Abstract
Equity in health has been the underlying value of the World Health Organization’s (WHO) Health for All policy for 30 years. This article examines how cities have translated this principle into action. Using information designed to help evaluate phase IV (2003–2008) of the WHO European Healthy Cities Network (WHO-EHCN) plus documentation from city programs and websites, an attempt is made to assess how far the concept of equity in health is understood, the political will to tackle the issue, and types of action taken. Results show that although cities continue to focus considerable support on vulnerable groups, rather than the full social gradient, most are now making the necessary shift towards more upstream policies to tackle determinants of health such as poverty, unemployment, education, housing, and the environment, without neglecting access to care. Although local level data reflecting inequalities in health is improving, there is still a long way to go in some cities. The Healthy Cities Project is becoming an integral part of structures for long-term planning and intersectoral action for health in cities, and Health Impact Assessment is gradually being developed. Participation in the WHO-EHCN appears to allow new members to leap-frog ahead established cities. However, this evaluation also exposes barriers to effective local policies and processes to reduce health inequalities. Armed with locally generated evidence of critical success factors, the WHO-EHCN has embarked on a more rigorous and determined effort to achieve the prerequisites for equity in health. More attention will be given to evaluating the effectiveness of action taken and to dealing not only with the most vulnerable but a greater part of the gradient in socioeconomic health inequalities.
Keywords: Equity, Healthy cities, Social determinants, Health equality
Introduction
Following the 19771 World Health Assembly resolution to address inequalities in health, the “Health for All” (HFA) strategy clarified that this can only be tackled through action influencing the broader social determinants of health. The HFA principles have underpinned the work of the WHO European Healthy Cities Network (WHO-EHCN) since its inception in 1987.
In the WHO European Region, considerable efforts were made to broaden understanding of the policy implications of tackling inequalities in health. In the early 1990s, discussion papers2–4 clarified what is meant by equity in health, how inequality might be measured, and what policies and strategies would be most likely to reduce the gaps. Intended for a nontechnical audience, these documents were widely translated and incorporated in training material for a range of disciplines.
A distinction was made between differences in health status affected by fixed factors such as age, gender and genetics, and those amenable to change. Inequity in health refers to differences in variable factors such as lifestyles, personal and family circumstances, social and community networks, and general socioeconomic, cultural and environmental conditions. Adopting the principle of equity in health requires interventions to tackle differences that are avoidable and considered unjust. Judgments on what is unfair vary by time and place, but one widely used criterion is the degree of choice involved. If people have little choice in their living and working conditions, the resulting health differences are more likely to be considered unjust than those resulting from health risks chosen voluntarily. Moreover, disadvantages related to education, income, environment, and other factors tend to reinforce each other, making certain groups very vulnerable to ill health.
Europe has experienced great changes since these policy documents were published in the early 1990s. There is an increasing body of evidence concerning the social determinants of health and more sensitive and reliable measures for assessing inequities in health. In 1997, the WHO-EHCN commissioned The Solid Facts,5 designed to indicate in terms understood by policy-makers, stated that “the role that public policy can play in shaping the social environment in ways conducive to better health.”6 In presenting their evidence, contributing experts emphasized the need for a more just and caring society. In 2007, the WHO Venice Office invited the authors of the first discussion papers to reconsider the concepts and principles and possible strategies for tackling social inequities in health.7,8
On a global level, the WHO Commission on Macroeconomics and Health brought the economic argument more firmly on the agenda, showing “how disease is a drain on societies, and investments in health can be a concrete input to economic development.”9 In 2005, WHO established a Commission on Social Determinants of Health (CSDH). Nine Knowledge Networks collected and synthesized evidence on (a) plausible causal relations, (b) key areas in which action should take place, and (c) effective practices and interventions for addressing socially determined health inequities globally.10 The Commission reported in 2008 with a call to close the (health) gap in a generation,11 and a report on the implications for cities.12 A similar review is now being carried out for Europe,13 as background information for a new health policy for Europe, accompanied by a report on the implications for the local level.14
The principle of equity in health has gained acceptance in the work of the wider United Nations system, particularly through recognition of poverty as a major cause of ill health and mortality.15 The UNDP16 and World Bank,17 for example, have presented ambitious policies to reduce poverty and carry out poverty impact assessment. There has been a strong focus in the EU on reducing poverty and social exclusion, with countries called upon to formulate national plans for their reduction.18
Although the terms poverty and inequality are often used interchangeably, poverty refers to the most disadvantaged, whereas inequality reflects the full social gradient. The WHO European health policy HEALTH2119 suggested that, although priority should be given to the most disadvantaged, the distribution of the determinants of health among all social groups should be addressed. The CSDH stresses that not only the needs of the most vulnerable should be tackled but also the social gradient in health that runs from top to bottom of the socioeconomic spectrum. Both the CSDH reports and other researchers emphasize that tackling the social determinants of health (SDH) does not automatically tackle health inequalities.20
Although there is no agreement on how socioeconomic inequality in health should be conceptualized,21 it is usually characterized in terms of level of income, education, occupation, and, to some extent, income-related indicators such as home or car ownership. It is frequently analyzed by gender, age, and area-based measures, for which some countries have developed complex indicators of deprivation. Health21 includes vulnerable groups such as women, physically or mentally disabled people, elderly people, immigrants, and refugees under the equity in health label.
