Abstract
Purpose
The data currently available concerning total ankle arthroplasty (TAA) does not allow valid conclusions in several clinically relevant areas. Total ankle arthroplasty imposes special requirements on the methodology of data collection, evaluation, publication and the assessment of register data.
Methods
We undertook a structured and descriptive analysis of all outcome data available from high-quality national arthroplasty registers worldwide. Register data from Sweden, Finland, Norway, New Zealand and Australia were included in the analysis.
Results
There are marked differences between Europe and Oceania with respect to indications. All data sets show revision rates of approximately 10 % at five years, of which about 40 % of cases are for aseptic loosening. Inlay fractures are relatively common, which indicates potential for the improvement of implants. The documentation of intraoperative surgical errors leading to revision surgery varies significantly among registers. A relevant number of complications are treated without an implant component being exchanged and therefore not covered by a register.
Conclusions
The results of TAA are promising, but the revision rate is higher than for total hip or knee arthroplasty. TAA outcome measurement by means of registers has several specific requirements necessitating additional documentation beyond the basic data set. For methodological reasons the evaluation of results is more complex than for hip or knee arthroplasty. It will therefore be essential to standardise data collection and evaluation and develop a methodology addressing the specific needs of TAA.
Introduction
Over the last few years total ankle arthroplasty has evolved into a standard procedure in the treatment of advanced ankle osteoarthritis. After unacceptably high failure rates had been published for the first generation of implants (mostly ball-and-socket designs) [1–5], the second implant generation achieved marked improvements in outcome [6–8]. Nowadays, for the most part implants of the third generation are used, which feature mobile PE inlays. The publications covering this type of implant usually report satisfactory results and a positive risk–benefit profile for the patient [9–18].
However, a comparison of clinical studies with register data has also revealed shortcomings of clinical studies and limitations as regards conclusions exclusively based on clinical studies [19].
To date there is a relatively small number of published cohorts which exceed 100 patients.
On the other hand, over the last few years the growing number of arthroplasty registers worldwide has lead to an increase in data on total ankle arthroplasty available from this source [20–26].
The aim of this study was to review the most relevant results of worldwide register data, provide supporting information for the interpretation of these data, and summarise those register results that are relevant to everyday patient care.
Materials and methods
A structured review was undertaken of all arthroplasty registers worldwide. To this end, annual reports of national registers, which are summarised on the website of the European Arthroplasty Register (http://www.ear.efort.org/registers.aspx), were searched for data concerning TAA. Moreover, links provided on the individual websites were checked, and a Google search was performed. In addition, publications by members of the steering committees of ankle arthroplasty registers were identified via Medline and the respective abstracts were examined to determine whether the articles were based on register data. Papers which contained a reference to register data were analysed in full text.
All publications providing data on TAA revision rates were included in the analysis.
In one case, the Swedish Total Ankle Register, more than one paper had been published in peer-reviewed journals [21, 24]. The latest publication, which covers the most recent data, was included in our analysis [24]. Since 2011 the Annual Report of the Swedish Register [27] describes the same number of patients as a recent publication, this publication [24] has been used in view of the fact that, contrary to the Swedish-language Annual Report, it is available in English. A descriptive summary and presentation of results is provided.
Data concerning TAA were identified from the national registers of Sweden, Norway, Finland, New Zealand and Australia and included in our analysis [20, 22–26]. The Finnish Register comprises data from 1982 through to 2006, thus being the data set with the longest follow-up worldwide. The unavailability of more recent data may be due to the fact that the organisation responsible for the national register in Finland has been restructured and the procedures of data collection and evaluation had to be newly established from 2006.
The Norwegian Register has been documenting TAA since 1994. For the publication from 2007 [20], data were considered until the end of 2005. Since the Norwegian Register on principle does not publish implant-specific outcome data in its annual reports, more recent data are not available.
The New Zealand Register started regular data collection in the year 2000 and included ankle arthroplasty from the very beginning. The 13-year report covers the data collected until the end of 2011.
