Abstract
Background
Current research on nonconscious stereotyping in health care is limited by an emphasis on practicing physicians’ beliefs about African American patients and by heavy reliance on a measure of nonconscious processes that allows participants to exert control over their behavior if they are motivated to appear nonbiased.
Objectives
The present research examined whether nursing and medical students exhibit nonconscious activation of stereotypes about Hispanic patients using a task that subliminally primes patient ethnicity. It was hypothesized that participants would exhibit greater activation of noncompliance and health risk stereotypes following subliminal exposure to Hispanic faces compared with non-Hispanic White faces and, because ethnicity was primed outside of conscious awareness, that explicit motivations to control prejudice would not moderate stereotype activation.
Methods
Nursing and medical students completed a sequential priming task that measured the speed with which they recognized words related to noncompliance and health risk following subliminal exposure to Hispanic and non-Hispanic White faces. They then completed explicit measures of their motivation to control prejudice against Hispanics.
Results
Both nursing and medical students exhibited greater activation of noncompliance and health risk words after subliminal exposure to Hispanic faces, compared with non-Hispanic White faces. Explicit motivations to control prejudice did not moderate stereotype activation.
Discussion
These findings show that, regardless of their motivation to treat Hispanics fairly, nursing and medical students exhibit nonconscious activation of negative stereotypes when they encounter Hispanics. Implications are discussed.
Keywords: Nonconscious processes, stereotyping, Hispanic Americans, health care disparities, minority health, Implicit Associations Test, prejudice
Hispanic Americans face disparities in the diagnosis, treatment, survival, and prevention of disease (Gordon, Street, Sharf, & Souchek, 2006; Johnson, Saha, Arbelaez, Beach, & Cooper, 2004). Hispanics have a higher prevalence of obesity than non-Hispanic Whites, and they are more likely to die from diabetes and colorectal cancer (Agency for Healthcare Research and Quality [AHRQ], 2010). Hispanic Americans’ poor health outcomes are, in part, due to the disparate care they receive from health care providers. Indeed, Hispanic patients are less likely than non-Hispanic White patients to receive advice critical to long-term health outcomes, like obesity counseling, information on smoking cessation, and recommendations for annual cancer screening (AHRQ, 2010; Lopez-Quintero, Crum, & Neumark, 2006; Mead et al., 2008). Addressing poor health outcomes among Hispanic Americans necessitates an understanding of the psychological processes that are at the heart of differential treatment.
The present research examines one form of intergroup bias that may contribute to the inferior care that Hispanic Americans receive: implicit stereotyping. Specifically, we examine whether nursing and medical students exhibit nonconscious mental activation of negative stereotypes associating Hispanics with noncompliance and risky health behaviors.
Stereotypes are beliefs associated with members of a given social group that become activated, or available in working memory, when perceivers encounter, and subsequently categorize, a member of the group (see Fiske, 1998 for review). Stereotypes can come to mind explicitly (consciously) or implicitly (nonconsciously) when a group member is encountered (Devine & Monteith, 1999). When stereotypes are explicit, perceivers are consciously aware of the stereotype, and they can deliberately decide whether to apply the stereotype to an individual group member. When a stereotype is implicit, on the other hand, it is available in working memory while remaining outside of conscious awareness, and it can guide how perceivers initially attend to and evaluate an individual group member without realizing they are using the stereotype (Sekaquaptewa, Espinoza, Thompson, Vergas, & von Hippel, 2003).
Research on racial health disparities suggests that medical personnel hold nonconscious negative stereotypes about minority patients (Cooper et al., 2012; Green et al., 2007; Sabin & Greenwald, 2012; Sheeran, Gollwitzer, & Bargh, 2012). However, most published research focuses on stereotypes about African Americans among practicing physicians. Little research has examined whether other minority patient groups, like Hispanics, are also nonconsciously stereotyped, or if nursing and medical students, who are in the early stages of learning about cultural competence, exhibit nonconscious stereotype activation. Given that both nursing and medical students are consciously aware of stereotypes within the health care community associating Hispanics with noncompliance and risky health behaviors (Bean, Focella, Stone, Moskowitz, & Badger, under review; Gregory, Wells, & Leake, 1987), it is important to examine if they also exhibit nonconscious activation of these stereotypes when they see a Hispanic face.
