Abstract
Objective
To compare the effects of antiplatelets and anticoagulants on stroke and death in patients with acute cervical artery dissection.
Design
Systematic review with Bayesian meta-analysis.
Data Sources
The reviewers searched MEDLINE and EMBASE from inception to November 2012, checked reference lists, and contacted authors.
Study Selection
Studies were eligible if they were randomised, quasi-randomised or observational comparisons of antiplatelets and anticoagulants in patients with cervical artery dissection.
Data Extraction
Data were extracted by one reviewer and checked by another. Bayesian techniques were used to appropriately account for studies with scarce event data and imbalances in the size of comparison groups.
Data Synthesis
Thirty-seven studies (1991 patients) were included. We found no randomised trial. The primary analysis revealed a large treatment effect in favour of antiplatelets for preventing the primary composite outcome of ischaemic stroke, intracranial haemorrhage or death within the first 3 months after treatment initiation (relative risk 0.32, 95% credibility interval 0.12 to 0.63), while the degree of between-study heterogeneity was moderate (τ2 = 0.18). In an analysis restricted to studies of higher methodological quality, the possible advantage of antiplatelets over anticoagulants was less obvious than in the main analysis (relative risk 0.73, 95% credibility interval 0.17 to 2.30).
Conclusion
In view of these results and the safety advantages, easier usage and lower cost of antiplatelets, we conclude that antiplatelets should be given precedence over anticoagulants as a first line treatment in patients with cervical artery dissection unless results of an adequately powered randomised trial suggest the opposite.
Introduction
Dissections of cervical carotid or vertebral arteries are among the most frequent causes of ischaemic stroke in young adults according to hospital-based series [1]–[3]. More than a quarter of patients with stroke caused by cervical artery dissection develop relevant disability, while almost half report a decreased quality of life [4]. The socio-economic consequences are significant, because patients with cervical artery dissection are on average 45 years of age and play an important role in private, business and social life [5]. Brain imaging studies and detection of micro-embolic signals by transcranial ultrasound in patients with cervical artery dissection suggest that arterial embolism is the main mechanism of stroke [6], [7]. Most physicians prescribe anticoagulants for stroke prevention in patients with acute cervical artery dissection, although no randomised trial has compared the safety and efficacy of anticoagulants with antiplatelets or placebo. In addition, the International Stroke Trial has shown that the potential benefit of anticoagulants is offset by an increased risk of intracranial haemorrhage in patients with acute ischaemic stroke [8].
Hitherto, three meta-analyses comparing antiplatets and anticoagulants in patients with cervical artery dissection were published [9]–[11]. All three used frequentist methods for statistical analysis. Summary estimates, uncertainty, and statistical significance vary depending on the analytical approach used. In the presence of many studies with scarce or zero events in either or both groups and imbalances in the size of comparison groups, the statistical analysis becomes challenging [12], [13]. This is the case for many of the studies comparing antiplatelets and anticoagulants in patients with cervical artery dissection. The original Cochrane Review and its recent update excluded studies with zero events in both groups [9], [11]. This approach may have biased results in either direction, particularly in view of the considerable imbalances in group sizes. Menon and colleagues included studies with zero events in both groups [10], but the analytical technique used gave undue weight to studies with zero events in both groups and is therefore likely to have biased results towards underestimating potential differences in the effects of antiplatelets and anticoagulants. Therefore, we conducted a systematic review and meta-analysis using appropriate Bayesian techniques to account for studies with scarce event data. We compared the effects of antiplatelets and anticoagulants on the composite of ischaemic stroke, intracranial haemorrhage or death as primary outcome, and determined whether estimated treatment effects differed according to the site of dissection or methodological quality of included studies.
Methods
Data Sources and Searches
We searched MEDLINE and EMBASE (from inception to November 2012) using a combination of keywords, text words, and specific database terms related to carotid and vertebral artery dissection and to interventions (see Appendix S1). Search strategies were developed by an experienced medical librarian in collaboration with neurologists experienced in the field of interest (HS, RWB). We used similar strategies to identify previously published systematic reviews and meta-analysis, searched clinical trial registries, screened reference lists of all retrieved reports and contacted experts in the field. There were no restrictions regarding language or publication status. See Appendix S2 for the review protocol.
Study Selection
We included any randomised, quasi-randomised or observational study that allowed a within-study comparison of antiplatelets and anticoagulants administered for an intended duration of at least 3 months in patients with cervical artery dissection. Patients with intended shorter durations of treatment or with treatment regimens including a switch from one treatment to the other before 3 months were excluded, as were patients who underwent a surgical intervention of the dissected artery, patients with traumatic or isolated intracranial dissections, and children. Therefore, patient numbers reported here will not necessarily correspond to those previously published. Dissections were considered to be of traumatic origin in the presence of severe blunt head or neck traumas, occuring most often due to motor vehicle accidents [14], [15]. Conversely, dissections associated with minor trauma (e.g. sneezing, coughing, vomiting, minor injuries after sport or recreational activities) were considered spontaneous and included [16], [17]. Studies which did not provide 3 month follow-up data were excluded, as were case series in patients only treated with one of the interventions. Eligibility of all reports was determined by one reviewer (HS) and independently checked by one out of three other reviewers (RWB, BdC, or PJ).
Outcome Measures
The primary outcome was the composite of ischaemic stroke, symptomatic intracranial haemorrhage or death occurring up to three months after initiation of antithrombotic treatment. Secondary outcomes were the composite of ischaemic stroke or symptomatic intracranial haemorrhage; ischaemic stroke; symptomatic intracranial haemorrhage; transient ischaemic attack; death; and the composite of ischaemic stroke or transient ischaemic attack. If three-month follow-up data were not available in published reports, we requested these data from authors.
Data Extraction and Quality Assessment
Data on clinical outcomes and methodological quality were extracted by one reviewer (HS) and checked by another (BdC). We contacted the corresponding authors if additional information on outcome data was required for the specified follow-up period, or for the eligible patient population, overall or stratified by site of dissection (carotid or vertebral). The following components of methodological quality that may be associated with bias in therapeutic research were assessed: prospective design; enrolment of consecutive patients with cervical artery dissection; blinding of investigators responsible for the adjudication of clinical events; and inclusion of all enrolled patients in the analysis (in analogy to the intention-to-treat principle used in randomised trials). In addition, we classified studies according to their size and according to balance in the size of treatment groups. Studies were considered have balanced sizes of treatment groups if the difference in the number of patients between groups was less than fourfold. For example, a study had included 83 patients receiving aspirin and 47 receiving anticoagulants and was considered to be balanced [18]. Conversely, another study had included 9 patients receiving aspirin and 113 receiving anticoagulants and was deemed to have unbalanced sizes of treatment groups [19]. Studies were considered large if they had included more than 15 patients in each treatment group, and more than 50 patients overall. Disagreements were resolved by consensus.
Statistical Analysis
We used a Bayesian method developed for random effects meta-analysis on the relative risk scale [20], [21]. The model adequately accounts for situations with sparse event data, including zero cells in one or both treatment groups. Monte-Carlo Markov Chain simulation methods were used to obtain posterior distributions of the relative risks (RRs) of outcomes of interest and of τ2. Pooled RRs were estimated from the median of the respective posterior distributions [21]. An RR below one indicates a benefit of antiplatelets as compared with anticoagulants. 95% credibility intervals (95% CrI) were obtained from the 2.5th and the 97.5th percentile of the posterior distribution, which can be interpreted similarly to a conventional 95% confidence interval. Between-study heterogeneity was considered low if the median of the posterior distribution of τ2 was 0.04 or less; τ2 estimates of 0.14 may be interpreted as a moderate and 0.40 as a high degree of heterogeneity between studies [22], [23]. Analyses were performed overall in all patients, and stratified according to site of dissection (carotid or vertebral). For three outcomes, we observed high degrees of heterogeneity; we identified the study contributing most to between-study heterogeneity and repeated the analyses after exclusion of this study.