According to the common structure of Swedish outcome registers, the Swedish Total Ankle Arthroplasty Register is organised as an independent project within a national network under the strategic management of the Swedish Association of Local Authorities and Regions (SALAR), which also provides the major part of the funding [27]. The published analyses include primary implantations since the year 2003 [24].
The Australian arthroplasty register (AOANJJR – Australian Orthopaedic Association National Joint Replacement Registry) started documentation on 28 July 2006, but most of the departments provided data after the official launch of TAA registration on 15 November 2007. The 2012 report includes data until the end of 2011.
The data sets used for our study comprise a total of 3,348 primary and 472 revision cases (Table 1).
Table 1.
Cases of primary and revision total ankle arthroplasty (TAA) per country
| Country | Primary cases | Revision cases |
|---|---|---|
| Sweden | 780 | 168 |
| Finland | 573 | 59 |
| Norway | 257 | 33 |
| New Zealand | 837 | 64 |
| Australia | 901 | 148 |
| Total | 3348 | 472 |
Results
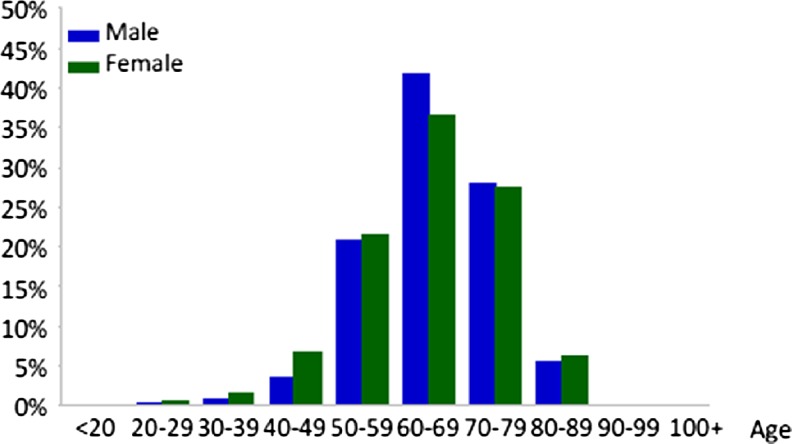
Clinical studies from Europe unfortunately do not include detailed descriptions of the age distribution of the patients treated with total ankle replacement. In New Zealand the average age is 65 years, with a range of 32–88 years. The age pattern in Australia is similar [25, 26] (Fig. 1).
Fig. 1.
Age structure of patients treated with total ankle arthroplasty (TAA) in Australia. Source: AOANJRR Annual Report 2012, total ankle arthroplasty [26]
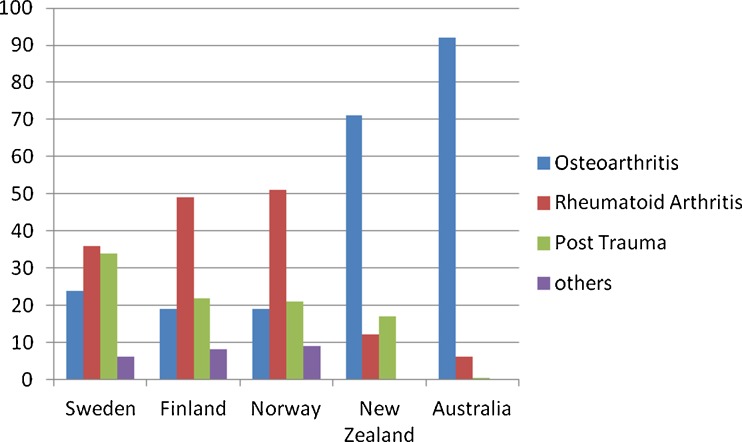
As to the indications for interventions, there are marked differences between Europe and Oceania. Whereas in Scandinavia rheumatoid arthritis, accounting for one third up to half of indications, is the most frequent reason for surgery, only about every tenth patient in New Zealand and only one in sixteen patients in Australia are operated upon for this reason.
The dominant indication in New Zealand and Australia is osteoarthritis. In the comparative interpretation of register data the problematic nature of definitions and documentation practices is a well-known difficulty. This could explain the differences between Australia and the other countries as regards the rate of post-traumatic osteoarthritis. Whereas worldwide a relatively uniform percentage of patients—between 15 and 30 %—undergo surgery for that reason, this indication only appears in 0.3 % of cases in Australia.
