Abstract
Background Intra-articular fractures of the distal radius represent a therapeutic challenge as compared with the unstable extra-articular fractures. With the recent development of specifically designed internal fixation materials for the distal radius, treatment of these fractures by fragment-specific implants using two or more incisions has been advocated.
Purpose The purpose of this study was to investigate the efficacy of a fixed-angle locking plate applied through a single volar approach in maintaining the radiographic alignment of unstable intra-articular fractures as well as to report the clinical outcomes. We only excluded those with massive comminution, as is discussed in greater detail in the text.
Patients and Methods This is a multicentered, retrospective study involving three hospitals situated in Spain, Switzerland, and the United States. In the period between January 2000 and March 2006, 97 patients with 101 intra-articular distal radius fractures, including 13 volarly displaced and 88 dorsally angulated fractures were analyzed. Over 80% were C2/C3 fractures, based on the AO classification. 16 open fractures were noted.
Results With an average follow-up of 28 months (range 24-70 months), the range of movement of the wrist was very satisfactory, and the mean grip strength was 81% of the opposite wrist. The Disabilities of the Arm, Shoulder, and Hand (DASH) score was 8. The complications rate was < 5%, including loss of reduction in two patients. All fractures healed by 3 months postinjury.
Conclusions Irrespective of the direction and amount of initial displacement, a great majority of intra-articular fractures of the distal radius can be managed with a fixed-angle volar plate through a single volar approach.
Level IV retrospective case series
Keywords: distal radius fractures, volar plate, internal fixation, intra-articular fractures
Intra-articular fractures of the distal radius represent a therapeutic challenge as compared with unstable extra-articular fractures.1 Apart from being more difficult to reduce and stabilize with internal fixation, these injuries frequently result in malunion,2 which may result in a less satisfactory long-term functional outcome, if not anatomically reduced.3 In the past, these fractures were managed with external fixation or a combination of limited open reduction, Kirschner wire (K-wire) augmentation, and bone grafting.4 However, with the recent development of specifically designed locking implants for the distal radius, fragment-specific fixation has emerged as an option.5 Open reduction and internal fixation (ORIF) using volar fixed-angle plates has also shown to be a valid treatment option for unstable, dorsally displaced distal radial fractures.6,7
The purpose of this study was to investigate the efficacy of a fixed angle locking plate applied through a volar approach in maintaining the radiographic alignment of unstable simple intra-articular fractures as well as to report the clinical outcomes.
Patients and Methods
This is a multi-centered retrospective study, conducting in three separate institutions, in three different cities, namely Miami, Florida, USA; Berne, Switzerland; and Barcelona, Spain. 100 patients with 103 intra-articular fractures of the distal radius were treated with internal fixation using the DVR plate (Biomet, Miami, Florida, USA) through a volar flexor carpi radialis (FCR) approach between January 2000 and March 2006. All of the patients gave informed consent for surgical treatment. Three patients were lost to follow-up; thus, we analyzed the remaining 97 patients with 101 distal radius fractures. We excluded all distal radius fractures that presented with (1) dorsal marginal shearing fractures (Barton's fractures), (2) radiocarpal fracture dislocations, (3) dorsal articular impacted fractures with intact or nondisplaced volar cortex, (4) isolated radial styloid fractures, and (5) massive intra-articular comminution and /or bone loss (i.e., more than five intra-articular fragments), as we believed that these could not be dealt with by volar plating alone. There were 41 female and 56 male patients. The average age was 50.3 years old (range, 18-76 years old). More than 50% of the patients (n = 50) sustained their injury after a simple fall on an outstretched hand. The remaining were work-related accidents, motor vehicle accidents, and sports injuries. Apart from four patients who had bilateral fractures, the wrist involvement for the remaining 93 patients was evenly distributed (46 dominant wrists versus 47 nondominant wrists).
The fractures were classified according to the Comprehensive Classification of Long Bone Fractures.8 There were 15 C1, 44 C2, and 42 C3 fractures (Table 1).8 Fracture displacement was volar in 13 fractures and dorsal in 88 fractures. Out of the 16 open fractures, 10 were classified as Gustillo grade 1 (i.e., open fracture with clean wound < 1 cm in length) and 6 were Gustillo grade 2 fractures (i.e., open fracture with wound between 1 and 10 cm in length without extensive soft tissue damage). For radiographic evaluation, standard anteroposterior (AP) and lateral X-ray images were taken of both wrists, with the parameters measured by ruler in millimeters based on Castaing.9 The preoperative radiographic evaluation showed an average dorsal tilt of 22° (range, 35° volar tilt to 60° dorsal tilt), an average radial inclination of 9.7° (range, -10° to 35°), and an average radial shortening of 4.3 mm (range, 0 to 12 mm). Articular incongruity (step-off or gap of the articular surface) averaged 4.0 mm (range, 1 to 10 mm).
