Abstract
Background Posttraumatic arthritides of the radiocarpal joint, secondary to scaphoid nonunion advanced collapse (SNAC), scapholunate advanced collapse (SLAC), or Kienböck disease or in cases of intraarticularmalunion of the distal radius, are classically solved by some type of arthrodesis procedure. Osteochondral grafting provides a possible motion-sparing option that can diminish pain in the active patient.
Description of Technique A chondrocostal graft harvested from the ninth rib was inserted and fixed with a plate in place of the articular defect in cases of a malunited intra-articular distal radius fracture (7 cases) or to replace the proximal pole of the scaphoid in cases of SNAC or SLAC (18 cases). In Kienböck disease, the graft was inserted as a free cartilage spacer (4 cases).
Results Harvesting the graft from the ninth rib had minimal morbidity without pleural injury in the reported series. Graft union was achieved in all cases of fixation. No graft resorption or necrosis were observed on X-ray and magnetic resonance imaging (MRI) evaluation at the longest follow-up of 10 years. Histological analysis performed at the time of plate removal showed the vitality of the graft. Two thirds of the patients had excellent or good results using the Green and O'Brien score.
Conclusions Reconstruction of a partially destroyed articular surface using a costal graft is reliable and provides an alternative option for resurfacing the articular surface with viable cartilage.
Keywords: rib cartilage graft, SNAC, SLAC, Kienböck disease, wrist surgery, interposition and free spacer surgery
Rib cartilage harvested from the osteocartilaginous junction of the eighth rib is part of the classical armamentarium in maxillofacial surgery for reconstructing the concha,1 the mandibular condyle in both adults and children,2,3 the nose, and the trachea.4 More recently, grafts have been used in orthopedics, whether costal cartilage or not, in post-traumatic interphalangeal (PIP) joint injury,5 metacarpal bone and metacarpophalangeal (MCP) joint injury,6 phalangeal joint reconstruction,7,8 and radioscaphoid osteoarthritis (OA).9,10 Currently, osteochondral allografts and cartilage autografts are used in managing osteochondritis of the elbow and knee.11,12,13,14 In addition, although theoretically many graft harvest sites exist (auricle, nasal septum, or costal cartilage), all authors15,16 agree in saying that these three types of cartilage are histologically similar.
In this paper, we will report our experience with the use of costal cartilage grafts in posttraumatic arthritis or cartilage defects for scapholunate advanced collapse (SLAC) wrist, scaphoid nonunion advanced collapse (SNAC), intraarticular malunions of the distal radius, and Kienböck disease.
Surgical Technique
Rib Graft Harvesting
The rib graft harvest procedure is illustrated in Fig. 1.17,18 Through a horizontal incision, the cartilaginous surface of the seventh, eighth, or ninth rib is exposed. The osteochondral junction is easy to identify because of the difference in color. The deep side of the ninth rib is carefully exposed. The graft is harvested along with the perichondrium using a no. 23 scalpel blade to divide the cartilage and an oscillating saw to osteotomize the rib. Positive pressure insufflation is then performed to detect any pleural leaks after harvest. The wound is closed with a drain after repairing the intercostal muscles and the subcutaneous tissue.
Fig. 1.

Harvesting a graft from the ninth rib (from left to right) after identification of the osteochondral junction.
SNAC and SLAC Wrist
In SNAC and SLAC wrist (Figs. 2345),9,10 whether it be nonunion or a scapholunate ligament lesion with osteoarthritis, we have resected the proximal pole of the scaphoid. In SLAC, this is logical because this is the part of the scaphoid that is arthritic. In SNAC, this solution can be criticized because it is the middle and distal parts of the scaphoid that are arthritic. It is critical to resect no more than the proximal two-thirds of the scaphoid in order to be able to attach the osteochondral cartilage graft (the bony part toward the scaphoid and the cartilaginous part toward the radius) using at least two pins. To date, we have not used screw fixation for osteosynthesis. In addition, given the technical difficulty of placing an osteochondral graft, we have at times placed the graft in a perpendicular fashion. Our series consists of 18 patients with a mean age of 47.7 years (range, 26-62 years). There were 12 SNAC cases and 6 SLAC cases. The mean follow-up was 4.1 years (range, 6 months to 10 years). Graft union was observed in 17 of 18 cases at 3 months, without graft resorption. In the case that failed to achieve bone union, there were no clinical consequences. There is potential for osteoarthritis progression within the carpus, but this was not found in our patients at the latest follow-up. The subjective evaluation found 17 patients who were satisfied or very satisfied, with improvement observed compared with the preoperative condition. Using the Green and O'Brien score there were five excellent, ten good, and three fair results.