The evaluation of phase IV of the WHO-EHCN, aimed to understand the following:
whether equity in health is on the political agenda in cities, and if so, how it is conceived;
whether information is available for raising awareness, defining health inequalities to be tackled, and monitoring progress;
whether the past focus on access to health care and care for certain vulnerable groups has shifted to deal with the wider spectrum of inequalities; and
what are the main areas and types of interventions.
The results, available to the WHO-EHCN at the end of phase IV, have informed the development of a framework for action in phase V (2009–2013).
Methodology
This article draws on information gathered during the regular assessment of progress by member cities of the WHO-EHCN:
self-reporting by member cities;
abstracts submitted for the 2008 International Healthy Cities Conference; and
international bibliography and selected national level policy documents indicating the context in which cities are working.
The main source of information was an analysis of replies to a General Evaluation Questionnaire completed by 59 cities in 23 countries in 2008. Seven questions related to inequalities in health and SDH. Cross-reference was made to other relevant questions, such as those concerning the monitoring of health inequalities.
Open-ended questions facilitated a potentially rich input from respondents, but the comprehensiveness of replies was vulnerable to their interest and time pressures, as reflected in the considerable variation in responses. Cultural background and the stage of development of equity issues also affected replies. In cases where historical analysis indicates long-term concern, there is a tendency for more critical reporting compared with certain cities where equity is new on the agenda. Since cities were asked to cite both initiatives of their Healthy Cities Project and other agencies, the results indicate the general progress in promoting equity in health, as seen from the HCP perspective.
Results
Understanding the Concept of Equity in Health
Q.4.2 “How does your city understand the concept and the implications of ‘equity’/‘health inequalities’”?
Guidance for this question asked whether there were differing views, referred to HFA and the Horsens Statement,22 and distinguished between inequalities and inequity. The formulation was rather problematic in that geographic differences were presented as inevitable, and English is the only European language with separate words for “equity” and “equality.”
Four cities did not reply to this question. One gave an unrelated reply. Only 17 mentioned whether or not there is a common understanding, and of those, only nine stated unequivocally that there is indeed common understanding between stakeholders. Most of those replying that the concept is not generally understood, or that there are differing views, were among the newcomers to the HC project. However, two phase I cities (Milan and Turku) also pointed out that this is not an easy concept to grasp.
Thirty-eight cities (64 % of respondents) referred to a rather broad concept of equity in health, reflecting the WHO HFA definition, or the social determinants of health. Most cities illustrated their conception by listing policies or programs offered. Only a handful provided the definition outlined in their policy documents.
In contrast to previous evaluations, only six respondents said that equity in health was seen mainly in terms of access to health care. All except one of these were comparative newcomers to the project. Interestingly, although Pecs has progressed on many fronts, the respondent felt that “it is very difficult to change the traditional attitude…A lot of decision-makers still think that health inequalities are created in the health services and do not consider the broad social determinants of health.”
Putting and Keeping Equity in Health on the Agenda
Three questions were linked to this issue:
Q.5.3 How does your city measure and monitor inequalities in health?
Q.4.3 How much importance is given to equity/inequalities in health?
Q.4.7 What role did the HCP have in raising the importance of equity/inequalities in the city?
Simply walking or driving around a city gives a rough impression of socioeconomic inequalities, but more hard evidence is usually necessary to put equity on the political agenda.