Table 1. The distribution of the severity of intra-articular fractures of distal radius based on AO classification8.
| AO type C classification of distal radius | No of patients | |
|---|---|---|
| C1 | Simple intra-articular fracture with simple metaphyseal involvement | 15 |
| C2 | Simple intra-articular fracture with multifragmentary metaphyseal configuration | 44 |
| C3 | Multifragmentary intra-articular fracture | 42 |
Source: Müller et al8
All fractures were treated by using a fixed-angle locking plate (DVR, Biomet, Miami, Florida, USA) and a single volar incision overlying the FCR tendon.6 From 2000 to 2004, the original DVR plate used had a single distal row of 4 pegs (i.e., for 47 patients with 49 distal radius fractures). Then from 2005 onwards, for the remaining 50 patients with 52 fractures, the plates used were the DVR Anatomic, which has a double row of pegs (Fig. 1a, b). Pronation of the proximal radial shaft enabled an intrafocal reduction of the volar and dorsal articular surfaces. The plate was applied to the proximal fragment first and then used as a template to reduce the distal fragments and restore the contour of the volar surface and volar tilt. The support pegs were applied as close as possible to the subchondral bone to obtain optimal buttressing of the articular surface. For the DVR Anatomic plate, the proximal row was used to provide support of the distal and dorsal fragments while the distal row was used to support the central fragments. The number of pegs used mainly correlated with the bone quality of the patients, judged intraoperatively by the surgeons. The entire distal row was filled for patients with osteoporotic bones. Intraoperative fluoroscopy was used to obtain a 20° elevated tangential lateral view10 to confirm the absence of intraarticular screw penetration, and the dorsal horizon view11 to confirm the absence of screws emerging beyond the dorsal cortex. Ten patients were noted to have a significant metaphyseal defect intraoperatively. Bone grafting with autograft (six patients), crushed cancellous allograft (two patients), and synthetic bone substitute (two patients) were used. The time interval between the injury and surgical fracture fixation was on average 6.1 days (range, 0-12 days). Delayed open treatment was performed in seven severely comminuted C3 fractures, which were initially treated with temporary external fixation.
Fig. 1.
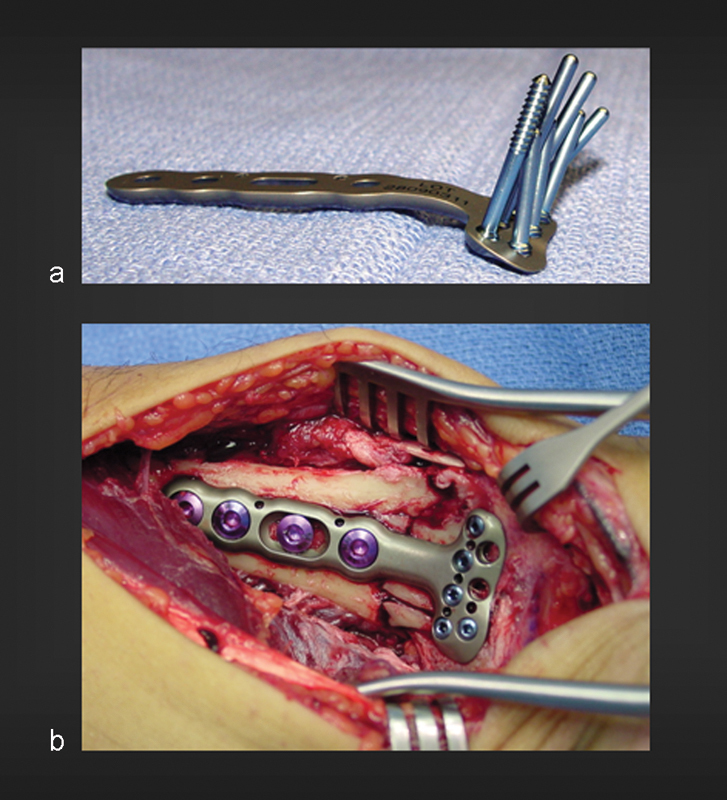
(a) DVR plate, showing the subchondral support pegs that buttress both the radial and intermediate columns of the affected articular surface. Notice the fan-shaped distribution of the pegs to conform to the anatomy of the subchondral plate. (b) DVR plate in situ in a patient with intra-articular fracture of the distal radius, exposed through a volar approach. Notice the position of the plate just proximal to the watershed line.
Distal radioulnar joint (DRUJ) instability was tested in all cases intraoperatively after the fixation of the distal radius. The distal end of the radius was grasped by the surgeon, with the forearm in a neutral position. Then the distal end of the ulna, grasped by the contralateral hand of the surgeon, was moved in the dorsal and palmar direction with respect to the radius. DRUJ instability was arbitrarily defined as an increase in the anteroposterior translation of 5-10 mm as compared with the uninjured wrist and a soft endpoint12 (Fig. 2a, b, c), when tested after the plate fixation of the distal radius. Fifty-two patients were noted to have an associated ulnar styloid fracture (28 were basistyloid fractures and 24 were more distal fractures). Only six patients (of which two patients had basistyloid fractures and four had more distal ulnar styloid frctures) were detected to have an unstable DRUJ intraoperatively, as judged by the surgeons' clinical appreciation. Two patients underwent an open triangular fibrocartilage complex (TFCC) repair, one underwent an open reduction and tension band wiring of the base of the ulnar styloid fracture, and two were conservatively treated with sugar tong splint immobilization. The remaining patient with DRUJ instability had a high-energy injury with an associated compartment syndrome and was managed with internal fixation, fasciotomy, and temporary radioulnar K-wire transfixion (Fig. 3a, b, c, and d). Other associated injuries that required additional surgical procedures included 2 ulnar neck fractures that were internally fixed.