Fig. 2.
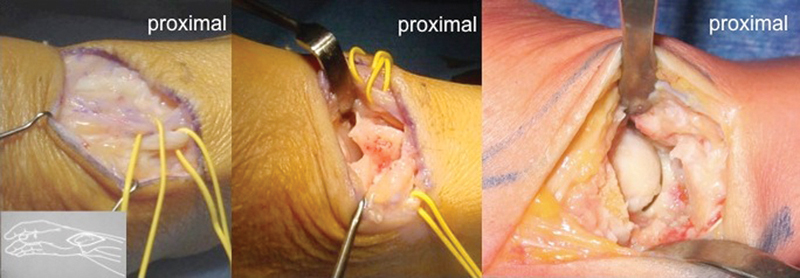
Lateral approach in case of SNAC or SLAC (from left to right): The radial sensory branch is protected while a radial styloidectomy is preformed to improve the access to the proximal pole.
Fig. 3.
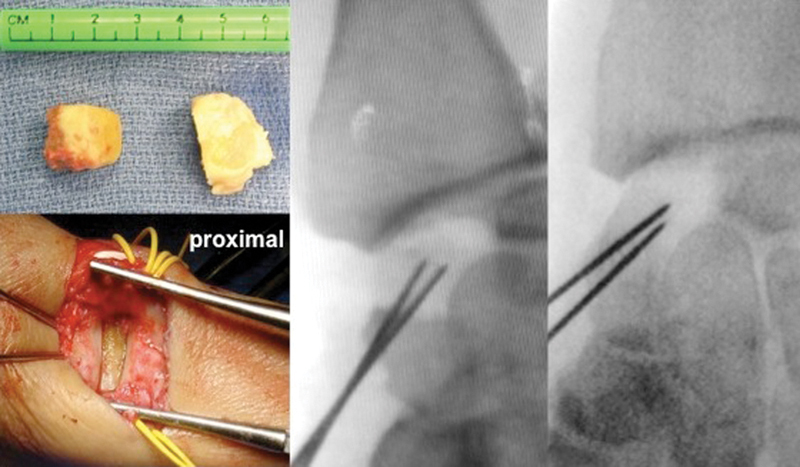
Implantation and fixation of the graft (from left to right). The proximal part of the scaphoid has the same diameter as the graft.
Fig. 4.

SNAC: preoperative and postoperative with the graft at 5 years follow-up in a 46-year-old patient demonstrating preserved radial and ulnar deviation.
Fig. 5.

X-ray at 3 years and 5 years and computed tomography (CT) scan (5 years) of the osteochondral graft in the same patient.
Radiocarpal Osteoarthritis
We have used a cartilage graft for posttraumatic radiocarpal OA (Fig. 6)19 secondary to a malunited distal radius fracture. The osteocartilaginous defect must be perfectly assessed preoperatively on a thin-slice computed tomography (CT) scan. The bony part of the graft is inset in contact with the radius. The cartilaginous part is inset facing the radiocarpal joint and trimmed as needed. We have operated on 6 patients using this technique. They all presented with substantial wrist pain and stiffness. The mean age was 49.2 years (range, 22-72 years). They were reviewed at a mean follow-up of 22.5 months (range, 6-38 months). The mean Herzberg score was 72/100 (range, 54-82). The postoperative Disabilities of the Arm, Shoulder, and Hand (DASH) score was 30.3 (range, 22.5-51.7). In two patients, biopsies were taken during hardware removal, which demonstrated viable grafts. A single case of failure was observed due to lysis of the proximal graft in one female patient who had presented with radiocarpal osteoarthritis secondary to probable sepsis of the scaphoid.