Since the decision regarding the extent to which incidents of secondary osteoarthritis after trauma can be causally attributed to the injury leaves ample room for subjective interpretation, definitions in individual countries or habits in documentation practice can lead to essentially different results, even if the patients’ conditions may actually be similar (Fig. 2).
Fig. 2.
Main indications for total ankle arthroplasty (TAA) per country
The average revision rates exhibit considerable differences in the raw data. After five years revision rates slightly exceed the 10 % range in most data sets. This corresponds to the average value from all registers worldwide, with the calculation adjusted for the number of cases and follow-up period [19] (Table 2).
Table 2.
Survival rates per country
| Country | One year | Two years | Three years | Four years | Five years | Six years | Seven years | Ten years |
|---|---|---|---|---|---|---|---|---|
| Sweden | 81 % | 69 % | ||||||
| Finland | 83 % | 78 % | ||||||
| Norway | 89 % | 76 % | ||||||
| New Zealand | 98.8 % | 97.8 % | 96.8 % | 95.6 % | 92.9 % | 90.8 % | 89.5 % | |
| Australia | 96.6 % | 92.7 % | 91.7 % | 89.9 % |
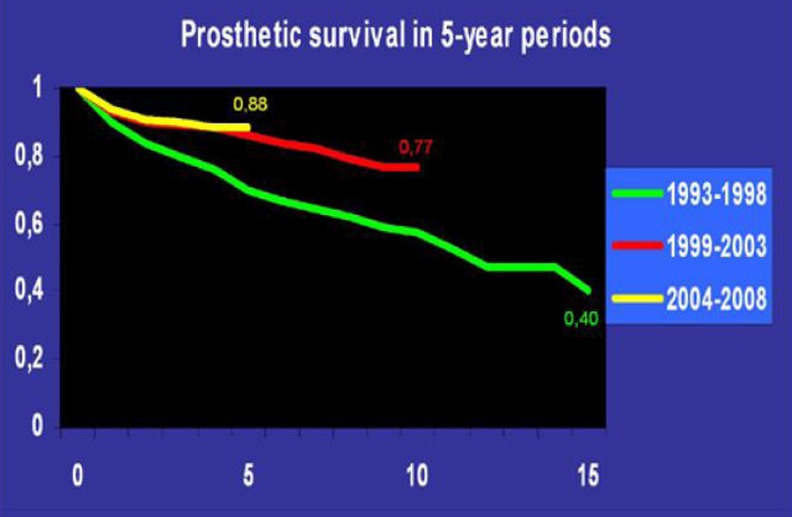
Sweden and Finland show higher revision rates in the raw data. However, in the interpretation it should be taken into account that these data sets feature the longest follow-up periods and hence also include patients whose primary treatment was more than ten years ago.
Considering the fact that the results of interventions performed during the past ten years—which are comparable to the cohorts of the other countries—show markedly superior outcome, the two countries only show minor differences in revision rates [27] (Fig. 3). For that reason also the ten-year revision rates currently available should be interpreted with caution. Improvement of implants, surgical technique, and the concentration of interventions in a smaller number of departments give reason to expect that the outcome in patients operated upon during the past few years will be better.
Fig. 3.
Revision rate of patients in Sweden for various time periods. Source: Swedish Ankle Arthroplasty Register Annual Report 2011 [27]
As to the reasons for revision, aseptic loosening of one or both bone-anchored components is the most frequent cause of failure accounting for approximately 40 % of cases (Table 3). Implant exchange for septic complications is relatively rare at 5–10 %.
Table 3.