For the primary composite outcome, we performed analyses of the overall population stratified by the following pre-specified methodological criteria: prospective design; enrolment of consecutive patients; inclusion of all enrolled patients in the analysis; study size; and balanced size of treatment groups. We also stratified the analysis of the primary composite outcome according to two post hoc classifications according to methodological quality: studies that satisfied all five of the above criteria (prospective design, consecutive patients, inclusion of all patients in the analysis, balanced group size and large sample size overall) versus studies that did not; studies, for which we were able to reconfirm with authors that outcome data included in our analysis were complete, versus studies for which this was not the case. All stratified analyses were accompanied by tests for interaction between study characteristic and treatment effect. Then, we performed a post hoc analysis of all outcomes restricted to studies that satisfied all five pre-specified methodological criteria [24]. After the publication of the International Stroke Trial in 1997, patients with severe stroke were more likely to receive antiplatelets than anticoagulants due to the lower risk of intracranial haemorrhage [8]. We therefore determined whether there was evidence for confounding by indication by stratifying the analysis of overall mortality according to time-point of death (≤7 days versus >7 days after symptoms onset). Finally, we re-analysed the two previous meta-analyses [10], [11] using our Bayesian random-effects model. Then, we compared results from intersecting studies, which were included in our meta-analysis as well as in those previously published, with results from studies only included in our meta-analysis, and studies only included in the previously published meta-analyses, but excluded from ours. See Appendix S3 for an extended description of statistical methods. Analyses were done using Stata version 11.0 and WinBUGS version 1.4.3 [25], [26].
Results
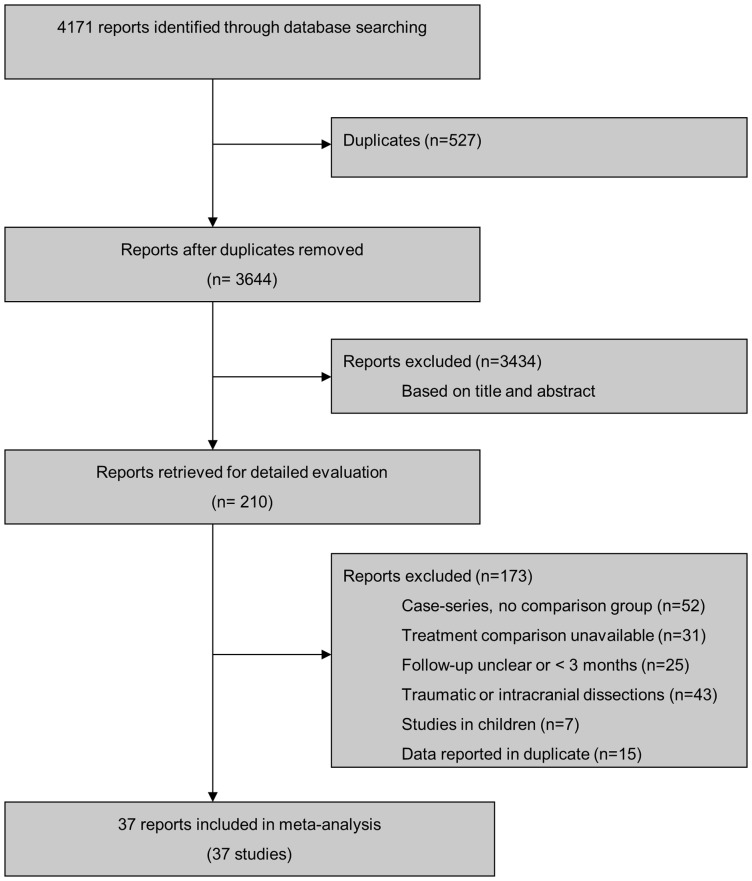
We identified 4171 unique references through our literature search and considered 210 for detailed evaluation ( Figure 1 ). Thirty-seven studies performed in 1991 patients fulfilled our eligibility criteria and were included. All were published as full-text articles. The median year of publication was 1998 (range, 1978 to 2012). All 37 studies were observational, allowing a comparison of antiplatelets with anticoagulants [18], [19], [27]–[61]. No randomised trial was identified. The median number of patients per study was 21 (range, 2 to 315), with 527 (26%) patients receiving antiplatelets and 1464 (74%) receiving anticoagulants. Twenty-four studies reported outcomes for 1039 patients with internal carotid artery dissection [18], [27]–[33], [35], [37]–[40], [45], [47], [49]–[51], [54]–[58], [60]. Fifteen studies reported outcomes for 532 patients with vertebral artery dissection [18], [34], [36], [42]–[44], [46], [49]–[52], [54], [55], [58], [59]. Two studies (223 patients) had included patients with internal carotid or vertebral dissection, but clinical outcomes stratified according to site of dissection were unavailable [19], [48]. Table 1 presents the methodological characteristics of included studies. Prospective design was reported in 10 studies (27%) including 874 patients [18], [44], [45], [48], [50], [52], [53], [57], [59], [61], and recruitment of consecutive patients in 19 studies (51%) with 1673 patients [18], [19], [31], [32], [34], [44]–[50], [52]–[55], [57]–[59]. Nineteen studies (51%) with a total of 1029 patients included all eligible patients in the analysis [18], [19], [27], [29], [30], [37], [38], [40]–[42], [45], [47], [48], [50], [53], [56], [57], [59], [60]. Twenty-nine studies (78%) including 1125 patients satisfied our criteria of balanced group sizes [18], [27]–[31], [33], [35]–[48], [50], [52]–[57], [61], and eight studies including 1146 patients were considered large [18], [40], [48], [49], [52], [53], [57], [61]. Four studies (11%) in 631 patients satisfied all 5 criteria and were considered to be of higher methodological quality overall [18], [48], [53], [57]. None of the included studies reported blinding of investigators responsible for the adjudication of clinical events. For 16 studies, we were able to reconfirm with investigators that outcome data included in our analysis were complete [18], [19], [37], [44], [47], [49]–[55], [57]–[60].
Figure 1. Study flow diagram.
Table 1. Characteristics of identified studies.
| Study, Year (Reference) | Study Population | Prospective | Consecutive | No exclusions* | Balanced group size | Large |
| Fisher et al. 1978 [27] | carotid | no | unclear | yes | yes | no |
| Luken et al. 1979 [28] | carotid | unclear | unclear | no | yes | no |
| Sellier et al. 1983 [29] | carotid | unclear | unclear | yes | yes | no |
| Vanneste et al. 1984 [30] | carotid | no | no | yes | yes | no |
| Mokri et al. 1986 [31] | carotid | no | yes | no | yes | no |
| Bogousslavsky et al. 1987 [32] | carotid | unclear | yes | no | no | no |
| Marx et al. 1987 [33] | carotid | unclear | unclear | no | yes | no |
| Mas et al. 1987 [34] | vertebral | unclear | yes | no | no | no |
| Landre et al. 1987 [35] | carotid | no | no | no | yes | no |
| Mokri et al. 1988 [36] | vertebral | unclear | unclear | no | yes | no |
| De Bray et al. 1989 [37] | carotid | unclear | unclear | yes | yes | no |
| Eljamel et al. 1990 [38] | carotid | unclear | unclear | yes | yes | no |
| Schievink et al. 1990 [39] | both | unclear | unclear | no | yes | no |
| Ast et al. 1993 [40] | carotid | no | unclear | yes | yes | yes |
| Landini et al. 1996 [41] | both | unclear | unclear | yes | yes | no |
| Pego et al. 1996 [42] | vertebral | no | unclear | yes | yes | no |
| Plaza et al. 1996 [43] | vertebral | unclear | unclear | no | yes | no |
| De Bray et al. 1997 [44] | vertebral | yes | yes | no | yes | no |
| Biousse et al. 1998 [45] | carotid | yes | yes | yes | yes | no |
| Han et al. 1998 [46] | vertebral | no | yes | no | yes | no |
| Engelter et al. 2000 [47] | carotid | no | yes | yes | yes | no |
| Beletsky et al. 2003 [48] | both | yes | yes | yes | yes | yes |
| Dziewas et al. 2003 [19] | both | no | yes | yes | no | no |
| Touzé et al. 2003 [49] | both | no | yes | no | no | yes |
| Caso et al. 2004 [51] | both | no | yes | yes | yes | no |
| Campos et al. 2004 [50] | both | yes | unclear | no | no | no |
| Arauz et al. 2006 [18] | both | yes | yes | yes | yes | yes |
| Arnold et al. 2006 [52] | vertebral | yes | yes | no | yes | yes |
| De Bray et al. 2007 [53] | both | yes | yes | yes | yes | yes |
| Nyberg et al. 2007 [54] | both | no | yes | no | yes | no |
| Simoes et al. 2007 [55] | both | no | yes | no | yes | no |
| Rigamonti et al. 2008 [56] | carotid | no | no | Yes | yes | no |
| Georgiadis et al. 2009 [57] | carotid | yes | yes | yes | yes | yes |
| Metso et al. 2009 [58] | both | no | yes | no | no | no |
| Arauz et al. 2010 [59] | vertebral | yes | yes | yes | no | no |
| Divjak et al. 2011 60 | carotid | no | no | yes | no | no |
| Kennedy et al. 2012 61 | both | no | no | yes | yes | yes |
No exclusions refers to no exclusions of eligible patients from the analysis.