Fig. 6.
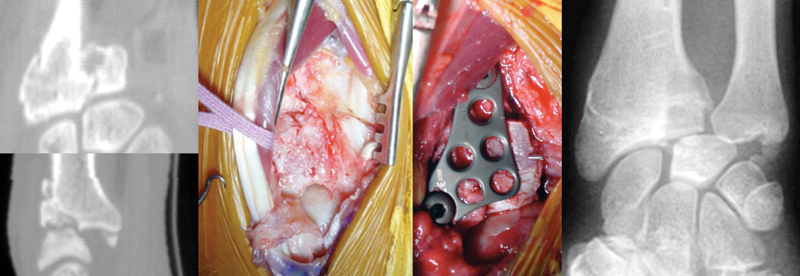
Intraarticular nonunion (from left to right): CT scan view, operative view through a dorsal approach, implantation of the graft fixed by a dorsal plate, and X-ray image at 5 years follow up following hardware removal.
Kienböck Disease
Advanced Kienböck disease with collapse and radiocarpal and midcarpal OA (Lichtman IV) is commonly treated by proximal row resection or by a lunate excision and partial wrist arthrodesis. Between 2007 and 2009, four patients with a mean age of 40 years old (32-51) were treated with lunate excision and a free costochondral autograft from the ninth rib (Fig. 7).20 At a mean follow-up of 27 months (range, 6-36), there was no pain at rest or during daily activities for all patients. The mean DASH score was 6 (range, 5-8). Flexion-extension was108% of contralateral side, and grip strength 83% (range, 70-100) compared with the opposite side. There was no progression of OA radiographically. No complications were reported.
Fig. 7.
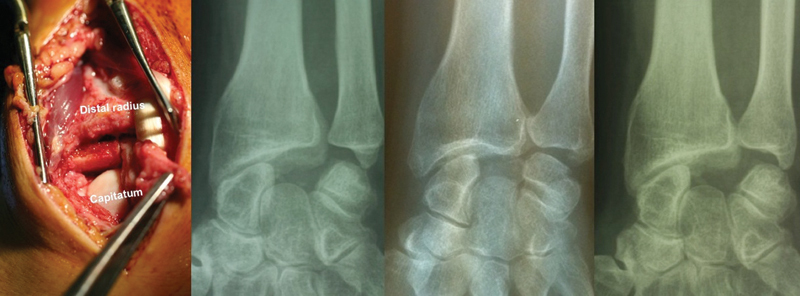
Resection of the lunate in a case of Kienböck disease (from left to right): operative view with the graft X-ray at 2 years of three different cases.
Footnotes
Conflict of Interest None
References
- 1.Brent B Auricular repair with autogenous rib cartilage grafts: two decades of experience with 600 cases Plast Reconstr Surg 1992903355–374., discussion 375-376 [PubMed] [Google Scholar]
- 2.MacIntosh R B, Henny F A. A spectrum of application of autogenous costochondral grafts. J Maxillofac Surg. 1977;5(4):257–267. doi: 10.1016/s0301-0503(77)80120-3. [DOI] [PubMed] [Google Scholar]
- 3.Lindqvist C, Pihakari A, Tasanen A, Hampf G. Autogenous costochondral grafts in temporo-mandibular joint arthroplasty. A survey of 66 arthroplasties in 60 patients. J Maxillofac Surg. 1986;14(3):143–149. doi: 10.1016/s0301-0503(86)80280-6. [DOI] [PubMed] [Google Scholar]
- 4.Ohlsén L, Nordin U. Tracheal reconstruction with perichondrial grafts. Scand J Plast Reconstr Surg. 1976;10(2):135–145. doi: 10.3109/02844317609105201. [DOI] [PubMed] [Google Scholar]
- 5.Hasegawa T, Yamano Y. Arthroplasty of the proximal interphalangeal joint using costal cartilage grafts. J Hand Surg Br. 1992;17(5):583–585. doi: 10.1016/s0266-7681(05)80248-7. [DOI] [PubMed] [Google Scholar]
- 6.Richards R R, Nunley J A. Metacarpal reconstruction with free autogenous cartilage and bone following tumor resection. A case report. Clin Orthop Relat Res. 1984;(190):223–226. [PubMed] [Google Scholar]
- 7.Katsaros J, Milner R, Marshall N J. Perichondrial arthroplasty incorporating costal cartilage. J Hand Surg [Br] 1995;20(2):137–142. doi: 10.1016/s0266-7681(05)80039-7. [DOI] [PubMed] [Google Scholar]