Understanding nonconscious stereotyping by health care personnel is also limited by heavy reliance on one computer-based reaction-time measure of stereotype activation: the Implicit Association Test (IAT).The IAT methodology is based on the assumption that if individuals hold a negative stereotype about a group, they will more quickly pair images of the group (e.g., African-American faces) with negative words related to the stereotype (e.g., “lazy”), compared with how quickly they pair the images with positive words. However, because the IAT requires participants to pair the images and words together, participants are consciously aware that the task is measuring their beliefs about the group. Consequently, participants who do not want to appear prejudiced can control their behavior on the task in an effort to respond in an unbiased manner (Conrey, Sherman, Gawronski, Hugenberg, & Groom, 2005; Fiedler & Bluemke, 2005).
The present study addresses these concerns by using a sequential priming task to present information about ethnicity subliminally, or outside of conscious awareness (Bargh & Chartrand, 2000). During the task, faces are flashed so quickly that participants are unable to consciously identify the images. The brain can still perceive the person’s ethnicity, however, which “primes,” or brings to mind, the associated ethnic group and its corresponding stereotypes. After a face is flashed, participants are asked to identify whether a letter string comprises a word in the English language. Similar to the IAT approach, studies show that, when subliminally primed for race, participants recognize words related to stereotypes about the target group more quickly than words unrelated to the stereotypes (Kawakami & Dovidio, 2001; Moskowitz, Stone, & Childs, 2012; Wittenbrink, Judd, & Park, 1997). Importantly, because information about the group is primed subliminally, participants are not aware that ethnicity is a central component of the task and, therefore, they do not become motivated to appear nonprejudiced.
In the present study, nursing and medical students were subliminally exposed to Hispanic and non-Hispanic White faces before identifying words related to noncompliance, health risk, negative stereotypes about Hispanics that are unrelated to health (e.g., uneducated; Dick, 2011; Dixon & Rosenbaum, 2004), and equally negative control words unrelated to stereotypes about Hispanics. It was hypothesized that participants would be faster to recognize noncompliance, health risk, and general stereotype words following exposure to Hispanic faces, compared with non-Hispanic Whitefaces. It was also predicted that, after Hispanic faces, participants would be faster to recognize stereotype-relevant words compared with negative control words, suggesting that specific stereotypes, rather than general negativity, are nonconsciously activated upon exposure to Hispanics. Because ethnicity was primed subliminally, we predicted that explicit motivation to control prejudice would not moderate facilitation of the stereotype-relevant words. Finally, because both nursing and medical students are explicitly aware of stereotypes associating Hispanic patients with noncompliance and risky health behavior (Bean et al., under review), participants’ program affiliation was not expected to moderate stereotype activation.
Methods
Participants and Recruitment
Twenty-two nursing students and 25 medical students (35 female/12 male; M age = 24.2) from a University in the Southwestern U.S. were recruited via email for a study on medical decision-making and paid $10 for their participation. When the study was completed, the experimenter led participants through a funnel debriefing procedure whereby they were asked to "guess" what images were flashed on the computer screen as a check on the success of the subliminal priming procedure. They were then fully debriefed regarding the aims of the research, paid, and thanked for their time. The University of Arizona Institutional Review Board approved this study. All participants provided consent before beginning the sequential priming task.