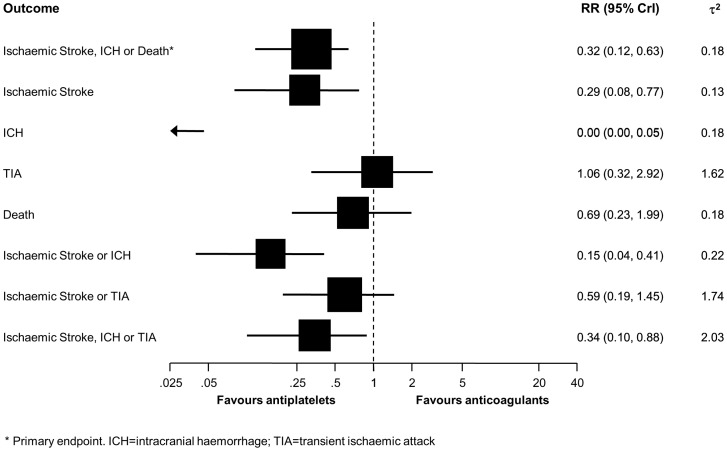
Table 2 presents the clinical outcomes of all included studies. Thirty-six studies contributed to the analysis of the primary composite outcome of ischaemic stroke, intracranial haemorrhage or death [18], [19], [27]–[60]. Sixty-one patients experienced the primary composite outcome, 13 of 467 patients with antiplatelets and 48 of 1416 patients with anticoagulants. Figure 2 (top) indicates an advantage of antiplatelets over anticoagulants, with a 68% reduction in the relative risk of ischaemic stroke, intracranial haemorrhage or death afforded by antiplatelets (RR 0.32, 95% CrI 0.12 to 0.63). A τ2 of 0.18 indicated a moderate degree of between-study heterogeneity.
Table 2. Number of included patients and events reported in included studies.
| Antiplatelets | Anticoagulants | |||||||||||||||||
| Study, Year (Ref) | Number included | IS, ICH or death* | IS | ICH | TIA | Death | IS or ICH | IS or TIA | IS, ICH or TIA | Number included | IS, ICH or death* | IS | ICH | TIA | Death | IS or ICH | IS or TIA | IS, ICH or TIA |
| Fisher 1978 27 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 2 | 0 | 1 | 2 | 1 | 1 | 2 | 3 |
| Luken 1979 28 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Sellier 1983 29 | 13 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Vanneste 1984 30 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 |
| Mokri 1986 31 | 9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 |
| Bogousslavsky 1987 32 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 19 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Marx 1987 33 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 |
| Mas 1987 34 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Landre E 1987 35 | 3 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 |
| Mokri B 1988 36 | 9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| De Bray 1989 37 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 14 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Eljamel 1990 38 | 4 | 0 | 0 | 0 | 3 | 0 | 0 | 3 | 3 | 4 | 0 | 0 | 0 | 2 | 0 | 0 | 2 | 2 |
| Schievink 1990 39 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ast 1993 40 | 21 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 30 | 1 | 1 | 0 | 1 | 0 | 1 | 2 | 2 |
| Landini 1996 41 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Pego 1996 42 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Plaza 1996 43 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 |
| De Bray 1997 44 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biousse 1998 45 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 |
| Han 1998 46 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Engelter 2000 47 | 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 25 | 3 | 2 | 0 | 1 | 1 | 2 | 3 | 3 |
| Beletsky 2003 48 | 23 | 1 | 1 | 0 | 1 | 0 | 1 | 2 | 2 | 78 | 4 | 2 | 0 | 1 | 2 | 2 | 3 | 3 |
| Dziewas 2003 19 | 9 | 0 | 0 | 0 | 6 | 0 | 0 | 6 | 6 | 113 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 2 |
| Touzé 2003 49 | 18 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 297 | 4 | 1 | 0 | 1 | 3 | 1 | 2 | 2 |
| Caso 2004 50 | 20 | 2 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 18 | 2 | 1 | 0 | 0 | 1 | 1 | 1 | 1 |
| Campos 2004 51 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 33 | 4 | 2 | 0 | 0 | 2 | 2 | 2 | 2 |
| Arauz 2006 18 | 82 | 7 | 3 | 0 | . | 4 | 3 | . | . | 48 | 3 | 3 | 0 | . | 0 | 3 | . | . |
| Arnold 2006 52 | 38 | 2 | 0 | 0 | 2 | 2 | 0 | 2 | 2 | 24 | 4 | 3 | 1 | 3 | 0 | 4 | 6 | 7 |
| De Bray 2007 53 | 31 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 71 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Nyberg 2007 54 | 15 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 21 | 3 | 1 | 0 | 0 | 2 | 1 | 1 | 1 |
| Simoes 2007 55 | 13 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 29 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Rigamonti 2008 56 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Georgiadis 2009 57 | 96 | 0 | 0 | 0 | 2 | 0 | 0 | 2 | 2 | 202 | 3 | 1 | 2 | 8 | 0 | 3 | 9 | 11 |
| Metso 2009 58 | 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 281 | 9 | 4 | 3 | 7 | 2 | 7 | 11 | 14 |
| Arauz 2010 59 | 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 40 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Divjak 2011 60 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 20 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Kennedy 2012 61 | 59 | . | 1 | . | 3 | 0 | . | 4 | . | 28 | . | 1 | . | 0 | 0 | . | 1 | . |
Primary endpoint.
IS = Ischaemic Stroke; ICH = intracranial haemorrhage; TIA = transient ischaemic attack.
Ref = references.
Figure 2. Pooled relative risks of primary and secondary outcomes comparing antiplatelets with anticoagulants.
* Primary endpoint. ICH = intracranial haemorrhage; TIA = transient ischaemic attack.
Thirty-seven studies in 527 patients with antiplatelets and 1464 patients with anticoagulants contributed to the analysis of the ischaemic stroke and death (Table 2) [18], [19], [27]–[61]. Six patients with antiplatelets and 24 patients with anticoagulants experienced an ischaemic stroke. The pooled relative risk was 0.29 (95% CrI 0.08 to 0.77) and a τ2 of 0.13 indicated a moderate heterogeneity between studies ( Figure 2 ). Eight patients with antiplatelets and 15 patients with anticoagulants died during the follow-up of 3 months (pooled RR 0.69, 95% CrI 0.23 to 1.99), with a moderate heterogeneity between studies (τ2 = 0.18, Figure 2). The pooled RR was higher for deaths occurring within 7 days of treatment initiation (RR 1.20, 95% CrI 0.30 to 4.41) than for death occurring thereafter (RR 0.19, 95% 0.01 to 152), but a test for interaction between time of death and estimated RR did not provide strong evidence for the presence of interaction (p for interaction = 0.14).
Thirty-six studies in 468 patients with antiplatelets and 1436 patients with anticoagulants contributed to the analyses of intracranial haemorrhage and the composite of ischaemic stroke and intracranial haemorrhage [18], [19], [27]–[60]. Intracranial haemorrhages occurred in none of the patients with antiplatelets, but in 10 patients with anticoagulants. Accordingly, the pooled RR was estimated at 0.00 (95% CrI 0.00 to 0.05), and a τ2 of 0.18 indicated a moderate statistical heterogeneity ( Figure 2 ). Five patients with antiplatelets and 33 patients with anticoagulants experienced the composite of ischaemic stroke or intracranial haemorrhage. The pooled RR was 0.15 (95% CrI 0.04 to 0.41) and the heterogeneity between studies moderate (τ2 = 0.22, Figure 2).
Thirty-six studies in 445 patients with antiplatelets and 1416 patients with anticoagulants contributed to the analysis of transient ischaemic attack and the composite of ischaemic stroke or transient ischaemic attack [19], [27]–[61]. Eighteen patients with antiplatelets and 29 patients with anticoagulants experienced a transient ischaemic attack and there was little evidence for a difference between groups (RR 1.06, 95% CrI 0.32 to 2.92), but a high degree of heterogeneity between studies (τ2 = 1.62, Figure 2). Twenty-one patients with antiplatelets and 50 patients with anticoagulants experienced the composite of ischaemic stroke or transient ischaemic attack. The pooled RR was 0.59 (95% CrI 0.19 to 1.45), but the heterogeneity between studies was large (τ2 = 1.74).