The 1993 evaluation of phase I (1987–1992) of the WHO-EHCN showed that few cities had good experience of developing small-area information, and information to measure and monitor equity in health was inadequate.23 It was felt necessary to carry out population health surveys in phase II (1993–1997). Reviews of city health profiles in the mid-1990s24 indicated that, with notable exceptions, inequality in health was still not adequately covered and, in some cases, not clearly identified as an issue. Subcity level information was scarce, and few profiles presented data on lifestyles according to socioeconomic groups. By the end of phase III (1998–2002), 20 cities (49 %) were monitoring inequality in health at subcity level.
Guidance for question 5.3 referred to subareas of the city and vulnerable groups and whether changes are tracked over time. There was no reference to variables for measuring socioeconomic status, such as income level, occupation, or education. Replies were, therefore, of a rather general nature. Access to “city profiles” would doubtlessly give an overview of indicators used but were not available at the time of writing.
Fifty-seven cities replied to this question, four stating that they do not monitor inequalities in health. Three simply cited the institution responsible for monitoring. Twenty-one cities appeared to be monitoring on a regular basis through regularly collected data or surveys. A further nine cities were conducting special issue surveys, but it was not clear whether these were one-off or conducted on a regular basis.
Of the cities where the focus was on geographic variations, a number were putting their efforts into profiling particularly disadvantaged areas. Cities in the UK and Scandinavia, in particular, were fortunate in having small-area data. Vulnerable groups, particularly older people, migrants, children, and women were mentioned as being studied but did not seem to dominate the process as was the case in phase III. Cities such as Barcelona and Liverpool had taken advantage of local universities particularly active in the area of inequalities research, and Sheffield was said to have a “nationally renowned performance management system for monitoring inequalities”.
In relation to the importance given to equity in health, 71 % (42 cities) said that it was very important in their city; 19 % (11 cities), moderately important; 7 % (4 cities), of little importance; and none that it was of “no importance”.
Fifty-five cities replied to question 4.7 concerning the role played by the HCP in raising the issue of equity in health. Eleven considered this to be of strategic importance, indicating that equity would not have been on the agenda without their input, whereas five considered their role to have been rather small or too early to evaluate.
The majority indicated areas where they felt they had played a significant role. The two most frequently mentioned were as follows: convincing politicians of the importance of tackling inequalities in health, by providing the evidence in city profiles, or from international experience; and encouraging intersectoral collaboration, mainly through participation in steering groups and committees, with particular reference to the formulation of development plans and strategies.
Some cities felt they had contributed significantly to specific action, for example: introduction of the HFA principles into the planning process in Aydin Saglik and Stavropol; introduction of HIA in Pecs; inclusion of vulnerable groups in sample surveys in Galway; the promotion of healthy aging in Horsens and Stockholm; support for the disabled in Eskisehr; the development of a toolkit for equity auditing in Stoke-on-Trent; and a lead role in Liverpool, impacting also on a national level, for banning smoking in the workplace.
Taking Action to Promote Equity in Health
Two questions focussed directly on approaches and actions to promote equity in health:
Q.4.4 Are there specific policies and programs in your city that address equity/health inequalities?
Q.4.5 Could you list other important policies and programs in your city that can have an (implicit) impact on equity/health inequalities?
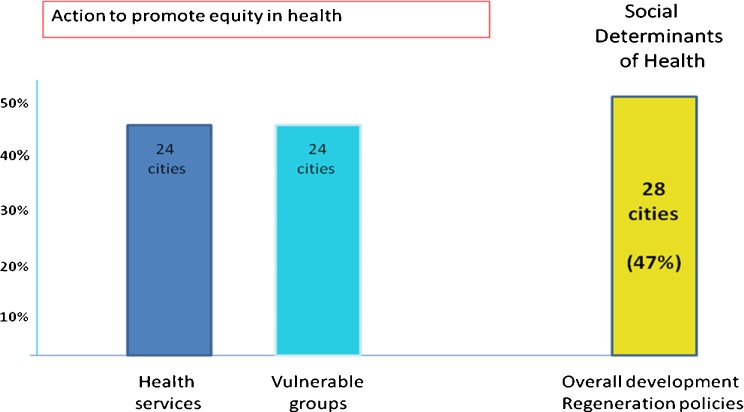
Fifty-six cities responded to question 4.4, four of which had no programs specifically to tackle inequalities. Almost all cities referred to more than one field of action. Forty-one percent (24 cities) referred to actions from within the health sector (health education, disease prevention, health care). In most cases, these appeared to be targeted at high risk or vulnerable groups. For example, health promotion for the elderly and disabled in Rijeka; screening for tuberculosis in disadvantaged areas of Barcelona; free screening for cancer and cardiovascular disease in Liege; mobile health units to reach those who cannot travel in Eskisehr; and providing primary health care for the uninsured in disadvantaged regions of Cancaya.