Materials and Procedure
Sequential priming task
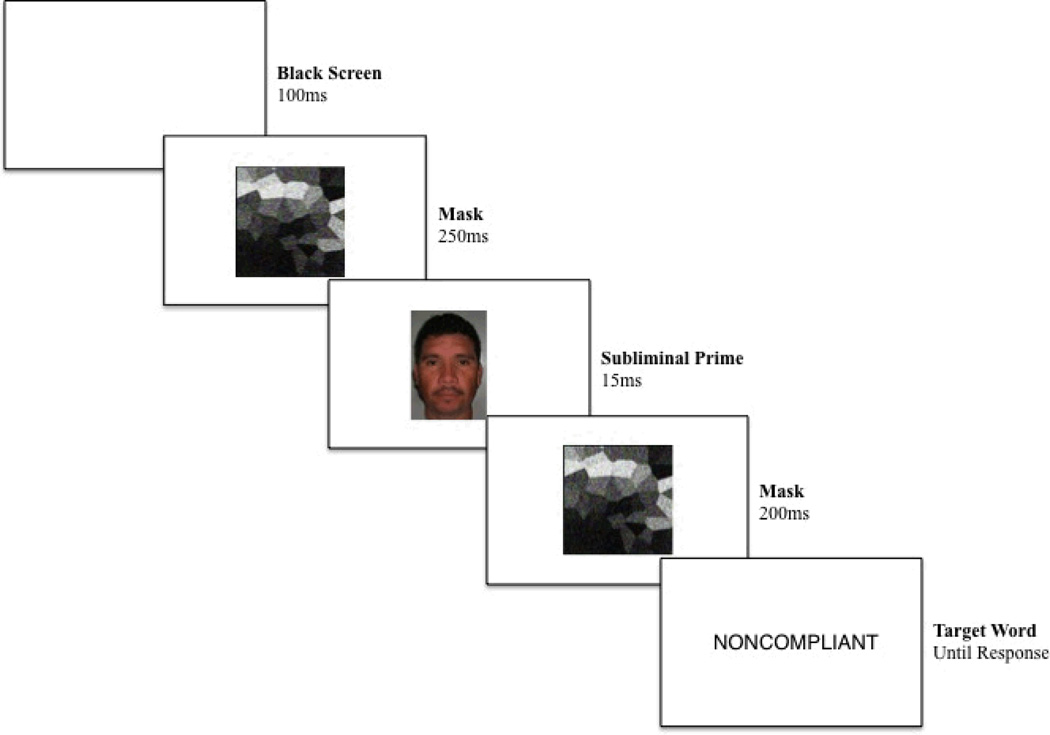
The sequential priming task consisted of 240 trials, separated into four blocks of 60 trials. Each trial included five components: a blank screen that appeared for 100ms, a visual mask that appeared for 250 ms, a critical image (either a Hispanic or a non-Hispanic White face for the critical trials or a blank slide for the filler trials) for 15 ms, the same visual mask for 200 ms, and then a letter string, which remained on the screen until participants made a selection (see Figure 1 for a schematic diagram). Half of the participants were instructed to press the “E” key when they believed a letter string was a word and the “I” key when they believed the letter string was a non-word, while the other half received the opposite instructions.
Figure 1.
Example trial from the sequential priming task.
Critical trials consisted of words semantically related to noncompliance (e.g., uncooperative), words related to the damaging effects of risky health behavior (e.g., damage), words related to general stereotypes of Hispanics (e.g., unimaginative), and control words unrelated to stereotypes of Hispanics (e.g., disgrace). The four categories of words were matched for length, and a pretest confirmed that the words in the four categories were perceived to be similarly negative in valence and that the control words were perceived as being unrelated to stereotypes of Hispanics. There were 34 critical trials total—each of the 17 critical words was shown once after a Hispanic face and once after a non-Hispanic White face. The other 206 trials consisted of filler words and non-words. Critical trials were distributed across the four blocks, and participants were primed with only Hispanic faces during two of the blocks and only non-Hispanic White faces during the other two. Blocks were counterbalanced so that some participants were first primed with Hispanic faces, while others were first primed with non-Hispanic White faces. Six color images, three of adult Hispanic male faces and three of adult non-Hispanic White male faces, pretested as being similar in age and attractiveness and standardized for size and color saturation, were used as prime images.
Motivation to respond without prejudice
A 10-item scale (Plant & Devine, 1998) was used to assess participant motivation to behave in a non-prejudiced way towards Hispanics for internal reasons (e.g., “I attempt to appear nonprejudiced toward Hispanic people because it is personally important to me”;α = .84) and external reasons (e.g., “Because of today’s politically correct standards, I try to appear non-prejudiced toward Hispanic people”;α = .77). Participants used 5-point Likert scales to rate the degree to which they agree with each statement (1 = Strongly Disagree, 5 = Strongly Agree). Ratings were averaged for internal motivation (IM) and external motivation (EM) questions separately.