Thirty-five studies in 386 patients with antiplatelets and 1388 patients with anticoagulants contributed to the analysis of the composite outcome of ischaemic stroke, intracranial haemorrhage or transient ischaemic attack.) [19], [27]–[60]. Seventeen patients with antiplatelets and 59 patients with anticoagulants experienced the composite of ischaemic stroke, intracranial haemorrhage or transient ischaemic attack. The pooled RR was 0.34 (95% CrI 0.10 to 0.88) and a τ2 of 2.03 again indicated large statistical heterogeneity.
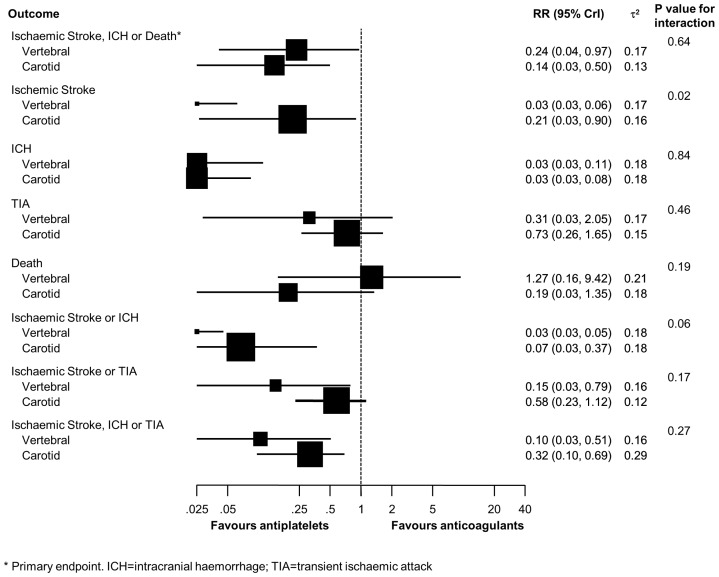
Figure 3 presents results of analyses stratified according to site of dissection. Estimates varied to some extent according to dissection site, but tests for interaction were negative for 7 out of the 8 outcomes, including the primary composite of ischaemic stroke, intracranial haemorrhage or death. The test for interaction between site of dissection and estimated treatment effect was positive, however, for ischaemic stroke (p for interaction = 0.02), suggesting a more pronounced benefit of antiplatelets in patients with vertebral dissection.
Figure 3. Analyses stratified according to site of dissection.
* Primary endpoint. ICH = intracranial haemorrhage; TIA = transient ischaemic attack.
Table 3 presents results from analyses of the primary outcome stratified according to study characteristics. Throughout, estimated relative risks were nearer 1 in studies that satisfied a methodological criterion. Tests for interaction between estimated relative risks and methodological criteria formally reached statistical significance for prospective study design (p for interaction = 0.01) and balanced group size (p for interaction = 0.04), and a statistical trend for consecutive recruitment of patients (p for interaction = 0.06).
Table 3. Stratified analyses of the primary outcome according to methodological quality.
| Variable | Total Studies, n | Number of patients included | RR (95% CrI) | τ2 * | P Value for interaction |
| All studies | 37 | 1991 | 0.32 (0.12−0.63) | 0.18 | |
| Prospective design | 0.13 | 0.01 | |||
| Yes | 10 | 874 | 0.62 (0.22−1.47) | ||
| No | 27 | 1117 | 0.05 (0.00−0.30) | ||
| Consecutive enrolment of patients | 0.16 | 0.06 | |||
| Yes | 19 | 1673 | 0.45 (0.16−0.98) | ||
| No | 18 | 318 | 0.09 (0.00−0.52) | ||
| Intention-to-treat analysis | 0.13 | 0.06 | |||
| Yes | 19 | 1029 | 0.52 (0.16−1.18) | ||
| No | 18 | 962 | 0.15 (0.03−0.51) | ||
| Balanced size of treatment groups | 0.15 | 0.04 | |||
| Yes | 29 | 1131 | 0.35 (0.13−0.67) | ||
| No | 8 | 860 | 0.00 (0.00−0.55) | ||
| Large sample size | 0.17 | 0.08 | |||
| Yes | 8 | 1146 | 0.51 (0.15−1.31) | ||
| No | 29 | 845 | 0.17 (0.04−0.51) |
Note that only one τ2 was estimated per outcome.
Table 4 shows results from a post hoc analysis of all outcomes restricted to studies that satisfied all five pre-specified methodological criteria. Compared with the analysis of all studies, estimates became less beneficial for antiplatelets on all outcomes except transient ischaemic attack. 95% CrI all overlapped the null effect at a RR of 1 for all outcomes, except intracranial haemorrhage. Studies that satisfied all five pre-specified methodological criteria showed a pooled RR of 0.73 (95% CrI 0.17 to 2.30), studies that satisfied four criteria or less showed a pooled RR of 0.20 (95% CrI 0.06 to 0.47; p for interaction = 0.07). For the 16 studies, for which we were able to reconfirm with investigators that outcome data included in our analysis were complete we found a pooled RR of 0.40 (95% CrI 0.12 to 0.91), in remaining studies a pooled RR of 0.17 (95% CrI 0.02 to 0.60; p for interaction 0.17).
Table 4. Pooled relative risks of primary and secondary outcomes found in studies satisfying all 5 methodological criteria.
| Outcome | RR (95% CrI) | τ2 |
| Ischaemic Stroke | 0.65 (0.12−3.05) | 0.15 |
| ICH | 0.00 (0.00−0.47) | 0.18 |
| TIA | 0.73 (0.12−3.97) | 0.18 |
| Death | 1.46 (0.17−10.79) | 0.26 |
| Ischaemic Stroke or ICH | 0.52 (0.10−2.16) | 0.16 |
| Ischaemic Stroke or TIA | 0.79 (0.17−3.31) | 0.19 |
| Ischaemic Stroke, ICH or TIA | 0.68 (0.14−2.98) | 0.21 |
Primary endpoint.
ICH = intracranial haemorrhage; TIA = transient ischaemic attack.
Table 5 shows a comparison of results of our and previous meta-analyses [10], [11]. Engelter and Lyrer used a fixed-effect model to derive pooled Peto odds ratios. They found clinically relevant, but non-significant reductions in the odds of stroke (OR 0.63, 95% CI 0.21 to 1.86) and intracranial haemorrhage (OR 0.25, 95% CI 0.02 to 3.36), but a clinically relevant trend towards higher overall mortality associated with antiplatelets as compared with anticoagulants (OR 2.02, 95% CI 0.62 to 6.60). Our re-analysis of Engelter and Lyrer's data using our Bayesian random-effects model (Table 5, top) shows a pronounced, albeit non-significant 55% relative reduction of stroke and a pronounced, statistically significant 100% relative risk reduction of intracranial haemorrhage. The 40% relative risk increase of death was non-significant and less pronounced than reported by Engelter and Lyrer [11] .The 20 intersecting studies in 1109 patients included in their and in our meta-analysis were less beneficial for antiplatelets (RR of stroke 0.64, 95% CrI 0.18 to 2.14) than the 16 studies in 176 patients included only in their meta-analysis (RR 0.45, 95% CrI 0.15 to 1.41) and the 17 studies in 882 patients included only in our meta-analysis (RR 0.19, 95% CrI 0.02 to 0.97, Table 5, middle). Menon et al used a fixed-effect model, which was not further specified. They found a small risk difference of −0.01 for stroke (95% CI −0.06 to 0.04), which was slightly in favour of antiplatelets, and a more pronounced risk difference in opposite direction of 0.05 in favour of anticoagulants for the composite of stroke or TIA (95% CI −0.01 to 0.11). In our re-analysis of their data (Table 5, top), we also found opposite directions of effects. However, on a relative risk scale, these opposite effects had the same magnitude: a 49% relative risk reduction for stroke and a 48% relative risk increase for the composite of stroke or TIA associated with antiplatelets, with considerable imprecision of both estimates, as evidenced by wide 95% credibility intervals. The 18 intersecting studies in 553 patients included in their and our meta-analysis (RR of stroke 0.48, 95% CrI 0.10 to 1.76) and the 16 studies in 209 patients included only in their meta-analysis (RR 0.65, 95% CrI 0.02 to 13.72) were less beneficial for antiplatelets than the 19 studies in 1438 patients included only in our meta-analysis (0.15, 95% CrI 0.02 to 0.70, Table 5, bottom).
