Abstract
Purpose
The purpose of this study was to compare results of partial proximal fasciotomy (PPF) with proximal medial gastrocnemius release (PMGR) in the treatment of chronic plantar fasciitis (CPF).
Method
This retrospective study compares 30 patients with CPF that underwent PPF with 30 that underwent isolated PMGR. Both groups were matched in terms of previous treatments and time from onset of symptoms to surgery. Different standardised evaluation scales (VAS, Likert, AOFASh) were used to evaluate results.
Results
Plantar fasciotomy had satisfactory results in just 60 % of patients, with an average ten weeks needed to resume work and sports. Patient satisfaction in the PMGR group reached 95 %, being back to work and sports at three weeks on average. Functional and pain scores were considerably better for PMGR and fewer complications registered.
Conclusion
In our series, isolated PMGR is a simple and reliable procedure to treat patients with CPF. It provides far better results than conventional fasciotomy with less morbidity and better patient satisfaction, and thus has become our surgical procedure of choice in recalcitrant CPF.
Introduction
Plantar fasciitis is a common foot condition treated by orthopaedic surgeons and is prevalent in both athletic and nonathletic populations [1].
The specific cause of plantar fasciitis is poorly understood and is multifactorial. Numerous interventions have been described for the treatment of plantar fasciitis, but few high-quality randomised controlled trials have been conducted to support these therapies. Chronic plantar fasciitis is a self-limiting condition that responds to conservative treatment in almost 90 % of patients within nine months from onset of symptoms. When conservative management fails, PPF is the most common surgical procedure performed. But success rates following plantar fascia release are variable.
Altered leg and foot biomechanics can play a role in the pathogenesis of plantar fasciitis. A tight gastrocnemius may not allow for a full “knee extension–ankle dorsiflexion couple” at the end of the second rocker of gait. The risk of developing CPF seems to be increased in patients with reduced ankle dorsiflexion [2].
In our experience, the majority of patients suffering from CPF have isolated gastrocnemius tightness. Since 2009, we have performed an isolated release of the proximal medial head of the gastrocnemius to treat recalcitrant CPF.
A retrospective study was design to assess the efficacy of PMGR for the treatment of recalcitrant CPF, and to compare its outcome with the outcome of proximal partial plantar fasciotomy. To our knowledge, this is the first report to compare PPF with PMGR.
Materials and methods
We retrospectively reviewed 60 patients who had undergone surgery for CPF over a four-year period. Thirty patients had an isolated open PPF and 30 had an isolated PMGR.
Plantar fasciitis was diagnosed clinically but all patients had plain foot and ankle X-rays and MRI. The indications for operative intervention were continued unremitting pain for more than nine months and failure of nonoperative treatments. Exclusion criteria were systemic inflammatory disease, and suspicion of tibialis posterior or Baxter’s neuropathy.
The study population consisted of:
Group 1: PPF comprised 30 patients; mean age was 42 years (range, 22–61 years), 18 men and 12 women, and duration of symptoms was 13 months on average (range, 9–62 months).
Group 2: PMGR comprised 30 patients; mean age was 44 years (range, 21–63 years), 16 men and 14 women, and duration of symptoms was 14 months on average (range, 10–64 months).
In both groups, previous conservative treatments were registered. They all had had blood tests to rule out inflammatory diseases.
Gastrocnemius tightness was assessed clinically by using the Silfverskiöld test [3]. With the examiner maintaining the foot in complete inversion (to avoid potential dorsiflexion in the midtarsal joints) the knee is flexed and extended. If ankle dorsiflexion is unchanged throughout knee range of movement, there is Achilles tendon tightness. If the lateral border of the foot cannot be made plantigrade with respect to the border of the fibula when the knee was extended, there is a short gastrocnemius present.