Demographics
Participants were asked to report their racial/ethnic group membership, age, gender, and program affiliation (medical or nursing).
Results
Eleven participants were eliminated before the analyses. Six participants were eliminated because they were not native speakers of English and their behavior on the sequential priming task may have been influenced by the unfamiliarity of the word or non-word stimuli used. In addition, consistent with the requirements for subliminal priming, four participants were eliminated because they reported consciously perceiving faces of different ethnicities. Finally, one participant was eliminated for not following instructions. This left 36 participants in the analyses (19 nursing and 17 medical students). Due to the large proportion of non-Hispanic White (81%) and female (78%) participants, race and gender were not included in the analyses.
IM scores were highly positive (M = 4.29, SD = .61, range: 2.60 – 5.0), skewed, and invariant, so they were excluded from further analyses. EM scores were more normally distributed (M = 2.87, SD = .82, range: 1.0 – 4.80) and were included in the analyses. In line with previous research (Fazio, 1990), the response time data were screened and the distribution of scores was normalized prior to analysis. Incorrect responses and response times three standard deviations above the mean were eliminated. The remaining response times were log transformed and averaged for each word set. SAS GLM procedures were used to test the 4 (word type: noncompliance v. risk v. general stereotype v. control) X 2 (prime ethnicity: Hispanic v. non-Hispanic White) X 2 (program: medical v. nursing) X EM (continuous, centered) mixed design. The model tested all main effects and all possible interaction effects
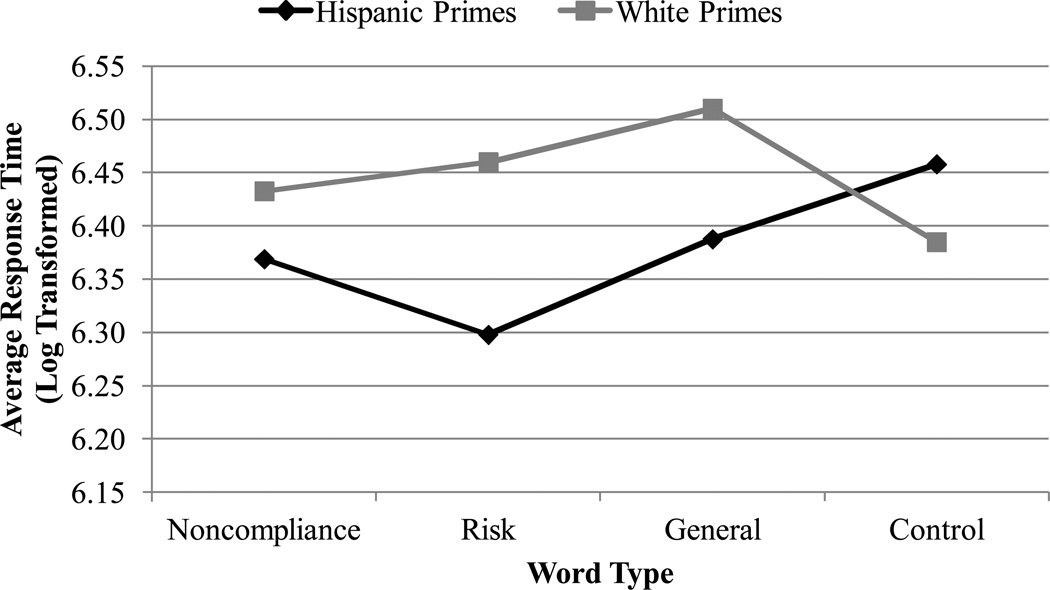
A summary of the significant main effects and interactions can be found in Table 1. Effects not included in the table were not significant, and they will not be discussed further. Results revealed the predicted interaction between word type and prime ethnicity (see Figure 2 for means and standard deviations, presented in raw form for ease of interpretation). Consistent with hypotheses, participants were faster to recognize noncompliance, risk, and general stereotype words after exposure to Hispanic, compared with non-Hispanic White, faces (see Table 2 for statistics). In contrast, participants were faster to recognize the control words after exposure to non-Hispanic White, compared with Hispanic, faces. Examining the effects of word type within the Hispanic prime trials (i.e., trials where a Hispanic face was flashed on the screen), consistent with hypotheses, participants were faster to recognize noncompliance, risk, and general stereotype words, than control words (see Table 3 for statistics). Within the non-Hispanic White prime trials, participants were faster to recognize control words than noncompliance, risk, and general stereotype words (see Table 4 for statistics). The results also revealed interactions between EM and program affiliation and between prime ethnicity and EM, but because these interaction effects collapse across the word sets, they are not discussed further.