Twenty-four cities referred to support to vulnerable groups. Immigrants and older people were mentioned most frequently (12 and 11 cities, respectively), followed by disabled people (eight cities), and children and women—the last two also being the target of a number of the “health sector” programs.
Twenty-one cities (36 %) clearly linked the tackling of inequalities in health directly to dealing with SDH, referring to overall development programs, regeneration programs, or those designed to tackle poverty and social exclusion. This approach was particularly strong in cities in the UK, Denmark, Finland, and Sweden. Pecs in Hungary reported trying to tackle inequalities in health through “all ongoing programs”.
Some of these 21 cities marshaled specific SDH to tackle inequalities in health, including, for example, housing, mainly the provision of social housing or rent subsidies, with Eskisehr carrying out a screening program to assess the suitability of housing for their residents. A number of cities were trying to improve access to employment and better income by supporting the development of small businesses in Stavropol, for example, and tackling adult literacy in Seixal. Finally, Kuopio, Turku, and Stockholm were developing specific equity policies or projects.
Question 4.5 invited cities to list actions where the impact on equity in health is implicit rather than explicit. Fifty-four cities replied to this question.
There was naturally some overlap with question 4.1, and 14 cities referred to overall development, regeneration, community development, and social inclusion/exclusion programs. Ten cities referred to specific actions to improve the economy or the labor market and access to employment. For example, Belfast and Leganes referred to skill building/professional training; Poznan, to preparing women for professional life; and Manchester, to attempts by local hospitals to draw more of their staff from the local area.
Seventeen cities mentioned actions in the education sector. Some encouraged access to employment, for example, by improving adult literacy rates and adult education in general. Others emphasized the educational needs of children at an early age. Examples were England’s “Sure-Start” and “special needs” programs. Dimitrovgrad also cited the provision of preschool education as one way of facilitating women’s entrance to the labor market.
Access to sports (and in some cases cultural) facilities, mainly through free or reduced-price facilities, were high on the list for 20 cities, as implicitly affecting inequalities in health. Fourteen cities referred to programs supporting children, youth, and the family, including gender issues such as the resurgence of Women’s Associations in Milan.
A small number of cities listed a wide range of actions in relation to environmental issues such as “greening” the city and planting trees and support for vulnerable groups, particularly older people or the disabled, and support to immigrants, including the establishment of immigrant’s associations and councils, teaching immigrants to use the national language, and the establishment of a radio station for immigrants in Athens.
A number of cities referred to improvement of the participation process, including the development of local district councils in Rennes; consumer organizations and an Omsbudsperson in Arezzo; and support of NGOs and improved consultation methods. Attempts to broaden access to new technology and personal computers were mentioned by three cities.
Q.4.1 “Are there specific policies and programs in your city that address the wider social determinants of health?”
Using the well-known Dahlgren/Whitehead “rainbow”, the guidance given for this question (not included in the phase III evaluation) distinguished between proximal interventions and more “upstream” or distal determinants such as income and employment.
Fifty-seven cities responded, their replies falling roughly into eight broad groups, with most listing more than one:
general development and regeneration of disadvantaged areas;
actions dealing with the economy, income/poverty, and employment;
the environment, spatial planning, sports and culture;
action related to individual sectors such as housing or education;
safety and crime prevention;
health care;
lifestyle issues; and
care for vulnerable groups.
Forty-seven percent (28 cities) referred to overall development policies and strategies or the regeneration of disadvantaged areas. These included all but one of the phase I cities. The UK cities formed a distinct group in this respect, referring to regeneration strategies, sustainable community strategies, local area agreements, and local development frameworks. Sunderland’s Local Area Agreement, for example, aims at creating “a prosperous and learning city, and a healthy city and high quality environment”.