Reasons for revision in individual countries
| Country | Aseptic loosening | Instability | Technical failures | Pain | Fracture of inlay | Septic loosening/infection | Periprosthetic fracture |
|---|---|---|---|---|---|---|---|
| Sweden | 40 % | 12.5 % | 11 % | 6.6 % | 10 % | 5 % | |
| Finland | 39 % | 39 % | 8 % | 5 % | 7 % | 1.7 % | |
| Norway | 39 % | 14 % | 21 % | 15 % | 6 % | 6 % | 3 % |
| New Zealand | 41 % | 33 % | 5 % | ||||
| Australia | 41.2 % | 8.1 % | 0.7 % | 3.1 % | 8.1 % | 11.5 % | 3.4 % |
However, the definition of a case that is to be documented by a register refers to the exchange, explantation or re-implantation of at least one part of the implant. A detailed analysis of the patients in the Swedish Register has shown, however, that in addition to 168 revisions documented another 118 secondary procedures had occurred that did not correspond to this definition of failure. Apart from ligament releases, ankle arthrodeses and metatarsal fusions these cases also comprised debridements. In New Zealand further complications were ascertained through patient-reported outcome measure questionaires [22].
These circumstances could also explain the fact that revisions for periprosthetic fractures are relatively rare. This group by definition only includes patients who had parts of the implant changed, which is often unnecessary in the case of malleolar fractures.
Strikingly, the data show a relatively high number of inlay fractures. Even if several registers subsume high wear under this category, this seems alarming especially against the background that the follow-up periods of a high proportion of the patients analysed are five years or less.
Although the data sets analysed include 3,348 primary cases and 472 revisions and are by far larger than any clinical trial, the number of cases is moderate as compared to hip and knee arthroplasty. Therefore even relatively small numbers of cases may change the average results, as becomes evident in a comparison of publications from the New Zealand Register.
A publication from 2007 included 14 revision cases, ten of which were due to aseptic loosening. This corresponded to a rate of 71 %.
The 13-year report published in 2012 already comprised 64 revisions, with 26 revisions resulting from aseptic loosening. The proportion of revisions had declined to 41 % during this period while the share of patients revised for pain only increased to 33 % (Table 4).
Table 4.
Distribution of reasons for revision in New Zealand according to publications in 2007 and 2012
| Source | Aseptic loosening | Technical failures | Pain | Septic loosening/infection | Number of revisions |
|---|---|---|---|---|---|
| 13-year report 2012 | 41 % | 33 % | 5 % | N = 64 | |
| Publication 2007 | 71 % | 7 % | 7 % | 14 % | N = 14 |
Whether this is associated with the results of the publication, which shows that patients with inferior subjective outcome have higher revision rates, can only be discussed theoretically at the moment [22]. However, it seems conceivable that such findings may have led to a more aggressive approach in cases of doubt; surgeons could consequently have reacted to the findings from the register.
A further interesting phenomenon is observed when analysing reasons for revision and assigning them to potential “causer groups”. Whereas surgeons in Scandinavia document between 8 and 21 % of revisions as “technical errors”, this has been the case only once in Australia (0.7 %), in which “incorrect sizing” was chosen as the reason for revision. In the annual report of the New Zealand register this reason is not stated explicitly, and such reasons are not offered as an option in the questionnaire [26].
In a journal publication a case of varus malalignement is mentioned [22]. This could have been documented as free text.
The question as to which extent the surgeon’s expertise influences the result has been examined by several registers [21, 22]. The definitions of experienced surgeons were not uniform though. No statistically significant differences were found between these groups. However, in view of the relatively small cohorts, this may also be due to methodological, i.e. mathematical reasons.
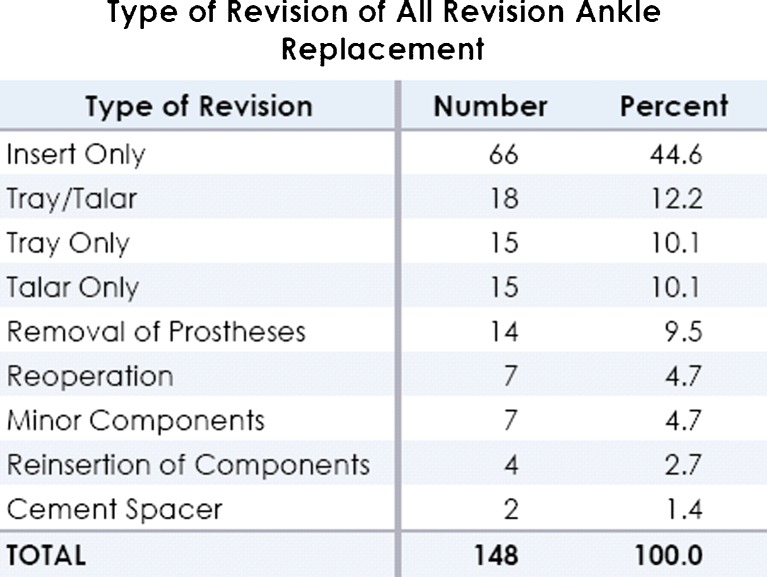
In most sources the description of the operations performed is comparatively superficial. The best documentation is available from the Australian register and shows a high proportion of partial exchanges (Fig. 4).