Fig. 2.
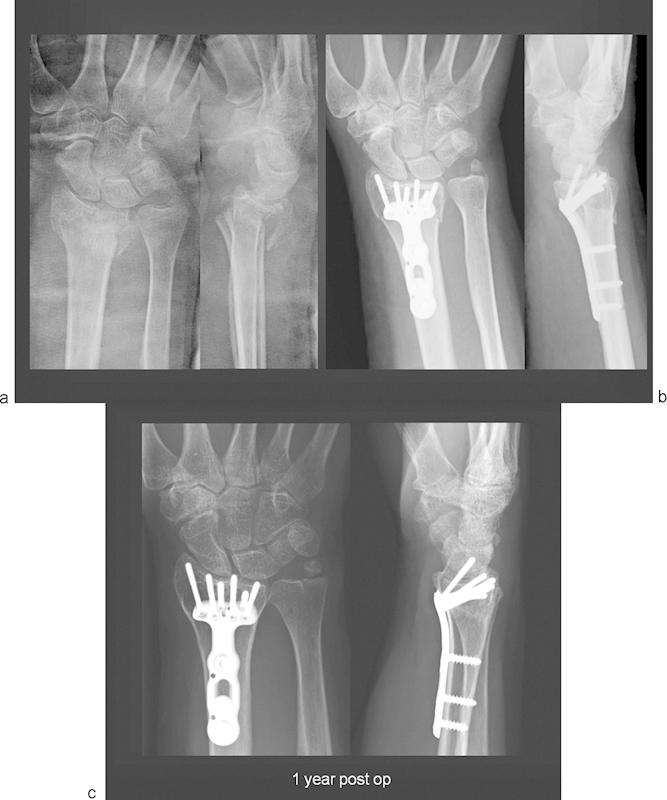
(a) X-ray images of a C3.1 intra-articular fracture with depressed lunate facet and dorsal displacement. Notice additional fracture at the base of the ulnar styloid. (b) Post-operative X-ray image showing anatomical reduction of the joint surface and restoration of length following volar fixed-angle plate fixation. (c) X-ray image at 1 year follow-up showing well-maintained joint surface and asymptomatic nonunion of the ulnar styloid.
Fig. 3.
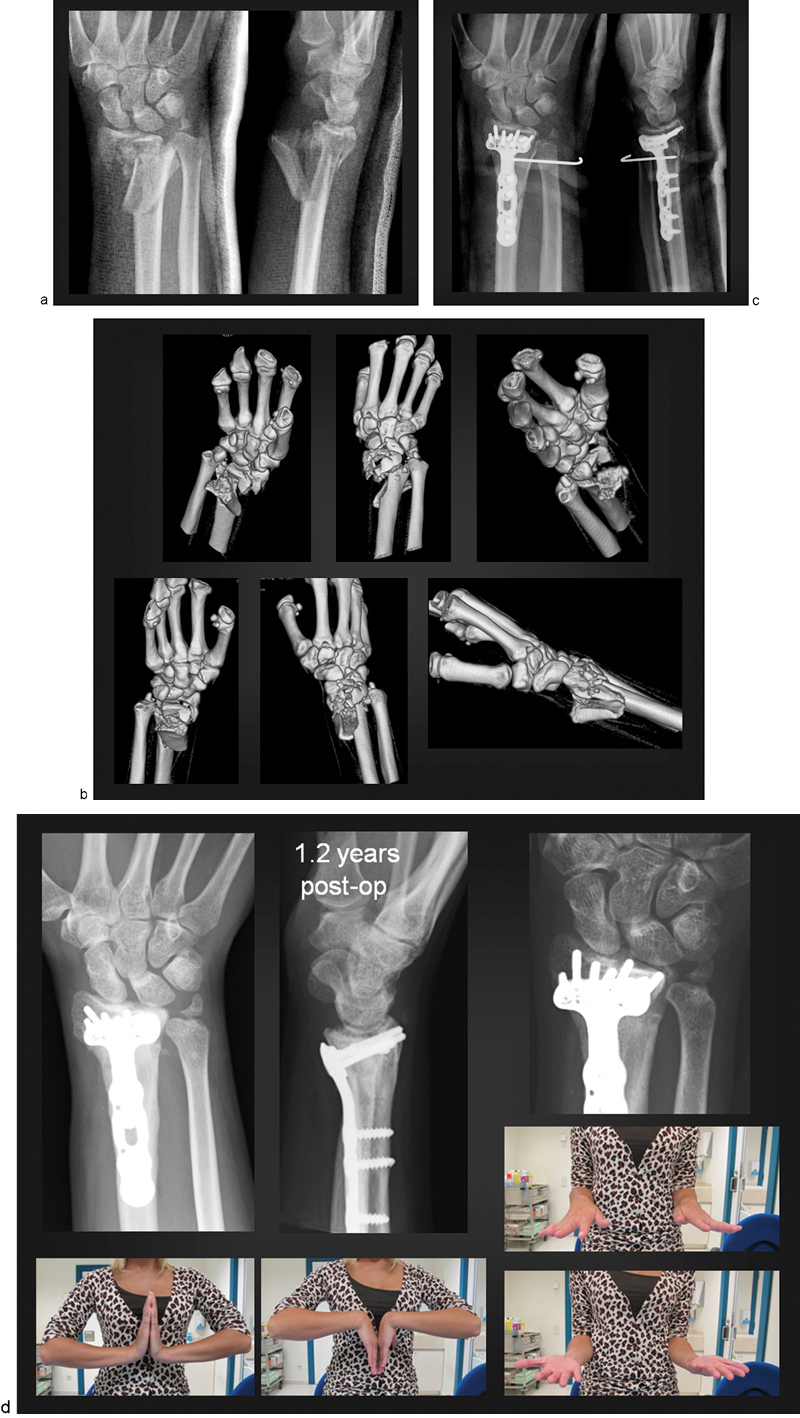
(a) X-ray images showing a high-energy intra-articular fracture of the distal radius, C3.3/Fernandez 5. (b) Three-dimensional (3D) computed tomography (CT) reconstruction revealing the extent of both the articular and metaphyseal comminution of the distal radius. Both the radiocarpal and the sigmoid notch articular surfaces are involved. Notice severe displacement of the ulnar styloid fracture. (c) Following anatomical reduction of the radius and the application of the DVR plate, the DRUJ was unstable and therefore was pinned to the radius (1.6 mm K-wire). The pin was left in place for a period of 3.5 weeks. (d) X-ray images at 1.2 years following the operation, revealing a congruent radiocarpal joint and a slight widening of the scapholunate interval. The DRUJ was noted to be well aligned, with persistent fibrous union of the ulnar styloid. Clinical photographs show almost symmetrical flexion, extension, pronation, and supination of the affected right wrist.
Postoperatively, the wrist was immobilized using a (dorsal) splint for rest. Elevation, active finger motion, and functional use of the hand were encouraged immediately after surgery. Except for patients with DRUJ instability, active wrist motion was started at 1 to 2 weeks postoperatively. For those with DRUJ instability, a sugar tong splint (or a K-wire, in one patient) was used to restrict forearm rotation for a total of 3 weeks postoperatively. Outpatient physiotherapy was provided in all cases. Heavy lifting was not allowed until signs of fracture healing were radiographically confirmed (i.e., 6-8 weeks postoperatively). The follow-up protocol was 1-2 weeks, 5-6 weeks, 3 months, 1 year, and 2 years. Clinical and radiographic assessments were performed at every visit.