Pain was evaluated using a visual analogue scale (VAS) (from 0—no pain to 100—maximal pain) at baseline, four weeks, 12 weeks, six months, and 12 months postoperative. The American Orthopaedic Foot and Ankle-Hindfoot Scale (AOFASh) was also used (pain 40 points, function 50 points, alignment 10 points) at baseline, four weeks, 12 weeks, six months, and 12 months.
Other variables were also analysed: ability to autonomous comfortable plantigrade weighbearing postoperatively, calf power, time to improvement with respect to preoperative condition, return to conventional shoes, and return to work and sports.
Patient subjective assessment included patient satisfaction, recommendation to a friend, and likelihood to undergo the same procedure again if they had CPF on the contralateral foot. Likert scale was used for the evaluation of treatment success. No outcome tools have been validated for CPF, but the Likert scale is a patient-reported outcome satisfaction scale which has been used in other studies [4]. Calf power was analysed objectively by asking patients to perform a one-minute single stance heel rise test on the operated side, at three and six months from surgery. Postoperative complications were also recorded.
Surgical techniques
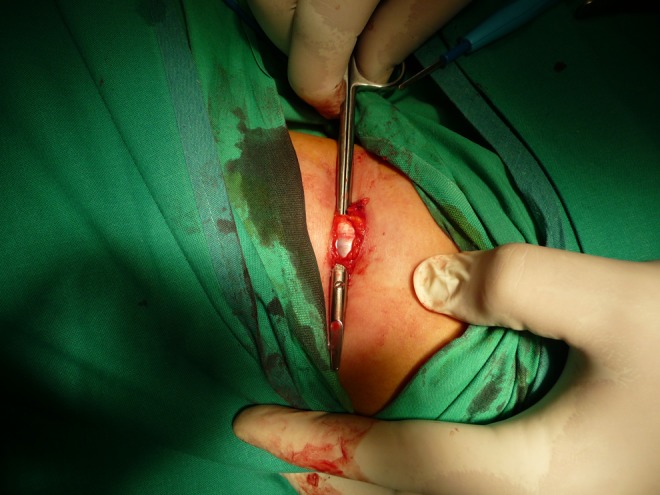
Partial fasciotomy was performed with the patient positioned supine with a tourniquet under spinal anesthesia. A 4-cm incision was made at the medial proximal aspect of plantar fascia, at around three centimetres distal to the calcaneal insertion. The fascia is exposed (Fig. 1) and the medial third released (Fig. 2). Skin was closed with absorbable sutures and a bulky foot compression dressing used for 24 hours, followed by adhesive dressing.
Fig. 1.

Proximal plantar fascia exposure
Fig. 2.

Section of the medial third of the proximal plantar fascia
Release of the proximal medial head of the gastrocnemius was performed with the patient positioned prone under spinal or local anesthesia. No tourniquet was used. A four centimetre incision at the medial crease of the popliteal fossa allowed for the division of the superficial fascia (Fig. 3). A blunt instrument was used to expose the proximal medial head of the gastrocnemius (Fig. 4) and the aponeurosis was divided (Fig. 5). The aponeurosis was then cut with a scalpel while exerting ankle dorsiflexion so that both ends separate. Special attention was paid to the complete semicircumferential release at the anterior aspect of the medial head of the gastrocnemius. Palpation of any residual tightness was of help to assess a potential incomplete recession. Increased ankle dorsiflexion was checked and skin was closed with absorbable sutures. A small adhesive dressing was applied.
Fig. 3.

Incision planning for proximal medial gastrocnemius release (PMGR) at the medial popliteal fossa
Fig. 4.
Exposure of the proximal medial head of the gastrocnemius with a blunt instrument
Fig. 5.

Division of the aponeurosis
In the postoperative period, full weightbearing was allowed as tolerated in both groups. A postoperative open shoe was used for the first two weeks and conventional footwear encouraged from the second week. Eccentric calf stretching exercises were reinitiated as soon as tolerated and maintained five minutes daily for six weeks in both groups.
Final follow-up was 12 months in both groups (range, 12–36 months).