Table 1.
Statistically Significant Effects from Overall Model
| Effect | df | F | p | η2p |
|---|---|---|---|---|
| Word Type | 3, 96 | 4.82 | < .01 | .13 |
| Prime Ethnicity | 1, 32 | 28.1 | < .001 | .23 |
| Word Type X Prime Ethnicity | 3, 96 | 15.3 | < .001 | .32 |
| Prime Ethnicity X EM | 1, 32 | 4.58 | < .05 | .05 |
| Program X EM | 1, 32 | 6.41 | < .05 | .06 |
Figure 2.
Average response times by word type and prime ethnicity.
Table 2.
Log Transformed Response Times for Hispanic and White Prime Trials for Each Word Category
| Hispanic Primes | White Primes | ||||||
|---|---|---|---|---|---|---|---|
| Word Category | M | SD | M | SD | F(1, 32) | p | d |
| Noncompliance | 6.369 | .094 | 6.433 | .092 | 13.0 | < .01 | .68 |
| Risk | 6.298 | .101 | 6.46 | .11 | 73.2 | < .001 | 1.53 |
| General Stereotype | 6.388 | .141 | 6.51 | .138 | 46.4 | < .001 | .88 |
| Control | 6.458 | .08 | 6.385 | .072 | 15.7 | < .001 | .96 |
Note. Time was originally measured in milliseconds.
Table 3.
Log Transformed Response Times for Each Word Category within Hispanic Prime Trials
| Category 1 | Category 2 | ||||||
|---|---|---|---|---|---|---|---|
| Word Group Comparison | M | SD | M | SD | F(1, 32) | p | d |
| Noncompliance v. Risk | 6.369 | .094 | 6.298 | .101 | 13.6 | < .001 | .73 |
| Noncompliance v. General | 6.369 | .094 | 6.388 | .141 | n.s. | ||
| Noncompliance v. Control | 6.369 | .094 | 6.458 | .08 | 23.2 | < .001 | 1.02 |
| Risk v. General | 6.298 | .101 | 6.388 | .141 | 20.5 | < .001 | .73 |
| Risk v. Control | 6.298 | .101 | 6.458 | .08 | 72.4 | < .001 | 1.76 |
| General v. Control | 6.388 | .141 | 6.458 | .08 | 15.8 | < .001 | .61 |
Note. Time was originally measured in milliseconds.
Table 4.
Log Transformed Response Times for Each Word Category within White Prime Trials
| Category 1 | Category 2 | ||||||
|---|---|---|---|---|---|---|---|
| Word Group Comparison | M | SD | M | SD | F(1, 32) | p | d |
| Noncompliance v. Risk | 6.433 | .092 | 6.46 | .11 | n.s. | ||
| Noncompliance v. General | 6.433 | .092 | 6.51 | .137 | 16.4 | < .001 | .66 |
| Noncompliance v. Control | 6.433 | .092 | 6.385 | .072 | 7.55 | < .01 | .58 |
| Risk v. General | 6.46 | .11 | 6.51 | .137 | 7.76 | < .01 | .40 |
| Risk v. Control | 6.46 | .11 | 6.385 | .072 | 16.1 | < .001 | .80 |
| General v. Control | 6.51 | .137 | 6.385 | .072 | 46.2 | < .001 | 1.14 |
Note. Time was originally measured in milliseconds.
Discussion
The present study makes several novel contributions to research on nonconscious cognition in health care. It is one of the first studies to demonstrate that nursing and medical students exhibit nonconscious stereotype activation. Further, participants exhibited activation of both noncompliance and health risk stereotypes regarding Hispanics—a stigmatized patient group that, to date, has received little attention in the literature. Finally, this research documents nonconscious stereotyping using a task that does not motivate participants to appear nonbiased.