The clinical outcome was evaluated with the following parameters: range of motion of the wrist and fingers, grip strength, pain according to the Fernandez pain score (Table 2)13 and the Disabilities of the Arm, Shoulder, and Hand (DASH) score. Digital motion was assessed by measuring the distance from the fingertips to the distal palmar crease; wrist and forearm motion was measured with a goniometer. Grip strength was measured using a Jamar dynamometer on the second position and compared with the contralateral side in 93 patients; this was not possible in the four patients with bilateral fractures.
Table 2. Degree of residual wrist pain, described by the patients.
| Degree of pain | Description |
|---|---|
| None | Absence of pain in carrying out all activities |
| Mild | Presence of pain only at the extreme(s) of the active range of motion of the wrist No physical or psychological disturbance was noted |
| Moderate | Presence of pain during heavy manual labor. Either physical or psychological disturbance or both was noted |
| Severe | Presence of pain occurring during activities of daily living and even at rest |
Source: Fernandez13
As for the radiographic evaluation, standard plain X-ray images of the wrist were obtained and the following parameters, according to Castaing,9 were measured: volar tilt, radial inclination, radial length and articular joint congruency. Pre-and postoperative X ray images were compared to assess the correction of the initial fragment displacement and to recognize any postoperative loss of reduction. Bone healing was defined as the presence of bridging bony trabeculae across the fracture lines on both the AP and lateral views.
Results
The average follow-up period was 28 months (range, 24-70 months). For the majority of cases, full finger motion was achieved at the end of the first week, and satisfactory forearm rotation was achieved by 8 weeks postoperatively.
At 2 years' follow-up all patients had achieved full finger range of motion. The mean wrist motion was as follows: 55.2° of extension (range, 38-85°), 53.4° of flexion (range, 40-80°), 23.6° of ulnar deviation (range, 14-40°), 15.8° of radial deviation (range, 10-26°), 79° of pronation (range, 60-90°), and 74.7° of supination (range, 30-90°). The average grip strength was 81% compared with the patient's unaffected wrist at final evaluation (range, 51-110%) (Fig. 4).
Fig. 4.