Fig. 4.
Revisions performed in Australia. Source: AOANJRR Annual Report 2012 [25]
Apart from the usual records for revision procedures some registers include additional information which could be used for interesting evaluations on specific issues in the future. Thus the New Zealand register also records the body mass index. Moreover, ASA classification, documentation of the approach or whether laminar airflow or space suits were used would allow for specific evaluations when sufficient numbers of cases are available. For hip and knee arthroplasty, for example, it has already been reported that laminar airflow and space suits are associated with a higher risk of septic complications [28].
Conclusion
While the results after TAA have not reached the same level as those for hip and knee arthroplasty, the revision rates show that this form of therapy is rational and promising. In a few areas, however, there is evidence of need for improvement.
The large number of inlay fractures is alarming and should be analysed critically. It would therefore be reasonable to undertake further evaluations on an international basis, for instance, as to whether increased complication rates are observed for the thinnest inlays. Similar problems with unicondylar knee implants has led to an increase in the minimum polyethylene thickness recommendation in the past.
It is frequently pointed out that TAA is a challenging surgical procedure requiring a high level of expertise. It would make sense to face up to this topic. Such matters should also be actively queried by registers, since structural improvements can only be achieved through feedback to the surgeon, without provoking a defensive counter-reaction for putting the blame on him.
With regard to the further development of registers and their availability for surgeons and other stakeholders a few basic aspects should be considered in evaluating the data and results.
Registers are a reflection of the circumstances of data collection. The physician in the respective country will usually be aware of these circumstances, but one cannot necessarily assume that this is equally true for every reader of a publication or report. Publications of register data sometimes resemble papers lacking a detailed description of materials and methods, which would hardly be acceptable for clinical studies. However, for register data sets this description is generally difficult and limited, since a specification by inclusion and exclusion criteria is impossible due to the complexity of the situation. Considering the circumstances it would make sense to standardise data collection and definitions.
Hip arthroplasty and—to a lesser extent—knee arthroplasty are relatively well standardised therapies with respect to both the initial situation and the procedure. A serious problem with the implant or associated with the implant almost always results in revision surgery including the exchange of parts of the implant; a case of failure can therefore be ascertained fairly well and safely. Complications which are not covered by routine documentation, for example, when patients cannot be operated upon due to their general condition, are either irrelevant in the context of quality improvement in patient care, very rare, or they typically occur randomly distributed in the control groups. Therefore, they have no relevant limiting impact on the results and aims of a register. This is not equally true for ankle arthroplasty. A number of relevant complications, such as malleolar fractures due to bone structure impairment caused by the implant or during surgery, septic complications or wound healing disorders, are to a significant extent treated without being documented in the register. Conventional register documentation therefore does not cover the entire set of problems, which is why additional documentation appears reasonable.
The comparatively small number of patients facilitates structured follow-up examinations, for example, by means of patient-reported outcome measures (PROMs).
On the one hand, this allows important general conclusions to be drawn, for instance, as regards the correlation between inferior subjective outcome and increased revision rates over time [22]. In the field of arthroplasty such instruments could generally be applied as early warning tools, for example, in the assessment of product innovations.
On the other hand, patients needing more intensive follow-up could be easily identified, which could improve the quality of care while increasing organisational efficiency.
Even now registers represent an important data pool for outcome monitoring in TAA. Owing to the documentation of all surgeries performed in a country and due to the fact that further national registers have started or plan on documenting this type of implants, they will continue to increase in value in the years to come.