Table 5. Influence of in- or exclusion of studies on estimated effects.
| RR (95% CrI) | ||||||
| Number of studies | Number of patients | Ischaemic Stroke | ICH | Death | Ischaemic Stroke or TIA | |
| Our meta-analysis, all included studies | 37 | 1991 | 0.29 (0.08−0.77) | 0.00 (0.00−0.05) | 0.69 (0.23−1.99) | 0.59 (0.19−1.45) |
| Engelter et al's meta-analysis, all included studies | 36 | 1285 | 0.45 (0.15−1.41) | 0.00 (0.00−0.36) | 1.40 (0.46−3.79) | n/a |
| Menon et al's meta-analysis, all included studies | 34 | 762 | 0.51 (0.13−1.62) | n/a | n/a | 1.48 (0.41−4.33) |
| Engelter et al's versus our meta-analysis | ||||||
| Studies included in Engelter et al's and our meta-analysis | 20 | 1109 | 0.64 (0.18−2.14) | 0.00 (0.00−0.15) | 1.80 (0.38−9.15) | n/a |
| Studies included in Engelter et al's but not in our meta-analysis | 16 | 176 | 0.45 (0.15−1.41) | 0.00 (0.00−26.68) | 0.96 (0.13−4.32) | n/a |
| Studies included in our, but not in Engelter et al's meta-analysis | 17 | 882 | 0.19 (0.02−0.97) | 0.00 (0.001−0.003) | 0.33 (0.03−1.80) | n/a |
| Menon et al's versus our meta-analysis | ||||||
| Studies included in Menon et al's and our meta-analysis | 18 | 553 | 0.48 (0.10−1.76) | n/a | n/a | 2.00 (0.44−7.52) |
| Studies included in Menon et al's but not in our meta-analysis | 16 | 209 | 0.65 (0.02−13.72) | n/a | n/a | 0.76 (0.10−4.05) |
| Studies included in our, but not in Menon et al's meta-analysis | 19 | 1438 | 0.15 (0.02−0.70) | n/a | n/a | 0.41 (0.14−1.03) |
Outcomes included if reported in at least two out of the three available meta-analyses.
ICH = intracranial haemorrhage; TIA = transient ischaemic attack.
Sensitivity analyses using different statistical methods are reported in Appendix S4. For the primary composite endpoint of stroke, intracranial haemorrhage or death, we found point estimates and precision much the same for all five methods used. This was also the case for stroke, death, and the composite of stroke or intracranial haemorrhage. For remaining outcomes, there were some differences in point estimates or precision, but overlapping credibility intervals suggested compatibility of estimates.
Discussion
In this meta-analysis of 37 observational studies comparing antiplatelets with anticoagulants in 1991 patients with cervical artery dissection, we found evidence to suggest a clinically relevant advantage of antiplatelets over anticoagulants on the primary outcome (composite of ischaemic stroke, intracranial haemorrhage or death), and 4 out of 7 secondary outcomes. When we stratified according to components of study quality, we found the benefit of antiplatelets considerably less pronounced in studies of higher methodological quality. Tests for interaction between estimated relative risks and study characteristics formally reached statistical significance for prospective study design and balanced group size, and showed a statistical trend for consecutive recruitment of patients and analysis in accordance with the intention-to-treat principle. In an analysis restricted to studies, which satisfied all pre-specified methodological criteria, credibility intervals were wide for all outcomes, except for intracranial haemorrhage, and were compatible with both, a substantial advantage or disadvantage of antiplatelets over anticoagulants. Furthermore, we stratified analyses according to the site of dissection, i.e. carotid or vertebral artery. This analysis showed similar results in the two groups, even though tests for interaction between the site of dissection and the estimated treatment effect were positive for ischaemic stroke and the composite of ischaemic stroke or intracranial haemorrhage. None of the numerous analyses provided robust evidence that anticoagulants are more beneficial than antiplatelets in patients with cervical artery dissection. The risk of intracranial hemorrhage was lower in the antiplatelet group and may be considered to contradict contemporary trials, which found aspirin in patients with atrial fibrillation not safer than warfarin [62], [63]. This apparent contradiction may be explained by the characteristics of included patients (age, comorbidity and severity of stroke) and timing of treatment initiation (immediate versus delayed): patients with cervical artery dissection are typically younger and have less comorbid conditions than patients with atrial fibrillation at risk of stroke considered for antiplatelet treatment, but typically experience severe strokes with large brain tissue infarction. If treatment is initiated immediately, these patients may be more likely to suffer intracranial haemorrhage with anticoagulation as compared to antiplatelet treatment [8]. This notion is in accordance with current guidelines, which recommend against full-dose anticoagulation in patients with acute ischaemic stroke [64], [65].
In our view, the major strength of this study is the use of Bayesian techniques to address the challenge of studies with scarce event data and studies with imbalanced sizes of treatment groups [21]. The major limitation is the complete lack of randomised trials comparing antiplatelets and anticoagulants in patients with cervical dissection and the variation in methodological quality of the observational studies included. We addressed this by performing analyses stratified according to methodological quality and found evidence for overestimations of the benefit of antiplatelets in studies of lower methodological quality. In an analysis restricted to studies of higher methodological quality, the possible advantage of antiplatelets over anticoagulants was less obvious than in the main analysis. Observational studies may be subject to confounding by indication: patients with extensive stroke at baseline and substantially increased risk of subsequent intracranial haemorrhage may be more likely to receive antiplatelets than anticoagulants [66], [67]. These patients typically have a poor prognosis and may die early after initiation of antithrombotic treatment. We were unable to formally compare stroke severity between patients with antiplatelet and anticoagulant treatment at baseline because of the low quality of reporting, but attempted to address this indirectly by performing an additional analysis of mortality data stratified according to time of death. During the first seven days after treatment initiation, we found a trend towards more deaths in the antiplatelet group, whereas a trend into the opposite direction was observed for the subsequent period up to 3 months. This observation indeed suggests confounding by indication, which may have introduced bias against antiplatelets, although a statistical test for interaction was negative. Conversely, patients may have been more likely to receive antiplatelets if they had lower degree stenoses of cerebral arteries or few clinical symptoms only [57]. This could have biased results in favour of antiplatelets, but again, the lack of information on baseline characteristics prevented us from addressing this formally. Results from adjusted analysis were available only for one study [57], which used the presence or absence of cerebral ischemic symptoms as covariate. The adjusted estimate for the composite of ischemic stroke, TIA or transient monocular blindness or retinal infarction showed a trend in favour of antiplatelets (OR 0.38, 95% CI 0.08 to 1.67) [57]. An alternative attempt to address comparability of groups was the classification of studies according to the balance in the size of treatment groups. Some might argue that this criterion is not obviously related to bias. We pre-specified it as a proxy for pronounced differences in treatment indication in a specific study. For example, in the study by Dziewas et al, only 7% of patients (9 out of 122) [19] had received antiplatelets as opposed to 64% in the study by Arauz et al (83 out of 130) [18]. We consider it more likely in the first than in the second study that pronounced differences in indication for treatment introduced bias: the 7% of patients who received antiplatelets are likely to be highly selected and not comparable with the remaining 93% who received anticoagulation. We found that this approach towards addressing comparability of groups was more suitable than a direct comparison of relevant patient characteristics at baseline between groups because of the limited quality of reporting of included studies. A further source of bias is the potential for selective reporting of outcomes [68] ,which may have biased results in favour of either treatment. We addressed this in a post hoc analysis, distinguishing between studies, for which we were able to reconfirm with authors that outcome data included in our analysis were complete, and studies for which this was not the case. There was little evidence for a difference in estimated effects, and studies with complete outcome data showed a robust advantage of antiplatelets.
We were also unable to address the fact that safety and efficacy of anticoagulation is associated with control of international normalized ratio since included studies did not provide the necessary information [69]. Consequently, we cannot exclude that patients with appropriate control of their international normalized ratio will fair better than patients included in our study. Another limitation may concern the exclusion of patients with a traumatic dissection, as classification into traumatic or spontaneous form may be arbitrary in some cases. Furthermore, the state of the dissected artery (stenosis vs. occlusion), which may be associated with both, the choice of antithrombotic treatment and prognosis, was not reported in most studies. Finally, the degree of heterogeneity between studies observed for three outcomes (transitory ischaemic attacks, and two composite endpoints including transitory ischaemic attacks as one of their components) was high. We identified one study to contribute most to heterogeneity [19]: it was small, had unbalanced group sizes and an unusually high rate of transitory ischaemic attacks in patients treated with antiplatelets. We performed a sensitivity analysis after exclusion of this study and found heterogeneity decreased, but emphasise the purely explorative character of this analysis along with the fact that remaining heterogeneity between studies was still moderate.