Results
Sixty patients were included in this study. The two groups were comparable with respect to age, sex, height, weight, body mass index (BMI), duration of symptoms, previous treatments, and previous sport activity. The characteristics of patients are shown in Table 1.
Table 1.
Characteristics of patients included in the study. Values are medians, number of patients and percentages
| Characteristics | PPF | PMGR |
|---|---|---|
| Female | 12 (40 %) | 14 (46.7 %) |
| Age | 42 (22–61) | 44 (21–63) |
| Mean height (m) | 1.64 (1.52–1.80) | 1.69 (1.53–1.86) |
| Mean body weight (kg) | 80 (58–115) | 82 (61–108) |
| Body mass index | 28.3 (24–33) | 29.3 (26–32) |
| Duration of symptoms, months | 13 (9–62) | 14 (10–64) |
| Previous rehab stretching | 30 (100 %) | 30 (100 %) |
| Previous cortisone injection | 12 (40 %) | 15 (50 %) |
| No sport habits preinjury | 10 (33.3 %) | 10 (33.3 %) |
| Amateur sports preinjury | 20 (66.7 %) | 18 (60 %) |
| Pro athlete preinjury | 0 (0 %) | 2 (6.7 %) |
PPF partial proximal fasciotomy, PMGR proximal medial gastrocnemius release
Patients in the fasciotomy group had their mean VAS scores reduced from 8.1 preoperatively to 4.5 at six months and 3.1 at 12 months. AOFASh scores improved from a mean 48 preop to 55 at six months and 66 at 12 months.
PMGR had a profound and lasting effect on the mean VAS and AOFASh scores of patients. Mean VAS scores were reduced after PMGR from 8.2 preoperatively to 1.8 at six months and 0.9 postoperatively at 12 months. AOFASh scores improved from a mean 46 preop to 85 at six months and 90 at 12 months.
It is interesting to note that about 20 % of those who improved with PMGR in our study did so within one week of surgery, about 60 % between weeks one and eight, and the remaining 20 % of improvements did so between the second and the sixth months from surgery. In the PPF group, none of the patients noticed improvement within six weeks of their surgery.
At one year, patient satisfaction in the PPF group was excellent in 10 % of cases, good in 30 %, satisfactory in 20 %, and poor in 40 %. In the PMGR group 80 % of patients were excellent, 10 % considered to be good, 5 % satisfactory, and 5 % poor.
In terms of postoperative success, Likert scale showed none of the patients had worsening of their symptoms after PMGR, but two patients reported to be worse following PPF. There were 24 pain-free heels in the PMGR group, whereas only ten patients were free of all pain in the PPF group (Table 2).
Table 2.
Postoperative success. Likert scale
| Change in symptoms | PPF | PMGR |
|---|---|---|
| Worsening | 2 | 0 |
| No change | 2 | 1 |
| Moderately better | 6 | 2 |
| Much better | 10 | 3 |
| Pain free | 10 | 24 |
PPF partial proximal fasciotomy, PMGR proximal medial gastrocnemius release
In the postoperative period, comfortable full weightbearing was achieved one week after PMGR, but it took over four weeks in all patients who underwent PPF. Comfortable eccentric calf stretching exercises were initiated at two weeks on average in the PMGR group and at nine weeks in the PPF group.
Return to previous work activities was achieved at an average of 12 weeks (range, 4–24 weeks) at the PPF group. Two patients who underwent a fasciotomy had not returned to their previous occupation at the end of the study (24 and 27 months from surgery). Patients in the PMGR group were able to work again at three weeks on average (range, 1–12 weeks). Return to previous sports activities was achieved at 16 weeks on average in the PPF group, with two patients unable to return to previous sports habits. In the PMGR group, sports resumption was achieved at five weeks on average, with all patients returning to their previous activities.
Conventional shoes were worn immediately after surgery in patients that underwent a PMGR, but took six weeks on average for patients that underwent PPF. Calf power was assessed by the one minute single-leg heel-raise test at three and six months postoperatively.