- 8.Skoog T, Johansson S H. The formation of articular cartilage from free perichondrial grafts. Plast Reconstr Surg. 1976;57(1):1–6. doi: 10.1097/00006534-197601000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Lepage D Obert L Clappaz P Hampel C Garbuio P Tropet Y Osteocartilaginous autograft after proximal resection of the scaphoid for radioscaphoid osteoarthritis [in French] Rev Chir Orthop Reparatrice Appar Mot 2005. Jun;914307–313. [DOI] [PubMed] [Google Scholar]
- 10.Sandow M J. Proximal scaphoid costo-osteochondral replacement arthroplasty. J Hand Surg Br. 1998;23(2):201–208. doi: 10.1016/s0266-7681(98)80175-7. [DOI] [PubMed] [Google Scholar]
- 11.Garrett J C. Fresh osteochondral allografts for treatment of articular defects in osteochondritis dissecans of the lateral femoral condyle in adults. Clin Orthop Relat Res. 1994;(303):33–37. [PubMed] [Google Scholar]
- 12.Beaver R J, Mahomed M, Backstein D, Davis A, Zukor D J, Gross A E. Fresh osteochondral allografts for post-traumatic defects in the knee. A survivorship analysis. J Bone Joint Surg Br. 1992;74(1):105–110. doi: 10.1302/0301-620X.74B1.1732235. [DOI] [PubMed] [Google Scholar]
- 13.Convery F R, Meyers M H, Akeson W H. Fresh osteochondral allografting of the femoral condyle. Clin Orthop Relat Res. 1991;(273):139–145. [PubMed] [Google Scholar]
- 14.Sato K, Mio F, Hosoya T, Ito Y. Two cases with osteochondritis dissecans of the capitulum humeri treated with costal osteochondral graft transplantation. J Shoulder Elbow Surg. 2003;12(4):403–407. doi: 10.1016/s1058-2746(02)00045-9. [DOI] [PubMed] [Google Scholar]
- 15.Engkvist O, Skoog V, Pastacaldi P, Yormuk E, Juhlin R. The cartilaginous potential of the perichondrium in rabbit ear and rib. A comparative study in vivo and in vitro. Scand J Plast Reconstr Surg. 1979;13(2):275–280. doi: 10.3109/02844317909013070. [DOI] [PubMed] [Google Scholar]
- 16.Gubisch W, Greulich M, Donath K. Experimental and clinical study on the vitality of orthotopic cartilage transplants. Plast Reconstr Surg. 1995;95(4):663–671. doi: 10.1097/00006534-199504000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Tropet Y, Gallinet D, Lepage D, Gasse N, Obert L. Treatment of trapeziometacarpal osteoarthritis by partial trapeziectomy and costal cartilage autograft. A review of 100 cases. Chir Main. 2012;31(3):145–151. doi: 10.1016/j.main.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Tropet Y Lepage D Gallinet D Obert L Barbuio P Vichard P Articular reconstructions by a costochondral grafting (or osteochondral costal grafting) Bull Acad Natl Med. 2006. Oct;19071439–1456. [PubMed] [Google Scholar]
- 19.Obert L, Lepage D, Sergent P. et al. Post-traumatic malunion of the distal radius treated with autologous costal cartilage graft: a technical note on seven cases. Orthop Traumatol Surg Res. 2011;97(4):430–437. doi: 10.1016/j.otsr.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 20.Huard S, Rochet S, Lepage D, Garbuio P, Obert L. Nouveau traitement de la maladie de Kienböck avancée: remplacement du semilunaire par greffon cartilagineux costal. [in French] Chir Main. 2011;30(3):211–217. doi: 10.1016/j.main.2011.04.005. [DOI] [PubMed] [Google Scholar]