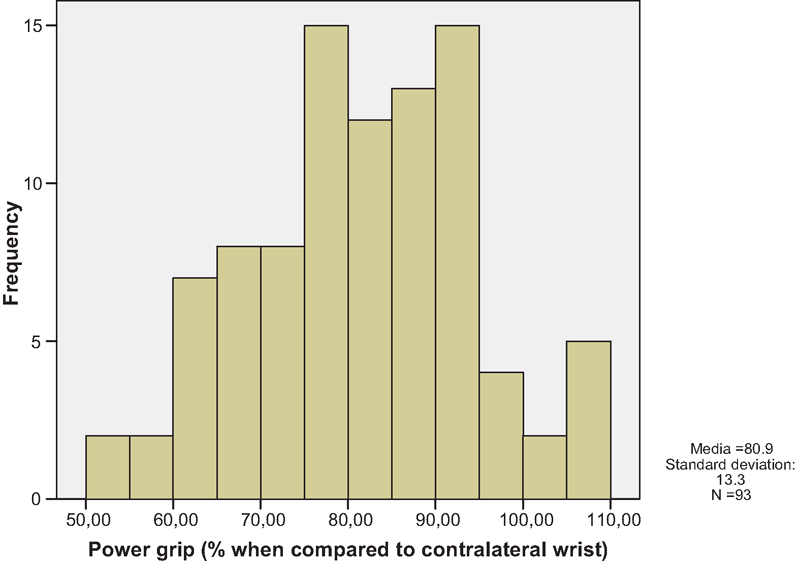
Distribution of the power grip achieved by patients postoperatively.
Seventy-four patients had no pain, 19 patients had mild pain, and 4 patients had moderate pain according to the Fernandez pain score.13 Of the 23 fractures that suffered with some residual pain, all except one had a C2 or C3 fracture pattern. Additional chondral damage or partial nonrecognized carpal ligament injuries might explain the persistence of discomfort, even though an anatomic or near-anatomic reduction of the joint surface and normal carpal alignment were achieved postoperatively. The average DASH disability/symptom score for all patients was 8.
Out of the 53 patients who were employed at the time of injury, 51 patients were able to return to work within 24 weeks of injury (depending on the nature of their work; 36 patients were manual workers and 15 had clerical jobs). For the remaining 44 patients, 26 retired patients, over the age of 65, and 4 students were able to return to their preinjury daily activities.
Radiographically, all fractures healed uneventfully with an average time to bone union of 15 weeks (range, 12-16 weeks). At final follow-up, the average volar tilt was 6.7° (range, 2° of dorsal tilt to 15° of volar tilt), radial inclination averaged 20.2° (range, 12-28°), radial shortening averaged 0.7 mm (range, 0-2 mm), and articular congruity averaged 0.14 mm (range, 0-2 mm). The position of the plate was noted to be on average 1.1 mm (range, 0-3.5 mm) proximal with respect to the watershed line. The maintenance of reduction was noted in all cases except two when follow-up X-ray images were compared with immediate postoperative images. The observed, relatively low percentage of settling in the follow-up X-ray is probably due to the fact that the DVR plates feature the spatial orientation of pegs that follow the anatomy of the subchondral surface. This is in contrast to the other locking plates that do not have this peg/screw arrangement. In the first case, 2 mm of radial shortening was observed. In the other case, a dorsoulnar fragment was found to be displaced in the postoperative period. Revision surgery with a small dorsal plate was subsequently performed at 10 days. In both cases, the loss of reduction was directly related to the surgeon's failure in placing the plate in a more distal position, allowing subsequent settling of the fracture.
Two cases of complex regional pain syndrome (CRPS) were also observed. There was no case of infection or implant failure. Late assessments of DRUJ stability revealed no case of residual joint laxity. Eighty of the patients with ulnar styloid fractures were noted to have fibrous union at the latest follow-up. Twenty percent had osseous union. The six patients who underwent treatment for DRUJ instability had a stable DRUJ at the latest follow-up.
Discussion
An anatomical reduction of the joint surface with rigid fixation is the main goal in the treatment of intra-articular fractures. It has been shown that residual intra-articular incongruity leads to posttraumatic arthritis in the long term,1,14,15 although this does not always correlate with the DASH outcomes. The treatment strategies to achieve anatomical reduction for these intra-articular fractures vary. The study demonstrates that the extended FCR approach with DVR plating provides a successful modality in treating a majority of intra-articular distal radius fractures.
The current trend of management for irreducible compression fractures of the joint surface (C3 fractures, or pilon fractures of the distal radius) has shifted from bridging external fixation, pins, and bone grafting16,17,18 to open reduction and stable internal fixation and functional after-treatment.6,7,19,20,21,22 Many studies show that the long-term functional results are equivalent, but the earlier functional results favor open reduction and internal fixation (ORIF) over external fixation.23,24,25
Unlike the dorsal approach, by using the volar approach, large volar fragments from the lunate fossa are reduced by direct manipulation and stabilized with the plate's buttressing surface and pegs. While the use of threaded pegs for the radial styloid and the ulnar corner of the proximal row is mandatory, threaded or smooth pegs can be used for the remaining screw holes, depending on the surgeon's choice intra-operatively. As for the small volar marginal fragments from the lunate fossa rim, they must be either buttressed by the plate or fixed with a separate screw, K-wires,26 or tension bands if present.