Forty-five percent of patients in the PPF group would recommend the procedure to a close friend, and 35 % would undergo the same surgery if they had a recalcitrant CPF in the contralateral foot. Ninety-five percent of patients in the PMGR would recommend the procedure and 95 % would undergo surgery for their contralateral leg.
In the PPF, complications included one case of plantar nerve neuroapraxia (that resolved uneventfully), five painful scars, and one superficial infection with wound dehiscence (that responded to conservative treatment). In the PMGR, the only complication registered was a calf haematoma in a patient with varicose veins that needed no treatment.
Discussion
Management of CFP is often difficult and frustrating. The choice of treatment for each patient is mainly based on the orthopaedic surgeon’s personal experience. Around 80–90 % of patients improve to achieve satisfaction within the first nine months from onset of symptoms. But around 10 % of patients are unresponsive to conservative methods.
Numerous treatments have been advocated for the management of CPF, including rest, stretching protocols, non-steroidal anti-inflammatory medication, manual therapy, heel pads, orthotics, taping, night splints, extracorporeal shock wave therapy, steroid injections and platelet rich plasma injections [5, 6].
In chronic cases, histological analysis shows no signs of inflammatory cell invasion around the fascia. The tissue instead is infiltrated with macrophages, lymphocytes, plasma cells, immature vascularisation and fibrosis [7]. These findings possibly explain the variable results encountered for conservative treatments of CPF.
Until recently, little attention has been paid to altered biomechanics around the gastrocnemius-soleus-Achilles-calcaneal-plantar fascia complex as contributor to CPF [8]. However, calf muscle stretching provides a small and statistically significant increase in ankle dorsiflexion [9]. The continuity of connective tissue between the Achilles tendon and the plantar fascia, and the fact that decreased ankle dorsiflexion is a risk factor in the development of plantar fasciitis, provides some justification for calf stretching [10].
In some difficult cases, symptoms persist despite all efforts at nonoperative intervention; thus, surgery may be indicated [11]. Surgical management of plantar fasciitis has traditionally consisted in an open proximal partial fasciotomy. Endoscopic plantar fascia release is an alternative to conventional open fasciotomy but concerns with endoscopic release are poor visualisation and the possibility of unintended complete release [12]. Surgical release of the plantar fascia may have implications for foot biomechanics as the windlass effect may be altered after surgery [8].
For both the open and the endoscopic techniques, there are risks of plantar fascia rupture, wound complications, lateral column pain, and plantar nerve injury [13]. Although a great deal of the early literature on this procedure touted excellent results, a more critical review of the findings leaves many questions unanswered. Success rates are variable with prolonged postoperative rehabilitation needed in most cases. In some series, less than 50 % of patients who had a surgical procedure for heel pain were completely satisfied with the results [14].
Gastrocnemius shortening has been implicated in several foot and ankle conditions, including plantar fasciitis, Achilles non-insertional tendinopathies, and second-rocker metatarsalgia [10, 15]. The clinical test to assess isolated gastrocnemius tightness was described by Silfverskiöld. Isolated gastrocnemius tightness has been associated with failure of conservative measures [16]. Plantar fascia tension was directly proportional to Achilles tendon tension in cadavers in dynamic gait stimulator [17]. Carlson et al. found that increasing tension within Achilles tendon caused increase in plantar fascia tension at four different angles of MPJ dorsiflexion [8]. Biomechanics is believed to contribute to the onset of this condition through a decreased ankle joint range of motion. Reduced dorsiflexion of the ankle is the most important risk factor for the development of CPF [18].
Many techniques have been described for the operative treatment of isolated gastrocnemius tightness. The different techniques are classified according to their anatomical level. Releasing the aponeurosis of the proximal gastrocnemius through a medial approach may put the saphenous nerve and greater saphenous vein at risk [19]. A more distal approach, at the musculotendinous junction, has been successful in the improvement of CFP [15]. The conventional Strayer procedure may put the sural nerve at risk and occasionally have poor cosmetic results. It also needs leg casting [19].