Research suggests that implicit bias and stereotyping can affect how health care personnel treat and interact with patients. Multiple studies have found that physicians’ implicit biases predict disparate treatment recommendations for African American, compared with non-Hispanic White, patients (Green et al., 2007; Sabin & Greenwald, 2012), and African-American patients’ satisfaction with their health care is influenced by their physicians’ level of implicit bias (Penner et al., 2010). Future research should assess whether the implicit activation of noncompliance or health risk stereotypes also has pernicious effects on health care practitioners’ interactions with Hispanic patients.
The present research examined nonconscious stereotyping among nursing and medical students—groups that are in the early stages of learning about cultural competence in health care. Future research should examine whether nurses and physicians who have been working in health care for an extended period time also exhibit nonconscious stereotyping of Hispanic patients, because prolonged contact with Hispanic patients could serve to either bolster or disconfirm stereotypes (Pettigrew & Tropp, 2006; Stephan, Diaz-Loving, & Duran, 2000).
The results of the present study indicate that nursing and medical students exhibit nonconscious stereotype activation, regardless of their explicit motivations to control prejudice toward Hispanics. This finding suggests that explicit goals to avoid bias do not always protect individuals against the automatic activation of negative beliefs about minority patients. To reduce nonconscious forms of bias, nursing and medical students may need to receive instruction on how to control their automatic responses to minority patients. For example, cultural competence courses could include workshops that expose students to strategies for controlling nonconscious stereotyping (Stone & Moskowitz, 2011). Training nursing and medical students in the psychology of nonconscious cognition may be as important as discussions of explicit stereotyping for eliminating the unintended antecedents of racial and ethnic health disparities.
Acknowledgment
The authors acknowledge research was supported by NIH grant #5R01MD005902-02 awarded to Jeff Stone, Gordon B. Moskowitz, and Terry A. Badger.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors of have no conflicts of interest to report.
Contributor Information
Meghan G. Bean, Department of Psychology, University of Arizona.
Jeff Stone, Department of Psychology, University of Arizona.
Terry A. Badger, College of Nursing, University of Arizona.
Elizabeth S. Focella, Department of Psychology, University of Arizona.
Gordon B. Moskowitz, Department of Psychology, Lehigh University.
References
- Agency for Healthcare Research and Quality. 2009 national healthcare disparities report. Rockville, MD: U.S. Department of Health and Human Services; 2010. Retrieved from http://www.ahrq.gov/research/findings/nhqrdr/nhdr09/index.html. [Google Scholar]
- Bargh JA, Chartrand TL. The mind in the middle: A practical guide to priming and automaticity research. In: Reis HT, Judd CM, editors. Handbook of Research Methods in Social and Personality Psychology. New York, NY: Cambridge University Press; 2000. pp. 253–285. [Google Scholar]
- Bean MG, Focella ES, Stone J, Moskowitz GB, Badger TA. Evidence for the diverse forms of bias that medical and nursing students hold toward Hispanic and Native American patients (under review). [Google Scholar]
- Conrey FR, Sherman JW, Gawronski B, Hugenberg K, Groom CJ. Separating multiple processes in implicit social cognition: The Quad Model of implicit task performance. Journal of Personality and Social Psychology. 2005;89:469–487. doi: 10.1037/0022-3514.89.4.469. [DOI] [PubMed] [Google Scholar]
- Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, Greenwald AG, Inui TS. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. American Journal of Public Health. 2012;102:979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine PG, Monteith MJ. Automaticity and control in stereotyping. In: Chaiken S, Trope Y, editors. Dual-process theories in social psychology. New York, NY: Guilford Press; 1999. pp. 339–360. [Google Scholar]
- Dick HP. Making immigrants illegal in small-town USA. Journal of Linguistic Anthropology. 2011;21:E35–E55. [Google Scholar]