The DVR plates used in this study feature the spatial orientation of pegs that follow the anatomy of the subchondral surface. It is important to insert the distal row pegs as close as possible to the subchondral plate to prevent secondary fracture settling, as can be illustrated from the relatively low percentage of settling in our series. This is especially true for osteoporotic fractures; otherwise, the distal fragment will settle until the subchondral plate comes into contact with the buttressing pins.27,28 It is very important to select the proper plate width to provide satisfactory subchondral support across the entire articular surface as well as to capture volar ulnar fragments with at least one threaded peg, which should otherwise be stabilized with a separate dorsoulnar plate. It is noted that if the volar ulnar fragment is large and can be covered by the flange of the plate, stability of the fragment is given by the buttressing effect of the plate. The peg across it then provides additional stability to the fragment. Failure to do so could result in fragment displacement, as shown in one of our cases.
Use of a volar approach and plating avoids irritation of the extensor tendons and late tendon rupture,29,30 provided that threaded screws do not perforate the dorsal cortex.11,31,32 Plate position is important. An increase in the incidence of flexor tendon irritation and/or ruptures has recently been reported in distal plate application due to the prominence of the distal edge of the volar plate, leading to direct contact with the flexor tendons.23 Volar prominence of the plate is often associated with an insufficient fracture reduction and residual dorsal tilt of the dorsal fragment as well as with plate application distal to the watershed line.31,33,34,35,36,37,38 We observed no flexor or extensor tendon irritation or ruptures in our series. Except for one case in our series that was reduced and fixed with an inadequately narrow plate, all other cases had satisfactory restoration of the articular surface. Restoration of the volar tilt, ulnar inclination, and radial length was also highly satisfactory. Absence of settling, secondary fragment displacement, and shortening appears to correlate with accurate placement of the fixation pegs in the immediate subchondral position on each articular fragment, as the ideal position of the plate position is 0-2 mm proximal to the watershed line. The final functional outcome of the patients in our study compares favorably with other reported series of open reduction, internal fixation, and functional after-treatment of complex articular distal radial fractures.23,24,25,39,40
Instability of the DRUJ is recognized as a poor prognostic factor in the management of distal radius fractures.41 However, recent studies42 have shown that if the distal radius fractures are anatomically reduced and rigidly fixed with locking plates, no significant difference is noted in the final outcome between patients with and without ulnar styloid fractures, despite the location of the fractures and the degree of displacement. Even if the ulnar styloid fracture progresses to nonunion, no significant clinical difference has been noted when compared with patients with united ulnar styloid fractures.43,44 It is postulated that with the introduction of anatomical locking plates, the osteoarticular congruency of the DRUJ has improved through anatomical restoration of the position of the sigmoid notch and radial length. Thus, despite the presence of “unstable“ lesions of the TFCC with or without ulnar styloid fracture, well-vascularized peripheral tears may heal in a short period of time, rendering the joint stable with or without postoperative immobilization as early as 3 weeks, following surgery. We observed similar findings in our cases. Although more than 50% of patients had associated ulnar styloid fractures, only six patients were found to have DRUJ instability intraoperatively, requiring temporary stabilization of the DRUJ. These patients were noted to have stable DRUJ at 6 weeks, of which were also maintained at the latest follow-up. No significant ulnar wrist pain has been noted at the final assessment in these patients.
The shortcomings of the present study include the fact that it is retrospective, which introduces bias. There was no control group; hence, no conclusions can be made as to comparison with other types of treatment methods. The series was nonhomogeneous and included different cohorts ranging from simple articular to complex intra-articular fracture patterns, which were not analyzed separately. Similarly, the patients with DRUJ instability or an ulnar neck fracture represent a different cohort, which may confound the results. Nevertheless, this study demonstrates that with the execution of good surgical techniques, including proper plate position, proper insertion of pegs and avoidance of past pointing, and proper patient selection, a satisfactory functional and radiological outcome can be obtained for a great majority of patients with complex intra-articular distal radius fractures by using a volar approach and a single locking plate.
Conflicts of Interest Professor DL Fernandez is currently a consultant for Biomet. Dr Orbay received royalties from other Depuy products, but not from DVR plates. All other named authors hereby declare that they have no conflicts of interest to disclose.
Notes
This study does not receive any financial support from any company or government body.
None of the cases, illustrations, images, and figures given contains any identifiable patient information.