Three meta-analyses have been published so far [9]–[11]. All used frequentist methods for statistical analyses. The original Cochrane Review and its recent update used a fixed effect model to derive pooled Peto odd ratios excluding studies with zero events in both groups [9], [11], [70]. In view of the considerable imbalances in group sizes, this approach may have introduced bias in favour of either treatment. The Cochrane Review included only studies reporting on patients with cervical carotid artery dissection, whereas we included also patients with vertebral artery dissection. When analyzing the primary outcome in our study, we found similar relative risks for carotid (RR 0.14, 95% CrI 0.03 to 0.50) and vertebral dissections (RR 0.24, 95% CrI 0.04 to 0.97), which suggests that a combined analysis of the two sites of dissections is viable. Another important difference is the choice of primary outcomes, which were overall mortality and the composite of death or disability in the Cochrane Review [9], [11]. For death, they found a pooled odds ratio of 2.02 (95% confidence interval 0.62 to 6.60), whereas our pooled relative risk was 0.69 (95% CrI 0.23 to 1.99). This difference in pooled estimates may be explained by chance alone, differences in study selection or differences in the analytical approaches used. Differences in study selection mainly occurred because of more stringent selection criteria in our study, requiring 3-month follow-up data. This follow-up duration was chosen in view of the frequent change from anticoagulants to antiplatelets in routine clinical practice that typically occurs after completion of the first three months of treatment. Other reasons for differing study selection include a more up to date literature search and the discussed inclusion of both, patients with carotid and vertebral dissection, even though we deem it unlikely that differences in results between the Cochrane Review and our study can be fully explained by dissection site. Re-analyses of data included in the Cochrane Review and our meta-analysis reported in Table 5 in comparison with original results [11] suggested that the differences between their and our results could be explained by both, differences in statistical methods and differences in study identification and selection. We emphasise, however, that widely overlapping uncertainty intervals indicate that our results for stroke, intracranial haemorrhage and death are compatible with both, the Bayesian re-analysis of the data of the Cochrane Review and the original results published of the Cochrane Review. We did not analyse the composite of death or disability, since disability was typically not reported at 3 months, but it is obvious that results on this long term outcome (odds ratio of 1.77 in favour of anticoagulants, 95% CI 0.98 to 3.22) reported in Cochrane Review are in opposition to the majority of our short to midterm results. This discrepancy could be explained by the different nature of outcomes, but may also be related to challenges in interpreting longer term data of included observational studies: clinical practice frequently involves a switch from anticoagulation to antiplatelets after 3 to 6 months, thus the true association of outcomes with type of antithrombotic treatment is difficult to determine after this period.
Menon and colleagues used a fixed effect model to derive risk differences and included studies with zero events in both groups [10]. They observed no relevant difference between antiplatelets and anticoagulants. This is not surprising because about half of the studies included had null events in both groups with an estimated risk difference of zero [10]. Their analytical approach used gave undue weight to these studies and is likely to have biased results towards underestimating potential differences [12]. In addition, they confined the follow-up duration to one month, which will have led to the exclusion of clinical events and reduced statistical power as compared with our analysis. Re-analyses of data included in Menon et al's and our meta-analysis (reported in Table 5) in comparison with original results [10] suggested that the differences can be explained by differences in statistical methods, study identification and selection, even though the impact of study identification and selection was more pronounced, with a nearly threefold increase in the number of patients in our as compared with Menon et al's analysis. Studies included either in the Cochrane Review [11] or in the meta-analysis by Menon et al [10], which were excluded from our analysis typically because of short follow-up duration or unclear reporting of type of treatment or outcome that could be resolved with authors, were small and had only a small number of primary outcome events.
Currently, two small-scale randomised trials comparing anticoagulants and antiplatelets in patients with cervical artery dissection are ongoing. The Cervical Artery Dissection in Stroke Study (CADISS) aims at including 250 patients. 215 patients have been randomised by 3rd December 2012 [71]. The other trial, a pilot study in 20 patients, has completed recruitment [72]. Both trials are pilot studies, not set up to formally compare antiplatelets with anticoagulants in terms of patient-relevant clinical outcomes.
Results of our overall analysis suggest an advantage of antiplatelets over anticoagulants on nearly all outcomes, which contradict the current preferential use of anticoagulants in routine clinical practice for patients with cervical artery dissection. Stratified analyses according to methodological quality showed less pronounced advantages of antiplatelets in studies of higher methodological quality, with point estimates nearer the line of no difference at 1 and credibility intervals compatible with both relevant advantages and disadvantages of antiplatelets over anticoagulants. This suggests equipoise between the two types of treatments and calls for a carefully designed, adequately powered randomised multicenter trial. A sample size of 2100 patients per group will provide 80% power at a two-sided alpha of 0.05 to detect a 30% relative risk reduction in the primary composite outcome of stroke, intracranial haemorrhage or death from 7% in patients receiving anticoagulants to 4.9% in patients receiving antiplatelets. Performing such a trial is difficult, time-consuming and costly. Cervical artery dissection is a typical example of an acute rare condition where, globally, it would be possible to recruit about 4000 patients to conduct a properly powered randomised trial within one or two years. However, given that each center would contribute only 1–2 patients per year, literally thousands of centers would be required, which makes the costs of initiation and logistics of such a trial prohibitive. Novel approaches might be needed, with an international trials consortium performing a series of trials in patients with different types of rare conditions, with standard procedures, common logistics, and simplified requirements for approval by local research ethics committees for the entire series of trials. For now, considering that discrepancies between randomised trials and observational studies may be less pronounced than theoretically expected [73], we call for carefully conducted prospective cohort studies to fill the evidence gap until randomised evidence becomes available.
Oral anticoagulants are widely used in routine clinical practice in patients with cervical artery dissection. They are about 15 times more expensive than aspirin [74], the classical antiplatelet used in clinical practice for the treatment of cervical artery dissection, require a higher degree of compliance, dependent on frequent laboratory testing and carry a higher risk of intracranial haemorrhage than antiplatelets. The pharmacokinetic profile of oral anticoagulants is variable and there are multiple interactions with drugs and food, which frequently result in poor control of the INR [75]. As compared to conventional Vitamin K antagonists, anticoagulation with the novel factor Xa or thrombin inhibitors were found more effective in stroke prevention in patients with atrial fibrillation and more practical for handling.76,77 The safety and effectiveness of these new anticoagulants in patients with cervical artery dissection will need to be investigated in randomised trials. Considering these practical and theoretical disadvantages of anticoagulants and our meta-analysis, which clearly provides no evidence for a superiority of anticoagulants over antiplatelets, even pointing towards a harmful effect of anticoagulants, we question the preferential use of anticoagulants as a first line treatment in patients with cervical artery dissection and conclude that antiplatelets should be given precedence instead, unless results of an adequately powered randomised trial suggest the opposite.
Supporting Information
Literature search strategy.
(DOCX)
Review Protocol.
(DOCX)
Extended description of statistical methods.
(DOCX)
Different approaches for estimating summary effect.