Twenty-four cities said they were taking action to enhance the economy or reduce poverty and unemployment. In three of the seven Turkish cities, this included vocational training or training for business skills, and Kuopio was trying to develop the intermediate labor market. Fifteen cities referred to spatial planning, creating a greener environment, and more sports facilities. Of action in individual sectors, housing, education, transport, and crime prevention were most frequently mentioned. A small number of cities mention health care or lifestyle issues, not all of which appeared relevant to tackling social determinants.
Thirty-one cities (53 %) referred to actions in support of vulnerable groups. Most frequently mentioned (13 cities) were children and/or the family, (Eskisehr stating the family to be the “main determinant” of health), older people, immigrants/ethnic minorities, the disabled, and women. It was not possible in many cases to ascertain whether these were traditional downstream services or, as in the case of Vitoria–Gasteiz, where the provision of child care was seen as enabling more women to enter the labor market.
Checking How Policies of Other Sectors Affect Equity in Health
Q.4.6 referred to “mechanisms to check (audit) existing and new policies, plans and programs for their impact on ‘equity’/‘health inequalities’”
In 1999, the WHO European Centre for Health Policy proposed that Health Impact Assessment (HIA) should focus not only on the aggregate impact of policies in other sectors on health but also on the distribution of potential effects.25 A review of HIA in European countries26 indicated that this definition has been widely accepted. However, the relevant literature offers few examples where the health impact of policies on different population groups has been assessed. HIA was one of the core themes for phase IV.
Fifty-six cities responded to this question. Thirty-two percent (19 cities) replied that they do not check/audit policies and programs for their impact on equity in health. The replies of a further seven indicated that they had perhaps not understood the question and were, in fact, referring to their regular evaluation of programs and projects.
Of the 15 cities replying in the affirmative, eight were from the UK, where HIA is being rapidly developed. Newcastle, for example, checks national and local policies and the Primary Health Care Authority (PHC) in Brighton checks all local authority policies; legislation in Belfast calls for a check in relation to nine population groups; Manchester so far restricts this to PHC; and in Liverpool where the University is one of the forerunners in HIA, a toolkit has been developed to assess mental health impacts, which have tended to be the Cinderella of the HIA process.
Pecs has a well-established approach, with all departments required to have a designated “health filter”, tasked with assessing possible health impacts of policies. Helsingborg uses a “Balanced Score Card system”. In cities such as Dresden, Galway, and Rennes, for example, the impact of policies on equity in health may be assessed as part of impact assessments related to “social inclusion” and sustainability. Other cities mention that reporting on EU-funded projects has some bearing on this issue.
Discussion
Although far from being a neat, linear process, the stages of policy development may be defined as follows: awareness building, policy formulation, implementation, monitoring and evaluation, reassessment, and revision.27 The promotion of equity in health in cities in the WHO-EHCN has entered the policy development cycle to varying degrees.
Raising Awareness of the Issues
The focus of mainstream academic studies is on inequalities in health associated with differences in socioeconomic circumstances. Outside the UK, Scandinavia, and more recently, France, few cities have access to health data disaggregated by variables such as income, education, and employment. Consequently in measuring and monitoring inequalities, network cities tend pragmatically to emphasize neighborhood differentials in health status, and/or the heath status of vulnerable groups. Vulnerable groups, including children, older people, disabled people, women, migrants, and ethnic minorities, are referred to either in relation to understanding the concept, monitoring and measuring, or action taken. Poverty and social exclusion/inclusion are high on the agenda in a number of cities, particularly those in EU countries. Access to health care and other services is monitored in a number of cities. In some cases, it is still assumed that, if services are equally available, they will be equally utilized, whereas international research has shown that this is frequently not the case.28
Whatever the weakness of many of the local databases for reflecting inequities in health, certain prerequisites, and structures required for participation in the WHO-EHCN appear to have been conducive in raising awareness of the importance of tackling inequalities in health and recognition that this requires intersectoral collaboration. The preparation of “city profiles” (some cities also developed “older people’s profiles” or “migrants’ profiles”) raised the equity issue. The fact that the Mayor, Deputy-Mayor, or other politician chair or are members of the HCP Steering Committee exposes them to the WHO HFA principles and the equity debate, and these politicians work across sectors. Furthermore, this has, in some cases, ensured cross-party political support. Almost all the “newcomers” (who joined in Phase IV) report having raised awareness among their politicians.