References
- 1.Cooney W P III Linscheid R L Dobyns J H External pin fixation for unstable Colles' fractures J Bone Joint Surg Am 197961(6A):840–845. [PubMed] [Google Scholar]
- 2.Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011;93(23):2146–2153. doi: 10.2106/JBJS.J.01597. [DOI] [PubMed] [Google Scholar]
- 3.Trumble T E, Schmitt S R, Vedder N B. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg Am. 1994;19(2):325–340. doi: 10.1016/0363-5023(94)90028-0. [DOI] [PubMed] [Google Scholar]
- 4.Wolfe S W, Pike L, Slade J F III, Katz L D. Augmentation of distal radius fracture fixation with coralline hydroxyapatite bone graft substitute. J Hand Surg Am. 1999;24(4):816–827. doi: 10.1053/jhsu.1999.0816. [DOI] [PubMed] [Google Scholar]
- 5.Medoff R J. Fragment-specific fixation of distal radius fractures. Atlas of the Hand Clinics. 2006;11(2):163–174. [Google Scholar]
- 6.Orbay J L, Fernandez D L. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am. 2002;27(2):205–215. doi: 10.1053/jhsu.2002.32081. [DOI] [PubMed] [Google Scholar]
- 7.Musgrave D S, Idler R S. Volar fixation of dorsally displaced distal radius fractures using the 2.4-mm locking compression plates. J Hand Surg Am. 2005;30(4):743–749. doi: 10.1016/j.jhsa.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Müller M Nazarian S, Koch P, Schatzker J. Berlin, Germany: Springer-Verlag; 1990. The Comprehensive Classification of Fractures of Long Bones. [Google Scholar]
- 9.Castaing J. Recent fractures of the lower extremity of the radius in adults [in French] Rev Chir Orthop Repar Appar Mot. 1964;50:581–696. [PubMed] [Google Scholar]
- 10.Soong M, Got C, Katarincic J, Akelman E. Fluoroscopic evaluation of intra-articular screw placement during locked volar plating of the distal radius: a cadaveric study. J Hand Surg Am. 2008;33(10):1720–1723. doi: 10.1016/j.jhsa.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 11.Joseph S J, Harvey J N. The dorsal horizon view: detecting screw protrusion at the distal radius. J Hand Surg Am. 2011;36(10):1691–1693. doi: 10.1016/j.jhsa.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 12.Atzei A. New trends in arthroscopic management of type 1-B TFCC injuries with DRUJ instability. J Hand Surg Eur Vol. 2009;34(5):582–591. doi: 10.1177/1753193409100120. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez D L. Radial osteotomy and Bowers arthroplasty for malunited fractures of the distal end of the radius. J Bone Joint Surg Am. 1988;70(10):1538–1551. [PubMed] [Google Scholar]
- 14.Jakob M, Rikli D A, Regazzoni P. Fractures of the distal radius treated by internal fixation and early function. A prospective study of 73 consecutive patients. J Bone Joint Surg Br. 2000;82(3):340–344. doi: 10.1302/0301-620x.82b3.10099. [DOI] [PubMed] [Google Scholar]
- 15.Lutz M, Arora R, Krappinger D, Wambacher M, Rieger M, Pechlaner S. Arthritis predicting factors in distal intraarticular radius fractures. Arch Orthop Trauma Surg. 2011;131(8):1121–1126. doi: 10.1007/s00402-010-1211-3. [DOI] [PubMed] [Google Scholar]
- 16.Edwards G S Jr. Intra-articular fractures of the distal part of the radius treated with the small AO external fixator. J Bone Joint Surg Am. 1991;73(8):1241–1250. [PubMed] [Google Scholar]
- 17.Bini A, Surace M F, Pilato G. Complex articular fractures of the distal radius: the role of closed reduction and external fixation. J Hand Surg Eur Vol. 2008;33(3):305–310. doi: 10.1177/1753193408087092. [DOI] [PubMed] [Google Scholar]
- 18.Glickel S Z, Catalano L W, Raia F J, Barron O A, Grabow R, Chia B. Long-term outcomes of closed reduction and percutaneous pinning for the treatment of distal radius fractures. J Hand Surg Am. 2008;33(10):1700–1705. doi: 10.1016/j.jhsa.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Ellis J. Smith's and Barton's fractures. A method of treatment. J Bone Joint Surg Br. 1965;47(4):724–727. [PubMed] [Google Scholar]
- 20.Jupiter J B, Fernandez D L, Toh C L, Fellman T, Ring D. Operative treatment of volar intra-articular fractures of the distal end of the radius. J Bone Joint Surg Am. 1996;78(12):1817–1828. doi: 10.2106/00004623-199612000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Khamaisy S, Weil Y A, Safran O, Liebergall M, Mosheiff R, Khoury A. Outcome of dorsally comminuted versus intact distal radial fracture fixed with volar locking plates. Injury. 2011;42(4):393–396. doi: 10.1016/j.injury.2010.10.011. [DOI] [PubMed] [Google Scholar]
- 22.Chung K C Petruska E A Treatment of unstable distal radial fractures with the volar locking plating system. Surgical technique J Bone Joint Surg Am 200789(Suppl 2 Pt.2):256–266. [DOI] [PubMed] [Google Scholar]
- 23.Rozental T D, Blazar P E. Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg Am. 2006;31(3):359–365. doi: 10.1016/j.jhsa.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 24.Egol K, Walsh M, Tejwani N, McLaurin T, Wynn C, Paksima N. Bridging external fixation and supplementary Kirschner-wire fixation versus volar locked plating for unstable fractures of the distal radius: a randomised, prospective trial. J Bone Joint Surg Br. 2008;90(9):1214–1221. doi: 10.1302/0301-620X.90B9.20521. [DOI] [PubMed] [Google Scholar]