Standardised procedures for data collection and the publication of annual reports would be reasonable. Even though sporadic journal publications are useful, they cannot replace publishing outcome quality data in annual reports.
The increasing demand for well-edited register data on the part of physicians and other stakeholders, such as health authorities or manufacturers, should be used as an opportunity to further develop the methodology and increasingly consider the requirements of TAA. This can only be achieved through international co-operation. As an area of manageable size TAA is well-suited to serve as a pilot to further develop outcome research for the benefit of the entire field of arthroplasty.
References
- 1.Bolton-Maggs BC, Sudlow RA, Freeman MA. Total ankle arthroplasty. A long term review of London Hospital experience. J Bone Joint Surg Br. 1985;67:785–790. doi: 10.1302/0301-620X.67B5.4055882. [DOI] [PubMed] [Google Scholar]
- 2.Demottaz JD, Mazur JM, Thomas WH, Sledge CB, Simon SR. Clinical study of total ankle replacement with gait analysis. A preliminary report. J. Bone Joint Surg. (Am) 1979;61:976–988. [PubMed] [Google Scholar]
- 3.Herberts P, Goldie IF, Korner L, Larsson U, Lindborg G, Zachrisson BE. Endoprosthetic arthroplasty of the ankle joint. A clinical and radiological follow up. Acta Orthop Scand. 1982;53:687–696. doi: 10.3109/17453678208992277. [DOI] [PubMed] [Google Scholar]
- 4.Kitaoka HB, Patzer GL. Clinical Results of Mayo total ankle arthroplasty. J Bone Joint Surg. (Am) 1996;78:1658–1664. doi: 10.2106/00004623-199611000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Takamura Y, Tanaka Y, Kumai T, Sugimoto K, Ohgushi H. Ankle arthroplasty using three generations of metal and ceramic prostheses. Clin. Orthop. 2004;4242:130–136. doi: 10.1097/01.blo.0000131246.79993.ec. [DOI] [PubMed] [Google Scholar]
- 6.Conti SF, Wong YS. Complications in total ankle replacements. Clin. Orthop. 2001;391:105–114. doi: 10.1097/00003086-200110000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Knecht SI, Estin M, Callaghan JJ, Zimmermann MB, Alliman KJ, Alvine FG, Salzmann CL. The agility total ankle arthroplasty. Seven to sixteen year follow up. J Bone Joint Surg (Am) 2004;86:1167–1171. [PubMed] [Google Scholar]
- 8.Spirt AA, Assal M, Hansen ST., Jr Complications and failures after total ankle arthroplasty. J Bone Joint Surg (Am) 2004;86:1172–1178. doi: 10.2106/00004623-200406000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Anderson T, Montgomery F, Carlsson A. Uncemented STAR total ankle prostheses. Three to eight-year follow up of fifty-one consecutive ankles. J. Bone Joint Surg (Am) 2003;85:1321–1329. [PubMed] [Google Scholar]
- 10.Buechel FF, Sr, Buechel FF, Jr, Pappas MJ. Ten year evaluation of cementless Buechel-Pappas meniscal bearing total ankle replacement. Foot Ankle Int. 2003;24:462–472. doi: 10.1177/107110070302400603. [DOI] [PubMed] [Google Scholar]
- 11.Kofoed H. Scandinavian total ankle replacement (STAR) Clin Orthop. 2004;424:73–79. doi: 10.1097/01.blo.0000132414.41124.06. [DOI] [PubMed] [Google Scholar]
- 12.Valderrabano V, Hintermann B, Dick W. Scandinavian total ankle replacement: a 3.7-year average follow up 65 patients. Clin Orthop. 2004;424:47–56. doi: 10.1097/01.blo.0000132245.18548.09. [DOI] [PubMed] [Google Scholar]
- 13.Doets HC, Brand R, Nelissen RG. Total ankle arthroplasty in inflammatory joint disease with use of two mobile bearing designs. J Bone Joint Surg Br. 2006;83:579–586. doi: 10.2106/JBJS.E.00414. [DOI] [PubMed] [Google Scholar]