Formulating Policies to Address Inequality in Health
Thirty-three cities (56 %) reported either being closely involved in policy and planning structures or in bodies for intersectoral collaboration. Since this is their specific remit, it can be expected that they will at least have brought equity issues to the planning platform. In comparison to the initial phases of the HCP, an increasing number of cities are formulating City Health Development Plans or incorporating health issues in overall development strategies.
Interventions to Address Inequality in Health
An examination of policies implemented by cities involved in phase II indicated that, although they were making efforts to tackle inequality in health, they had yet to move from a traditional health education focus on proximal lifestyle determinants to more strategic intervention on distal and intermediate determinants.29 This reflected similar findings at the national level.30 During phase III, cities cited a huge diversity of programs and policies as contributing to closing the gaps in equity. Whilst the array of interventions was no less wide for the present review, there appears to be a small but perceptible shift towards more upstream actions. Examples include trying to affect socioeconomic status by improving education and job opportunities, addressing poverty, improving living and working conditions, particularly housing and the environment, and tackling social exclusion. Although the more traditional health education programs were still evident, there appeared to be stronger efforts to target these at high-risk groups and those with specific needs such as immigrants.
In examining this slight shift towards dealing with the SDH (Figure 1), it is important to consider the context31,32 in which this is taking place. Forty of the 59 responding cities are in EU Member States. Since 2000, a Social Inclusion Process has been in place in the EU, the key challenges of which (tackling child poverty and financial exclusion, making labor markets inclusive, decent housing, overcoming discrimination, and increasing inclusion of people with disabilities, ethnic minorities and migrants) relate to many of the social determinants of health. In 2007, an EC Health Strategy33 was formulated, and equity and solidarity are among its overarching values. According to the EU website on health inequalities34 (information on cross-government strategies, policies, and strategies driven by the health sector and those driven by the nonhealth sector), tackling the social determinants of inequalities in health is now high on the agenda of many EU countries.
Figure 1.
Action to promote equity in health.
The home countries of almost half the responding cities have national level policies or strategies dealing to some extent with the social determinants of equity in health. In the Scandinavian countries, this has been a long-term focus, as in the constituent countries of the UK, where municipalities are closely monitored in relation to national efforts to close the gaps. For the seven cities in Turkey and the six in the Russian Federation, national level policies were also said to be a strong influence.
The tenth international HIA conference held in Rotterdam in 200935 indicated that this potentially powerful tool for promoting the long-term reduction of inequality in health is being rapidly developed across Europe, with a slowly emerging focus on implications for vulnerable groups. Liverpool and Manchester are among the lead cities in the UK for pioneering work on HIA. Belfast is able to take advantage of legislation setting up an Equality Commission, requiring public authorities to carry out equality impact assessments of their policies.36 Pecs seems to be unique in having “health filters” in place in all departments.
Conclusions
The global report of the WHO Commission on Social Determinants of Health, Closing the Gap in a Generation, has reinvigorated debate at national and city levels and has put equity in health higher on the agenda at a European level. It is an overarching value of the health strategy of the European Union, although less evident in relation to EU economic policies. At the international conference marking the end of phase IV of the WHO European Healthy Cities Network in 2008, city mayors signed a declaration reaffirming a commitment to equity which has been woven as a golden thread through all the phases of the project since its inception in 1987. They welcomed their local leadership role in promoting “Health and Health Equity in All Local Policies”.
Yet, in reality, there is compelling evidence that health inequalities are not reducing. The WHO/HABITAT report Hidden Cities37 unmasked great inequities in urban settings across every continent. Mackenbach highlights one of the great disappointments of public health in the persistence socioeconomic inequalities in health even in the highly developed welfare states of Western Europe.38,39 Within the WHO-EHCN, evidence from the author’s evaluations of both phases III40 and IV demonstrate improvements in monitoring inequalities in health and a greater understanding of the need to tackle the socioeconomic determinants. Political commitment is not, however, always translated into processes which, over time, will improve health outcomes and reduce health inequalities.