(DOC)
Funding Statement
Hakan Sarikaya was supported by a research grant from Swiss National Foundation (SNF). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Bogousslavsky J, Pierre P (1992) Ischemic stroke in patients under age 45. Neurol Clin 10: 113–124. [PubMed] [Google Scholar]
- 2. Leys D, Bandu L, Henon H, Lucas C, Mounier-Vehier F, et al. (2002) Clinical outcome in 287 consecutive young adults (15 to 45 years) with ischemic stroke. Neurology 59: 26–33. [DOI] [PubMed] [Google Scholar]
- 3. Nedeltchev K, der Maur TA, Georgiadis D, Arnold M, Caso V, et al. (2005) Ischaemic stroke in young adults: predictors of outcome and recurrence. J Neurol Neurosurg Psychiatry 76: 191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fischer U, Ledermann I, Nedeltchev K, Meier N, Gralla J, et al. (2009) Quality of life in survivors after cervical artery dissection. J Neurol 256: 443–449. [DOI] [PubMed] [Google Scholar]
- 5. Arnold M, Kappeler L, Georgiadis D, Berthet K, Keserue B, et al. (2006) Gender differences in spontaneous cervical artery dissection. Neurology 67: 1050–1052. [DOI] [PubMed] [Google Scholar]
- 6. Benninger DH, Georgiadis D, Kremer C, Studer A, Nedeltchev K, et al. (2004) Mechanism of ischemic infarct in spontaneous carotid dissection. Stroke 35: 482–485. [DOI] [PubMed] [Google Scholar]
- 7. Srinivasan J, Newell DW, Sturzenegger M, Mayberg MR, Winn HR (1996) Transcranial Doppler in the evaluation of internal carotid artery dissection. Stroke 27: 1226–1230. [DOI] [PubMed] [Google Scholar]
- 8. The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. International Stroke Trial Collaborative Group. Lancet 349: 1569–1581. [PubMed] [Google Scholar]
- 9.Lyrer P, Engelter S (2003) Antithrombotic drugs for carotid artery dissection. Cochrane Database of Systematic Reviews: CD000255. [DOI] [PubMed]
- 10. Menon R, Kerry S, Norris JW, Markus HS (2008) Treatment of cervical artery dissection: a systematic review and meta-analysis. Journal of Neurology, Neurosurgery & Psychiatry 79: 1122–1127. [DOI] [PubMed] [Google Scholar]
- 11.Lyrer P, Engelter S (2010) Antithrombotic drugs for carotid artery dissection. Cochrane Database of Systematic Reviews: CD000255. [DOI] [PubMed]
- 12. Mulrow CD, Cornell J, Localio AR (2007) Rosiglitazone: a thunderstorm from scarce and fragile data. Ann Intern Med 147: 585–587. [DOI] [PubMed] [Google Scholar]
- 13. Diamond GA, Bax L, Kaul S (2007) Uncertain effects of rosiglitazone on the risk for myocardial infarction and cardiovascular death. Ann Intern Med 147: 578–581. [DOI] [PubMed] [Google Scholar]
- 14. Biffl WL, Moore EE, Offner PJ, Brega KE, Franciose RJ, et al. (1999) Blunt carotid arterial injuries: implications of a new grading scale. Journal of Trauma-Injury Infection & Critical Care 47: 845–853. [DOI] [PubMed] [Google Scholar]
- 15. Davis JW, Holbrook TL, Hoyt DB, Mackersie RC, Field TO Jr, et al. (1990) Blunt carotid artery dissection: incidence, associated injuries, screening, and treatment. Journal of Trauma-Injury Infection & Critical Care 30: 1514–1517. [PubMed] [Google Scholar]
- 16. Caso V, Paciaroni M, Bogousslavsky J (2005) Environmental factors and cervical artery dissection. Front Neurol Neurosci 20: 44–53. [DOI] [PubMed] [Google Scholar]
- 17. Nedeltchev K, Baumgartner RW (2005) Traumatic cervical artery dissection. Frontiers of Neurology & Neuroscience 20: 54–63. [DOI] [PubMed] [Google Scholar]
- 18. Arauz A, Hoyos L, Espinoza C, Cantu C, Barinagarrementeria F, et al. (2006) Dissection of cervical arteries: Long-term follow-up study of 130 consecutive cases. Cerebrovascular Diseases 22: 150–154. [DOI] [PubMed] [Google Scholar]
- 19. Dziewas R, Konrad C, Drager B, Evers S, Besselmann M, et al. (2003) Cervical artery dissection – clinical features, risk factors, therapy and outcome in 126 patients. Journal of Neurology 250: 1179–1184. [DOI] [PubMed] [Google Scholar]
- 20. Smith TC, Spiegelhalter DJ, Thomas A (1995) Bayesian approaches to random-effects meta-analysis: a comparative study. Stat Med 14: 2685–2699. [DOI] [PubMed] [Google Scholar]
- 21. Warn DE, Thompson SG, Spiegelhalter DJ (2002) Bayesian random effects meta-analysis of trials with binary outcomes: methods for the absolute risk difference and relative risk scales. Stat Med 21: 1601–1623. [DOI] [PubMed] [Google Scholar]
- 22.Spiegelhalter D, Abrams K, Myles J (2004) Bayesian approaches to clinical trials and healthcare evaluation. Chichester: John Wiley & Sons.
- 23. Stettler C, Allemann S, Wandel S, Kastrati A, Morice MC, et al. (2008) Drug eluting and bare metal stents in people with and without diabetes: collaborative network meta-analysis. BMJ 337: a1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Slavin RE (1986) Best-Evidence Synthesis: An Alternative to Meta-Analytic and Traditional Reviews. EDUCATIONAL RESEARCHER 15: 5–11. [Google Scholar]
- 25. Lunn DJ, Thomas A, Best N, Spiegelhalter D (2000) WinBUGS – A Bayesian modelling framework: Concepts, structure, and extensibility. Statistics and Computing 10: 325–337. [Google Scholar]
- 26. Lunn D, Spiegelhalter D, Thomas A, Best N (2009) The BUGS project: Evolution, critique and future directions. Stat Med 28: 3049–3067. [DOI] [PubMed] [Google Scholar]
- 27. Fisher CM, Ojemann RG, Roberson GH (1978) Spontaneous Dissection of Cervico-Cerebral Arteries. Canadian Journal of Neurological Sciences 5: 9–19. [PubMed] [Google Scholar]
- 28. Luken MG 3rd, Ascherl GF Jr, Correll JW, Hilal SK (1979) Spontaneous dissecting aneurysms of the extracranial internal carotid artery. Clin Neurosurg 26: 353–375. [DOI] [PubMed] [Google Scholar]
- 29. Sellier N, Chiras J, Benhamou M, Bories J (1983) Spontaneous dissection of the internal carotid artery. Clinical, radiological and evolutive features. A study of 46 cases. Journal of Neuroradiology 10: 243–259. [PubMed] [Google Scholar]
- 30. Vanneste JA, Davies G (1984) Spontaneous dissection of the cervical internal carotid artery. Clin Neurol Neurosurg 86: 307–314. [DOI] [PubMed] [Google Scholar]
- 31. Mokri B, Sundt TM, Houser OW, Piepgras DG (1986) Spontaneous Dissection of the Cervical Internal Carotid-Artery. Annals of Neurology 19: 126–138. [DOI] [PubMed] [Google Scholar]
- 32. Bogousslavsky J, Despland PA, Regli F (1987) Spontaneous carotid dissection with acute stroke. Archives of Neurology 44: 137–140. [DOI] [PubMed] [Google Scholar]
- 33. Marx A, Messing B, Storch B, Busse O (1987) [Spontaneous dissection of arteries supplying the brain]. Nervenarzt 58: 8–18. [PubMed] [Google Scholar]
- 34. Mas JL, Bousser MG, Hasboun D, Laplane D (1987) Extracranial vertebral artery dissections: a review of 13 cases. Stroke 18: 1037–1047. [DOI] [PubMed] [Google Scholar]
- 35. Landre E, Roux FX, Cioloca C (1987) Spontaneous dissection of the extracranial internal carotid artery. Therapeutic aspects. Presse Medicale 16: 1273–1276. [PubMed] [Google Scholar]
- 36. Mokri B, Houser OW, Sandok BA, Piepgras DG (1988) Spontaneous dissections of the vertebral arteries. Neurology 38: 880–885. [DOI] [PubMed] [Google Scholar]
- 37. De Bray JM, Dubas F, Joseph PA, Causeret H, Pasquier JP, et al. (1989) Ultrasonic study of dissections of the internal carotid artery. 22 cases. Revue Neurologique 145: 702–709. [PubMed] [Google Scholar]
- 38. Eljamel MS, Humphrey PR, Shaw MD (1990) Dissection of the cervical internal carotid artery. The role of Doppler/Duplex studies and conservative management. Journal of Neurology, Neurosurgery & Psychiatry 53: 379–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Schievink WI, Limburg M (1990) Dissection of the cervical arteries as a cause of cerebral ischaemia and cranial nerve dysfunction. Nederlands Tijdschrift voor Geneeskunde 134: 1843–1848. [PubMed] [Google Scholar]
- 40. Ast G, Woimant F, Georges B, Laurian C, Haguenau M (1993) Spontaneous dissection of the internal carotid artery in 68 patients. European Journal of Medicine 2: 466–472. [PubMed] [Google Scholar]
