga MA. Economic analysis of the vaccination strategies adopted in Brazil in 1982. Bull Pan Am Health Organ. 1988;22:250–268. [PubMed] [Google Scholar]
- Kuhn L, Zwarenstein M. Evaluation of a village health worker programme: the use of village health worker retained records. Int J Epidemiol. 1990;19:685–692. doi: 10.1093/ije/19.3.685. [DOI] [PubMed] [Google Scholar]
- Maher CP, Hall JJ, Yakam W, Naupa M, Leonard D. Improving vaccination coverage: the experience of the Expanded Programme on Immunization in Vanuatu. P N G Med J. 1993;36:228–233. [PubMed] [Google Scholar]
- Main B, Lower T, James R, Rouse I. Changes in Expanded Program for Immunization coverage for mother and child in Krakor, Cambodia 1996–1998. Trop Med Int Health. 2001;6:526–528. doi: 10.1046/j.1365-3156.2001.00743.x. [DOI] [PubMed] [Google Scholar]
- Mukanga DO, Kiguli S. Factors affecting the retention and use of child health cards in a slum community in Kampala, Uganda, 2005. Matern Child Health J. 2006;10:545–552. doi: 10.1007/s10995-006-0132-9. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Shengelia B, Gupta N, Moussavi S, Tandon A, Thieren M. Validity of reported vaccination coverage in 45 countries. Lancet. 2003;27:1022–7. doi: 10.1016/S0140-6736(03)14411-X. [DOI] [PubMed] [Google Scholar]
- Pegurri E, Fox-Rushby JA, Damian W. The effects and costs of expanding the coverage of immunisation services in developing countries: a systematic literature review. Vaccine. 2005;23:1624–1635. doi: 10.1016/j.vaccine.2004.02.029. [DOI] [PubMed] [Google Scholar]
- Robinson JS, Burkhalter BR, Rasmussen B, Sugiono R. Low-cost on-the-job peer training of nurses improved immunization coverage in Indonesia. Bull World Health Organ. 2001;79:150–158. [PMC free article] [PubMed] [Google Scholar]
- San Sebastian M, Goicolea I, Aviles J, Narvaez M. Improving immunization coverage in rural areas of Ecuador: a cost-effectiveness analysis. Trop Doct. 2001;31:21–24. doi: 10.1177/004947550103100107. [DOI] [PubMed] [Google Scholar]
- Skov T, Deddens J, Petersen MR, Endahl L. Prevalence proportion ratios: estimation and hypothesis testing. Int J Epidemiol. 1998;27:91–95. doi: 10.1093/ije/27.1.91. [DOI] [PubMed] [Google Scholar]
- Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- Torun SD, Bakirci N. Vaccination coverage and reasons for non-vaccination in a district of Istanbul. BMC Public Health. 2006;6:125. doi: 10.1186/1471-2458-6-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usman HR, Akhtar S, Habib F, Jehan I. Redesigned immunization card and center-based education to reduce childhood immunization dropouts in urban Pakistan: a randomized controlled trial. Vaccine. 2009;27:467–472. doi: 10.1016/j.vaccine.2008.10.048. [DOI] [PubMed] [Google Scholar]
- van Zwanenberg TD, Hull C. Improving immunisation: coverage in a province in Papua New Guinea. Br Med J (Clin Res Ed) 1988;296:1654–1656. doi: 10.1136/bmj.296.6637.1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacholder S. Binomial regression in GLIM: estimating risk ratios and risk differences. Am J Epidemiol. 1986;123:174–184. doi: 10.1093/oxfordjournals.aje.a114212. [DOI] [PubMed] [Google Scholar]
- WHO. 2006 Global Summary. Geneva: 2006. Vaccines and Biologicals: WHO Vaccine Preventable Diseases: Monitoring System. [Google Scholar]
- Zocchetti C, Consonni D, Bertazzi PA. Estimation of prevalence rate ratios from cross-sectional data. Int J Epidemiol. 1995;24:1064–1067. doi: 10.1093/ije/24.5.1064. [DOI] [PubMed] [Google Scholar]
- Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]