- 25.Wright T W, Horodyski M, Smith D W. Functional outcome of unstable distal radius fractures: ORIF with a volar fixed-angle tine plate versus external fixation. J Hand Surg Am. 2005;30(2):289–299. doi: 10.1016/j.jhsa.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 26.Harness N G, Jupiter J B, Orbay J L, Raskin K B, Fernandez D L. Loss of fixation of the volar lunate facet fragment in fractures of the distal part of the radius. J Bone Joint Surg Am. 2004;86-A(9):1900–1908. doi: 10.2106/00004623-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Gehrmann S V, Windolf J, Kaufmann R A. Distal radius fracture management in elderly patients: a literature review. J Hand Surg Am. 2008;33(3):421–429. doi: 10.1016/j.jhsa.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 28.Orbay J L, Fernandez D L. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am. 2004;29(1):96–102. doi: 10.1016/j.jhsa.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 29.Chiang P P, Roach S, Baratz M E. Failure of a retinacular flap to prevent dorsal wrist pain after titanium Pi plate fixation of distal radius fractures. J Hand Surg Am. 2002;27(4):724–728. doi: 10.1053/jhsu.2002.33703. [DOI] [PubMed] [Google Scholar]
- 30.Tyllianakis M E, Panagopoulos A M, Saridis A. Long-term results of dorsally displaced distal radius fractures treated with the pi-plate: Is hardware removal necessary? Orthopedics. 2011;34(7):e282–e286. doi: 10.3928/01477447-20110526-10. [DOI] [PubMed] [Google Scholar]
- 31.Berglund L M, Messer T M. Complications of volar plate fixation for managing distal radius fractures. J Am Acad Orthop Surg. 2009;17(6):369–377. doi: 10.5435/00124635-200906000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Benson E C, DeCarvalho A, Mikola E A, Veitch J M, Moneim M S. Two potential causes of EPL rupture after distal radius volar plate fixation. Clin Orthop Relat Res. 2006;451:218–222. doi: 10.1097/01.blo.0000223998.02765.0d. [DOI] [PubMed] [Google Scholar]
- 33.Yu Y R, Makhni M C, Tabrizi S, Rozental T D, Mundanthanam G, Day C S. Complications of low-profile dorsal versus volar locking plates in the distal radius: a comparative study. J Hand Surg Am. 2011;36(7):1135–1141. doi: 10.1016/j.jhsa.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 34.Soong M, van Leerdam R, Guitton T G, Got C, Katarincic J, Ring D. Fracture of the distal radius: risk factors for complications after locked volar plate fixation. J Hand Surg Am. 2011;36(1):3–9. doi: 10.1016/j.jhsa.2010.09.033. [DOI] [PubMed] [Google Scholar]
- 35.Koo S C, Ho S T. Delayed rupture of flexor pollicis longus tendon after volar plating of the distal radius. Hand Surg. 2006;11(1-2):67–70. doi: 10.1142/S0218810406003048. [DOI] [PubMed] [Google Scholar]
- 36.Casaletto J A, Machin D, Leung R, Brown D J. Flexor pollicis longus tendon ruptures after palmar plate fixation of fractures of the distal radius. J Hand Surg Eur Vol. 2009;34(4):471–474. doi: 10.1177/1753193408100964. [DOI] [PubMed] [Google Scholar]
- 37.Cross A W, Schmidt C C. Flexor tendon injuries following locked volar plating of distal radius fractures. J Hand Surg Am. 2008;33(2):164–167. doi: 10.1016/j.jhsa.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 38.Nunley J A, Rowan P R. Delayed rupture of the flexor pollicis longus tendon after inappropriate placement of the Pi plate on the volar surface of the distal radius. J Hand Surg Am. 1999;24(6):1279–1280. doi: 10.1053/jhsu.1999.1279. [DOI] [PubMed] [Google Scholar]
- 39.Trumble T E, Culp R W, Hanel D P, Geissler W B, Berger R A. Intra-articular fracture of the distal aspect of the radius-An Instructioanl Course lecture: The American Academy of Orthopaedic Surgeons. J Bone Joint Surg Am. 1998;80(4):582–600. [Google Scholar]
- 40.Bradway J K, Amadio P C, Cooney W P. Open reduction and internal fixation of displaced, comminuted intra-articular fractures of the distal end of the radius. J Bone Joint Surg Am. 1989;71(6):839–847. [PubMed] [Google Scholar]
- 41.Lindau T, Hagberg L, Adlercreutz C, Jonsson K, Aspenberg P. Distal radioulnar instability is an independent worsening factor in distal radial fractures. Clin Orthop Relat Res. 2000;(376):229–235. doi: 10.1097/00003086-200007000-00031. [DOI] [PubMed] [Google Scholar]
- 42.Zenke Y, Sakai A, Oshige T, Moritani S, Nakamura T. The effect of an associated ulnar styloid fracture on the outcome after fixation of a fracture of the distal radius. J Bone Joint Surg Br. 2009;91(1):102–107. doi: 10.1302/0301-620X.91B1.21026. [DOI] [PubMed] [Google Scholar]
- 43.Buijze G A, Ring D. Clinical impact of united versus nonunited fractures of the proximal half of the ulnar styloid following volar plate fixation of the distal radius. J Hand Surg Am. 2010;35(2):223–227. doi: 10.1016/j.jhsa.2009.10.035. [DOI] [PubMed] [Google Scholar]
- 44.Kim J K, Koh Y D, Do N H. Should an ulnar styloid fracture be fixed following volar plate fixation of a distal radial fracture? J Bone Joint Surg Am. 2010;92(1):1–6. doi: 10.2106/JBJS.H.01738. [DOI] [PubMed] [Google Scholar]