Armed with this locally generated evidence on barriers and critical success factors, the WHO Regional Office for Europe pledged at the 2009 Annual Business and Technical Meeting Rennes, France, to support network cities in a more rigorous and determined effort to achieve the prerequisites for equity in health. First drafts of new guidance were presented at the 2010 Annual Business and Technical Meeting in Sandnes, Norway. Feedback from cities was incorporated into a revised framework presented at the 2011 Annual Business and Technical Meeting in Liege, Belgium. The final framework for action—Healthy cities tackle the social determinants of inequities in health41—was presented and discussed at the 2012 Annual Business and Technical Meeting in St. Petersburg, Russian Federation. It is complemented by a WHO report on the role of local government in addressing the social determinants of health.42
This guidance on city-based interventions, to tackle the whole gradient health inequalities, draws on international evidence and especially the phase IV evaluation summarized in this article. Action points are, in summary, (a) enhancing local governance and processes for both people and place, (b) increasing institutional capacity to deliver change, (c) improving the knowledge base for measuring and monitoring progress, (d) health equity in all local policies, (e) interventions to sensitize mainstream city services, and (f) special targeted programs. In phase V (2009–2013), a subnetwork of 25 cities is committed to advancing these action points in a systematic and comprehensive way, sharing and synthesizing best practice for decision-makers in Europe and beyond.
Footnotes
Anna Ritsatakis is an Independent Consultant in Health Policy Development
References
- 1.Global strategy for health for all by the year 2000. Geneva, World Health Organization, 1981.
- 2.Whitehead M. Concepts and principles of equity and health. Copenhagen: WHO Regional Office for Europe; 1990. [Google Scholar]
- 3.Dahlgren G, Whitehead M. Policies and strategies to promote equity in health. Copenhagen, WHO Regional Office for Europe, (EUR/ICP/RPD 414(2) 9866n), 1992.
- 4.Kunst AE, Mackenbach J.P. Measuring socio-economic inequalities in health. Copenhagen, WHO Regional Office for Europe, (EUR/ICP/RPD 416 12234), 1994.
- 5.Richard Wilkinson, Michael Marmot (eds) The solid facts Copenhagen, WHO Regional Office for Europe, 1998
- 6.Wilkinson R, Marmot M (eds) The solid facts Copenhagen, WHO Regional Office for Europe, second edition, 2003
- 7.Whitehead M, Dahlgren G. Concepts and principles for tackling social inequities in health: levelling up Part 1. Copenhagen. WHO Regional Office for Europe, Studies on social and economic determinants of population health, No. 2, 2007.
- 8.Dahlgren G, Whitehead M. European strategies for tackling social inequities in health: levelling up Part 2, Copenhagen, WHO Regional Office for Europe, Studies on social and economic determinants of population health, No. 3, 2007
- 9.World Health Organization. Investing in health. A summary of the finding of the Commission on Macroeconomics and Health. Geneva, CMH support unit, WHO. http://www.who.int/macrohealth/infocentre/advocacy/en/investinginhealth02052003.pdf accessed. 26/06/2012.
- 10.World Health Organization. Achieving health equity: from root causes to fair outcomes. Interim statement. Geneva, Commission on Social Determinants of Health, WHO, 2007.
- 11.WHO Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Geneva, World Health Organization, 2008. [DOI] [PubMed]
- 12.WHO Centre for Health Development. Our cities, our health, our future. Acting on social determinants for health equity in urban settings. Report to the WHO CSDH from the knowledge network on urban settings. Kobe City. World Health Organization., 2008
- 13.Interim first report on social determinants of health and the health divide in the WHO European Region Executive summary Copenhagen, WHO Regional Office for Europe, September 2010
- 14.World Health Organization Regional Office for Europe. (eds) Grady, M. & Goldblatt, P. Addressing the social determinants of health: the urban dimension and the role of local government. Copenhagen. WHO. 2012.
- 15.The world health report 1995: bridging the gap. Geneva, World Health Organization, 1995
- 16.Millennium development goals: a compact among nations to end human poverty. New York, Oxford: UNDP, Oxford University Press; 2003. [Google Scholar]
- 17.Bank W. World development report 2000/2001: attacking poverty. Oxford: Oxford University Press; 2001. [Google Scholar]
- 18.European Public Health Alliance, European public health update, No 60, Jan./Feb. 2002, Brussels, p. 19
- 19.World Health Organization. Health21—the health for all policy framework for the WHO European Region. Copenhagen, WHO Regional Office for Europe, 1999.