A more proximal release, with the division of the aponeurosis of both heads of the gastrocnemius through a single transverse incision over the back of the knee, has been used to treat CPF [20]. More recently this technique has been modified so that only the medial head of the gastrocnemius is released through a small posterior incision, placed more medially [4]. Additionally, the approach to the medial head was less likely to risk cutaneous nerve damage. The medial head was found to be much larger in both the muscular and aponeurotic components than the lateral head in all specimens. On average the cross-sectional area of the aponeurosis of the medial head of gastrocnemius was 2.4 times the cross-sectional area of the aponeurosis of the lateral head [21]. The medial head is supposed to account for most of the gastrocnemius tightness.
In a prospective study, the PMGR has shown excellent results in the treatment of recalcitrant plantar fasciitis [4]. Our results in the PMGR group are almost identical.
Good results obtained with either PPF or PMGR might be due to a prolonged period of unloading and reloading. But this is not the case for PMGR in which patients are allowed immediate weightbearing as tolerated postoperatively.
There might be concern over a potential loss of calf power following PMGR [22]. We did not observe any loss of calf power in our study group. Two of the patients were professional athletes and returned to previous sports activities uneventfully.
There might be evidence for a biomechanical approach to the treatment of CPF. It is important to explore gastrocnemius tightness in patients with no response to conservative management. PPF may disturb normal plantar fascia function and the potential effects on foot and ankle biomechanics are unpredictable. PMGR seems to be a more rational approach to the surgical treatment of CPF when compared to PPF.
Conclusion
Tight/short gastrocnemius was found to be significant to develop refractory CPF. All of our patients with CPF had gastrocnemius contracture. Isolated gastrocnemius proximal-medial recession was safe and effective. Conventional PPF compares poorly to PMGR in terms of success and patient satisfaction. The results of the present study have made us change our approach to surgical treatment of CPF, with PMGR becoming our procedure of choice and fasciotomy only considered in rare cases of gastrocnemius proximal-medial release failure.
References
- 1.Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004;25:303–310. doi: 10.1177/107110070402500505. [DOI] [PubMed] [Google Scholar]
- 2.Aronow MS, Diaz-Doran V, Sullivan RJ, Adams DJ. The effect of triceps surae contracture force on plantar foot pressure distribution. Foot Ankle Int. 2006;27:43–52. doi: 10.1177/107110070602700108. [DOI] [PubMed] [Google Scholar]
- 3.Silfverskiöld N. Reduction of the uncrossed two-joint muscles of the leg to one joint muscles in spastic conditions. Acta Chir Scand. 1923;56:315–330. [Google Scholar]
- 4.Abbassian A, Kohls-Gatzoulis J, Solan MC. Proximal medial gastrocnemius release in the treatment of recalcitrant plantar fasciitis. Foot Ankle Int. 2012;33(1):14–19. doi: 10.3113/FAI.2012.0014. [DOI] [PubMed] [Google Scholar]
- 5.LaFuente AG, O’Mullony IM, Escriba M, Cura-Iriarte P. Plantar fasciitis: evidence-based review of treatment. Reumatol Clin. 2007;3(4):159–165. doi: 10.1016/S1699-258X(07)73614-8. [DOI] [PubMed] [Google Scholar]