- Dixon JC, Rosenbaum MS. Nice to know you? Testing contact, cultural, and group threat theories of anti-Black and anti-Hispanic stereotypes. Social Science Quarterly. 2004;85:257–280. [Google Scholar]
- Fiedler K, Bluemke M. Faking the IAT: Aided and unaided response control on the Implicit Association Tests. Basic and Applied Social Psychology. 2005;27:307–316. [Google Scholar]
- Fiske S. Stereotyping, prejudice, and discrimination. In: Lindzey G, Gilbert D, Fiske S, editors. The handbook of social psychology. New York, NY: McGraw-Hill; 1998. pp. 357–411. [Google Scholar]
- Gordon HS, Street RL, Jr, Sharf BF, Souchek J. Racial differences in doctors’ information-giving and patients’ participation. Cancer. 2006;107:1313–1320. doi: 10.1002/cncr.22122. [DOI] [PubMed] [Google Scholar]
- Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, Banaji MR. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. Journal of General Internal Medicine. 2007;22:1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory K, Wells KB, Leake B. Medical students’ expectations for encounters with minority and nonminority patients. Journal of the National Medical Association. 1987;79:403–408. [PMC free article] [PubMed] [Google Scholar]
- Johnson RL, Saha S, Arbelaez JJ, Beach MC, Cooper LA. Racial and ethnic differences in patient perceptions of bias and cultural competence in health care. Journal of General Internal Medicine. 2004;19:101–110. doi: 10.1111/j.1525-1497.2004.30262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawakami K, Dovidio JF. The reliability of implicit stereotyping. Personality and Social Psychology Bulletin. 2001;27:212–225. [Google Scholar]
- Lopez-Quintero C, Crum RM, Neumark YD. Racial/ethnic disparities in report of physician-provided smoking cessation advice: Analysis of the 2000 National Health Interview Survey. Research and Practice. 2006;96:2235–2239. doi: 10.2105/AJPH.2005.071035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mead H, Cartwright-Smith L, Jones K, Ramos C, Woods K, Siegel R. Racial disparities in U.S. health care: A chartbook. New York, NY: The Commonwealth Fund; 2008. [Google Scholar]
- Moskowitz GB, Stone J, Childs A. Implicit stereotyping and medical decisions: Unconscious stereotype activation in practitioners’ thoughts about African Americans. American Journal of Public Health. 2012;102(5):996–1001. doi: 10.2105/AJPH.2011.300591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Dovidio JF, West TV, Gaertner SL, Albrecht TL, Dailey RK, Markova T. Aversive racism and medical interactions with Black patients: A field study. Journal of Experimental Social Psychology. 2010;46:436–440. doi: 10.1016/j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettigrew TF, Tropp LR. A meta-analytic test of intergroup contact theory. Journal of Personality and Social Psychology. 2006;90:751–783. doi: 10.1037/0022-3514.90.5.751. [DOI] [PubMed] [Google Scholar]
- Plant EA, Devine PG. Internal and external motivation to respond without prejudice. Journal of Personality and Social Psychology. 1998;75:811–832. doi: 10.1177/0146167205275304. [DOI] [PubMed] [Google Scholar]
- Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: Pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. American Journal of Public Health. 2012;102:988–995. doi: 10.2105/AJPH.2011.300621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekaquaptewa D, Espinoza P, Thompson M, Vergas P, von Hippel W. Stereotypic explanatory bias: Implicit stereotyping and a predictor of discrimination. Journal of Experimental Social Psychology. 2003;39:75–82. [Google Scholar]
- Sheeran P, Gollwitzer PM, Bargh JA. Nonconscious processes and health. Health Psychology. 2013;13:460–473. doi: 10.1037/a0029203. [DOI] [PubMed] [Google Scholar]
- Stephan WG, Diaz-Loving R, Duran A. Integrated threat theory and intercultural attitudes: Mexico and the United States. Journal of Cross-Cultural Psychology. 2000;31:240–249. [Google Scholar]
- Stone J, Moskowitz GB. Non-conscious racial bias in medical decision making: What can be done to reduce it? Medical Education. 2011;45:768–776. doi: 10.1111/j.1365-2923.2011.04026.x. [DOI] [PubMed] [Google Scholar]
- Wittenbrink B, Judd CM, Park B. Evidence for racial prejudice at the implicit level and its relationship with questionnaire measures. Journal of Personality and Social Psychology. 1997;72:262–274. doi: 10.1037//0022-3514.72.2.262. [DOI] [PubMed] [Google Scholar]