- 41. Landini G, Cordopatri F, Scarti L, Spolveri S, Pennati P, et al. (1996) Dissection of the epiaortic arteries: An emerging pathology as a cause of focal cerebral ischemia. Evaluation of 7 cases. Annali Italiani di Medicina Interna 11: 12–16. [PubMed] [Google Scholar]
- 42. Pego R, Marey J, Lopez-Facal MS, Marin-Sanchez M (1996) [Eight cases of extracranial vertebral artery dissection]. Revista de Neurologia 24: 172–175. [PubMed] [Google Scholar]
- 43. Plaza I, Diez-Tejedor E, Lara M, Barreiro P (1996) [Spontaneous dissection of the vertebral artery]. Revista de Neurologia 24: 163–171. [PubMed] [Google Scholar]
- 44. de Bray JM, Penisson-Besnier I, Dubas F, Emile J (1997) Extracranial and intracranial vertebrobasilar dissections: diagnosis and prognosis. Journal of Neurology, Neurosurgery & Psychiatry 63: 46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Biousse V, Schaison M, Touboul PJ, D'Anglejan-Chatillon J, Bousser MG (1998) Ischemic optic neuropathy associated with internal carotid artery dissection. Arch Neurol 55: 715–719. [DOI] [PubMed] [Google Scholar]
- 46. Han DH, Kwon OK, Oh CW (1998) Clinical characteristics of vertebrobasilar artery dissection. Neurologia Medico-Chirurgica 38 Suppl: 107–113 [DOI] [PubMed] [Google Scholar]
- 47. Engelter ST, Lyrer PA, Kirsch EC, Steck AJ (2000) Long-term follow-up after extracranial internal carotid artery dissection. European Neurology 44: 199–204. [DOI] [PubMed] [Google Scholar]
- 48. Beletsky V, Nadareishvili Z, Lynch J, Shuaib A, Woolfenden A, et al. (2003) Cervical arterial dissection: time for a therapeutic trial? Stroke 34: 2856–2860. [DOI] [PubMed] [Google Scholar]
- 49. Touze E, Gauvrit JY, Moulin T, Meder JF, Bracard S, et al. (2003) Risk of stroke and recurrent dissection after a cervical artery dissection: a multicenter study. Neurology 61: 1347–1351. [DOI] [PubMed] [Google Scholar]
- 50. Caso V, Paciaroni M, Corea F, Hamam M, Milia P, et al. (2004) Recanalization of cervical artery dissection: influencing factors and role in neurological outcome. Cerebrovascular Diseases 17: 93–97. [DOI] [PubMed] [Google Scholar]
- 51. Campos CR, Evaristo EF, Yamamoto FI, Puglia Jr P, Tavares Lucato L, et al. (2004) Spontaneous cervical carotid and vertebral arteries dissection – Study of 48 patients. Arquivos de Neuro-Psiquiatria 62: 492–498. [DOI] [PubMed] [Google Scholar]
- 52. Arnold M, Bousser MG, Fahrni G, Fischer U, Georgiadis D, et al. (2006) Vertebral artery dissection: presenting findings and predictors of outcome. [Erratum appears in Stroke. 2007 Jan;38(1):208]. Stroke 37: 2499–2503. [DOI] [PubMed] [Google Scholar]
- 53. de Bray JM, Marc G, Pautot V, Vielle B, Pasco A, et al. (2007) Fibromuscular dysplasia may herald symptomatic recurrence of cervical artery dissection. Cerebrovascular Diseases 23: 448–452. [DOI] [PubMed] [Google Scholar]
- 54. Nyberg J, Olsson T, Malm J (2007) [Carotid and vertebral artery dissection a common cause of stroke among younger persons. Minor trauma a precipitating factor in more than fifty percent according to a retrospective study]. Lakartidningen 104: 24–28. [PubMed] [Google Scholar]
- 55. Simoes R, Biscoito L, Parreira E, Pinto AN (2007) A comparison study of cervical artery dissections – Hospital series of 61 patients. Sinapse 7: 36–43. [Google Scholar]
- 56. Rigamonti A, Iurlaro S, Reganati P, Zilioli A, Agostoni E (2008) Cluster headache and internal carotid artery dissection: two cases and review of the literature. Headache 48: 467–470. [DOI] [PubMed] [Google Scholar]
- 57. Georgiadis D, Arnold M, von Buedingen HC, Valko P, Sarikaya H, et al. (2009) Aspirin vs anticoagulation in carotid artery dissection: a study of 298 patients. Neurology 72: 1810–1815. [DOI] [PubMed] [Google Scholar]
- 58. Metso TM, Metso AJ, Salonen O, Haapaniemi E, Putaala J, et al. (2009) Adult cervicocerebral artery dissection: a single-center study of 301 Finnish patients. European Journal of Neurology 16: 656–661. [DOI] [PubMed] [Google Scholar]
- 59. Arauz A, Marquez JM, Artigas C, Balderrama J, Orrego H (2010) Recanalization of vertebral artery dissection. Stroke 41: 717–721. [DOI] [PubMed] [Google Scholar]
- 60. Divjak I, Slankamenac P, Jovicevic M, Zikic TR, Prokin AL, et al. (2011) A case series of 22 patients with internal carotid artery dissection. Med Pregl 64: 575–578. [PubMed] [Google Scholar]
- 61. Kennedy F, Lanfranconi S, Hicks C, Reid J, Gompertz P, et al. (2012) Antiplatelets vs anticoagulation for dissection: CADISS nonrandomized arm and meta-analysis. Neurology 79: 686–689. [DOI] [PubMed] [Google Scholar]
- 62. Mant J, Hobbs FD, Fletcher K, Roalfe A, Fitzmaurice D, et al. (2007) Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation (the Birmingham Atrial Fibrillation Treatment of the Aged Study, BAFTA): a randomised controlled trial. Lancet 370: 493–503. [DOI] [PubMed] [Google Scholar]
- 63. Rash A, Downes T, Portner R, Yeo WW, Morgan N, et al. (2007) A randomised controlled trial of warfarin versus aspirin for stroke prevention in octogenarians with atrial fibrillation (WASPO). Age Ageing 36: 151–156. [DOI] [PubMed] [Google Scholar]
- 64. Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, et al. (2007) Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke 38: 1655–1711. [DOI] [PubMed] [Google Scholar]
- 65. Albers GW, Amarenco P, Easton JD, Sacco RL, Teal P (2008) Antithrombotic and thrombolytic therapy for ischemic stroke: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 133: 630S–669S. [DOI] [PubMed] [Google Scholar]
- 66. Engelter ST, Brandt T, Debette S, Caso V, Lichy C, et al. (2007) Antiplatelets versus anticoagulation in cervical artery dissection. Stroke 38: 2605–2611. [DOI] [PubMed] [Google Scholar]
- 67. Low molecular weight heparinoid, ORG 10172 (danaparoid), and outcome after acute ischemic stroke: a randomized controlled trial. The Publications Committee for the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) Investigators. JAMA 279: 1265–1272. [PubMed] [Google Scholar]
- 68. Chan AW, Hrobjartsson A, Haahr MT, Gotzsche PC, Altman DG (2004) Empirical evidence for selective reporting of outcomes in randomized trials: comparison of protocols to published articles. JAMA 291: 2457–2465. [DOI] [PubMed] [Google Scholar]
- 69. Wan Y, Heneghan C, Perera R, Roberts N, Hollowell J, et al. (2008) Anticoagulation control and prediction of adverse events in patients with atrial fibrillation: a systematic review. Circ Cardiovasc Qual Outcomes 1: 84–91. [DOI] [PubMed] [Google Scholar]
- 70. Yusuf S, Peto R, Lewis J, Collins R, Sleight P (1985) Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis 27: 335–371. [DOI] [PubMed] [Google Scholar]
- 71.The CADISS Trial Investigators. Cervical Artery Dissection in Stroke Study. Available: www.dissection.co.uk 24 August 2010.
- 72.Jensen M Pilot Study of Aspirin Versus Warfarin for Cervicocephalic Arterial Dissection. Available: www.clinicaltrials.gov/ct2/show/NCT00265408 24 August 2010.
- 73. Vandenbroucke JP (2011) Why do the results of randomised and observational studies differ? BMJ 343: d7020. [DOI] [PubMed] [Google Scholar]
- 74. Taylor FC, Ebrahim S (2000) Using anticoagulation or aspirin to prevent stroke – Aspirin is the logical choice for non-rheumatic atrial fibrillation. British Medical Journal 320: 1010–1010. [PubMed] [Google Scholar]
- 75. Samsa GP, Matchar DB, Goldstein LB, Bonito AJ, Lux LJ, et al. (2000) Quality of anticoagulation management among patients with atrial fibrillation: results of a review of medical records from 2 communities. Arch Intern Med 160: 967–973. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Literature search strategy.
(DOCX)
Review Protocol.
(DOCX)
Extended description of statistical methods.
(DOCX)
Different approaches for estimating summary effect.
(DOC)