- 6.Martinelli N, Marinozzi A, Carni S, Trovato U, Bianchi A, Denaro V. Platelet-rich plasma injections for chronic plantar fasciitis. Int Orthop. 2013;37(5):839–842. doi: 10.1007/s00264-012-1741-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lemont H, Ammirati KM, Usen N. Plantar fasciitis. A degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93(3):234–237. doi: 10.7547/87507315-93-3-234. [DOI] [PubMed] [Google Scholar]
- 8.Carlson RE, Fleming LL, Hutton WC. The biomechanical relationship between the tendoachilles, plantar fascia and metatarsophalangeal joint dorsiflexion angle. Foot Ankle Int. 2000;21:18–25. doi: 10.1177/107110070002100104. [DOI] [PubMed] [Google Scholar]
- 9.Radford JA, Burns J, Buchbinder R, Landorf KB, Cook C. Does stretching increase ankle dorsiflexion range of motion? A systematic review. Br J Sports Med. 2006;40:870–875. doi: 10.1136/bjsm.2006.029348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DiGiovanni CW, Kuo R, Tejwani N, Price R, Hansen ST, Jr, Cziernecki J, Sangeorzean BJ. Isolated gastrocnemius tightness. JBJS. 2002;84(A):962–970. doi: 10.2106/00004623-200206000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Sammarco GJ, Helfrey RB. Surgical treatment of recalcitrant plantar fasciitis. Foot Ankle Int. 1996;17:520–526. doi: 10.1177/107110079601700902. [DOI] [PubMed] [Google Scholar]
- 12.Bader L, Park K, Gu Y, O’Malley MJ. Functional outcome of endoscopic plantar fasciotomy. Foot Ankle Int. 2012;33(1):37–43. doi: 10.3113/FAI.2012.0037. [DOI] [PubMed] [Google Scholar]
- 13.Kinley S, Frascone S, Calderone D, Wertheimer SJ, Squire MA, Wiseman FA. Endoscopic plantar fasciotomy versus traditional heel spur surgery: a prospective study. J Foot Ankle Surg. 1993;32:595–603. [PubMed] [Google Scholar]
- 14.Davies MS, Weiss GA, Saxby TS. Plantar fasciitis: how successful is surgical intervention? Foot Ankle Int. 1999;20:803–807. doi: 10.1177/107110079902001209. [DOI] [PubMed] [Google Scholar]
- 15.Maskill JD, Bohay DR, Anderson JG. Gastrocnemius recession to treat isolated foot pain. Foot Ankle Int. 2010;31:19–23. doi: 10.3113/FAI.2010.0019. [DOI] [PubMed] [Google Scholar]
- 16.Patel A, DiGiovanni B. Association between plantar fasciitis and isolated contracture of the gastrocnemius. Foot Ankle Int. 2011;32:5–8. doi: 10.3113/FAI.2011.0005. [DOI] [PubMed] [Google Scholar]
- 17.Erdimir A, Hamel AJ, Fauth AR, Piazza SJ, Sharkey NA. Dynamic loading of the plantar aponeurosis in walking. JBJS. 2004;86(A):546–552. doi: 10.2106/00004623-200403000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for plantar fasciitis: a matched case–control study. J Bone Joint Surg Am. 2003;85:872–877. doi: 10.2106/00004623-200305000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Herzenberg JE, Lamm BM, Corwin C, Sekel J. Isolated recession of the gastrocnemius muscle: the Baumann procedure. Foot Ankle Int. 2007;28:1154–1159. doi: 10.3113/FAI.2007.1154. [DOI] [PubMed] [Google Scholar]
- 20.Barouk LS, Barouk P, Toulec E. Resulltats de la liberation proximale des gastrocnemiens. Etude prospective symposium “Brieveté des gastrocnemiens”, journées de Printemps SFMCP-AFCP, Toulouse. Med Chir Pied. 2006;22:151–156. [Google Scholar]
- 21.Hamilton PD, Brown M, Ferguson N, Adebibe M, Maggs J, Solan MC. Surgical anatomy of the proximal release of the gastrocnemius: a cadaveric study. Foot Ankle Int. 2009;30(12):1202–1206. doi: 10.3113/FAI.2009.1202. [DOI] [PubMed] [Google Scholar]
- 22.Chimera NJ, Castro M, Manal K. Function and strength following gastrocnemius recession for isolated gastrocnemius contraction. Foot Ankle Int. 2010;31(5):377–384. doi: 10.3113/FAI.2010.0377. [DOI] [PubMed] [Google Scholar]