- 14.Wood PL, Deakin S. Total ankle replacement. The results of 200 ankles. J Bone Joint Surg Br. 2003;65:334–341. doi: 10.1302/0301-620X.85B3.13849. [DOI] [PubMed] [Google Scholar]
- 15.Stengel D, Bauwens K, Ekkerkamp A, Cramer J. Efficacy of total ankle replacement with medical bearing devices: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2005;125:109–119. doi: 10.1007/s00402-004-0765-3. [DOI] [PubMed] [Google Scholar]
- 16.Wood P, Prem H, Sutton C. Total ankle replacement. Mid term results in 200 Scandinavian total ankle replacements. J Bone Joint Surg. 2008;90(5):605–609. doi: 10.1302/0301-620X.90B5.19677. [DOI] [PubMed] [Google Scholar]
- 17.Wood P, Sutton C, Mishra V, Suneja RA. A randomized controlled trial of two mobile bearing total ankle replacements. J Bone Joint Surg Br. 2009;91:69–74. doi: 10.1302/0301-620X.91B1.21346. [DOI] [PubMed] [Google Scholar]
- 18.Wood P, Karski M, Watmough P. The results of 100 mobility total ankle replacements. J Bone Joint Surg Br. 2010;92(7):958–962. doi: 10.1302/0301-620X.92B7.23852. [DOI] [PubMed] [Google Scholar]
- 19.Labek G, Thaler M, Janda W, Agreiter M, Stöckl B. Revision rates after total joint replacements: cumulative results from worldwide joint register datasets. J Bone Joint Surg Br. 2011;93(3):293–7. doi: 10.1302/0301-620X.93B3.25467. [DOI] [PubMed] [Google Scholar]
- 20.Fevang BS, Lie SA, Havelin SA, Brun JG, Skredderstuen A, Furnes O. 257 ankle arthroplasties performed in Norway between 1994 and 2005. Acta Orthop. 2007;78(5):575–583. doi: 10.1080/17453670710014257. [DOI] [PubMed] [Google Scholar]
- 21.Henricson A, Skoog A, Carlsson A. The Swedish Ankle Arthroplasty Register: an analysis of 531 arthroplasties between 1993 and 2005. Acta Orthop. 2007;78(5):569–574. doi: 10.1080/17453670710014248. [DOI] [PubMed] [Google Scholar]
- 22.Hosman AH, Mason RB, Hobbs T, Rothwell AG. A New Zealand national joint registry review of 202 total ankle replacements followed for up to 6 years. Acta Orthop. 2007;78(5):584–591. doi: 10.1080/17453670710014266. [DOI] [PubMed] [Google Scholar]
- 23.Syttä E, Koivu H, Eskelinen A, Ikävalko M, Paavolainen P, Remes V. Total ankle replacement: a population based study of 515 cases from the Finnish arthroplasty register. Acta Orthop. 2010;81:114–118. doi: 10.3109/17453671003685459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Henricson A, Nilsson JA, Carlsson A. 10-year survival rate of total ankle arthroplasties: a report on 780 cases from the Swedish Ankle Register. Acta Orthop. 2011;82(6):655–659. doi: 10.3109/17453674.2011.636678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.No authors listed (2012) AOA National Joint Replacement Registry, Supplementary Annual Report 2012 Demographics and Outcome of Ankle Arthroplasty https://aoanjrr.dmac.adelaide.edu.au/. Accessed 07 May 2013
- 26.No authors listed (2012) 13th Year Report New Zealand Joint Registry http://www.cdhb.govt.nz/NJR. Accessed 07 May 2013
- 27.No authors listed (2012) Annual Report 2011 Swedish Ankle Arthroplasty Register [Swedish] http://www.swedankle.se/index.php?l=1. Accessed 07 May 2013
- 28.Hooper GJ, Rothwell AG, Frampton C, Wyatt MC (2011) Does the use of laminar flow and space suits reduce early deep infection after total hip and knee replacement?The 10 years results from the New Zealand Joint Registry. J Bone Joint Surg (Br) 93(1):85–90 [DOI] [PubMed]