- 20.Graham H, Kelly P. Health inequalities: concepts, frameworks and policy London, NHS Briefing Paper, Health Development Agency, 2004
- 21.Mackenbach JP, et al. Socioeconomic inequalities in health in Europe. An overview. In: Mackenbach J, Bakker M, et al., editors. Reducing inequalities in health. London Routledge: A European perspective; 2002. [Google Scholar]
- 22.WHO Regional Office for Europe. The ‘Horsens Declaration’ on action for equity in Europe: Mayors’ statement on the WHO Healthy Cities Network in Phase III (1998-2002). Copenhagen. WHO. 2000.
- 23.Draper R, et al. WHO Healthy Cities project: review of the first five years (1987–1992): a working tool and reference framework for evaluating the project. Copenhagen, WHO Regional Office for Europe. (EUR/ICP/HSC 644).1993.
- 24.World Health Organization City health profiles—a review of progress. Copenhagen, WHO Regional Office for Europe, 1998.
- 25.WHO European Centre for Health Policy Health impact assessment. Main concepts and suggested approach. Gothenburg consensus paper, Copenhagen, WHO Regional Office for Europe, European Centre for Health Policy. 1999.
- 26.Welsh Assembly Health impact assessment and government policymaking in European countries: a position report. Survey coordinated by The Welsh Assembly Government, Wales UK, & the European Network of Health Promotion Agencies, Brussels, Cardiff, Public Health Strategy Division, Office of the Chief Medical Officer, Welsh Assembly Government, 2003.
- 27.Ritsatakis A, et al. Exploring health policy development in Europe. (WHO Regional Publications, European Series, No. 86), Copenhagen, WHO Regional Office for Europe. 2000.
- 28.Mielck A, Giraldes M. (eds) Health inequalities. Discussion in Western European countries. Munster/New York, Waxmann, 1994.
- 29.Obertop BY. Equity policy in healthy cities. Master’s thesis (942077). Maastricht, Health Policy and Administration, Faculty of Health Sciences, Maastricht University, 1999.
- 30.Ritsatakis A, et al. Exploring health policy development in Europe. Copenhagen, WHO Regional Office for Europe. (WHO Regional Publications, European Series, No. 86), 2000.
- 31.Navarro V, et al. “The importance of the political and the social in explaining mortality differentials among the countries of the OECD 1950–1998” in. International Journal of Health Services. 2003;33(3):419–94. doi: 10.2190/R7GE-8DWK-YY6C-183U. [DOI] [PubMed] [Google Scholar]
- 32.Strand M, Brown C, Torgersen T, Giaever O. Setting the political agenda to tackle health inequity in Norway Studies on social and economic determinants of population health, No. 4, Copenhagen, WHO Regional Office for Europe, 2009.
- 33.Commission of the European Communities Together for Health: a strategic approach for the EU 2008–2013 Brussels, White Paper COM(2007) 630 final, 23.10.2007
- 34.http://ec.europa.eu/health/social_determinants/videos/index_en.htm accessed 26/06/2012.
- 35.10th International HIA Conference, Rotterdam. 2009 http://www.apho.org.uk/resource/browse.aspx?RID=84239 Accessed 26/06/2012
- 36.Equality Commission. Obligations placed on public authorities to meet the statutory duties in Section 75 of the Northern Ireland Act 1998. The guide to the statutory duties. Revised Draft for Consultation. Revised 2003. Belfast. Equality Commission for Northern Ireland. 2003.
- 37.WHO/UN-HABITAT. Hidden Cities: unmasking and Overcoming Health Inequities in Urban Settings. Geneva. World Health Organization. 2010.
- 38.Machenbach J, et al. Socioeconomic inequalities in health in 22 European countries. New England Journal of Medicine. 2008;23:2468–2481. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- 39.Mackenbach J. The persistence of health inequalities in modern welfare states: the explanation of a paradox. Social Science & Medicine. 2012;75:761–769. doi: 10.1016/j.socscimed.2012.02.031. [DOI] [PubMed] [Google Scholar]
- 40.Ritsatakis A. Equity and social determinants at a city Level. Health Promotion International. 2009;24(s1):i81–i90. doi: 10.1093/heapro/dap058. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization Regional Office for Europe. Healthy cities tackle the social determinants of inequities in health: a framework for action. Copenhagen. WHO. 2012.
- 42.World Health Organization Regional Office for Europe. (eds) Grady, M. & Goldblatt, P. Addressing the social determinants of health: the urban dimension and the role of local government. WHO. Copenhagen 2012.