Abstract
Purpose
Several bony and soft tissue procedures have been described for the treatment of hallux valgus, and currently mini-invasive surgical techniques are preferred in order to reduce surgical trauma, complications, time of surgery and to allow an earlier recovery. The aim of this study is to analyse a series of 1,000 consecutive cases of hallux valgus, surgically treated by the minimally invasive SERI technique, reporting results at mid-term follow-up.
Methods
We prospectively studied 641 patients (1,000 feet) with symptomatic hallux valgus surgically treated by SERI osteotomy. Inclusion criteria were: age between 20 and 65 years, reducible mild or moderate hallux valgus, HVA ≤ 40°, IMA ≤ 20°, and arthritis of the first metatarsophalangeal joint up to grade 2 according to the Regnauld classification.
Results
The American Orthopaedic Foot and Ankle Society (AOFAS) score rose from 46.8 ± 16.7 preoperatively to 89 ± 10.3 at last follow-up. Radiographic control at follow-up showed a complete healing of the osteotomy and remodelling of the metatarsal bone. Low rate of complication has been reported.
Conclusions
This study demonstrated that the SERI technique is effective in treating mild to moderate hallux valgus in terms of relief from symptoms and functional improvement. This technique allowed correction of the main parameters of the deformity, with durable clinical and radiographic results at a mid-term follow-up.
Electronic supplementary material
The online version of this article (doi:10.1007/s00264-013-1980-8) contains supplementary material, which is available to authorized users.
Keywords: Hallux valgus, SERI, Osteotomy, Early metatarsophalangeal arthritis
Introduction
Hallux valgus is a deformity of the forefoot, characterised by lateral displacement of the great toe, associated to medial displacement of the first metatarsal bone, with progressive subluxation of the first metatarsophalangeal joint. The lateral deviation of the first toe is considered pathological when the angle between the long axis of the hallux and the long axis of the first metatarsal bone is greater than 15° [1–3].
Hallux valgus is often bilateral and it affects most frequently adult women, especially after the sixth decade [4, 5]. Rarely, also young people and children can be affected by this condition [4]. Several authors have tried to assess pathogenesis and risk factors, which include biomechanical, genetic and familial factors [1–20]; however, the end point is impairment of the normal function of the first metatarsophalangeal joint. Clinical symptoms include pain and reduced range of motion of the first metatarsophalangeal joint, where bursitis or callosities are often present. Moreover, the reduced function of the hallux during gait may provoke transfer metatarsalgia and also progressive deformities involving the lesser toes such as hammer toes or claw toes.
The main goal of surgical correction of hallux valgus is the morphological and functional rebalance of the first metatarsophalangeal joint and the first ray, correcting the pathological anatomy and the pathological function of the deformity. Several bony and soft tissue procedures have been described for the treatment of hallux valgus [21–41]. Currently, a mini-invasive surgical approach is preferred in order to reduce surgical trauma, complications, time of surgery and to allow an earlier recovery [11, 22, 32, 36, 39, 42, 43]. Historically, distal metatarsal osteotomies have been indicated in cases of mild or moderate deformity with an intermetatarsal angle (IMA) up to 15–20° [1, 29, 36, 44, 45]. Distal osteotomies may also be used to correct deformities characterised by deviation of the distal metatarsal articular angle (DMAA) or to address concomitant stiffness [24, 46].
Many authors over the years have described several techniques for hallux valgus correction by the performance of a distal first metatarsal osteotomy; each technique is characterised by different surgical approach, osteotomy design and fixation device [15, 21, 22, 33–37, 41, 47, 48]. Most surgical techniques are associated with more than 80 % good outcomes, but none is considered as entirely satisfactory or superior to the others [24, 36, 49]. In 1998, the senior author (SG) designed a minimally invasive technique for hallux valgus correction whose characteristics were summarised in the acronym SERI: simple, effective, rapid and inexpensive [29, 50, 51]. The SERI technique was not a completely new technique, since it consisted of a linear osteotomy at the metatarsal neck level as described by Hohmann [15], Wilson [41] and Magerl [35]. It is stabilised by one Kirschner wire as reported by Bosch [22], Lamprecth and Kramer [33], and it is not performed percutaneously but under direct vision through a small medial incision.
The aim of this prospective study was to analyse the results of a series of the first 1,000 consecutive feet operated upon for hallux valgus correction using the SERI technique, in order to determine (1) whether the SERI technique is effective for treating symptomatic hallux valgus, (2) whether the efficacy of the procedure is maintained over time and (3) to evaluate the complications related to this technique.
Materials and methods
Inclusion criteria and patient population
We prospectively studied 641 patients (61 men and 580 women) with symptomatic hallux valgus surgically treated by SERI osteotomy between 1998 and 2003. Foot involvement was bilateral in 359 patients, and unilateral in the other 282, for a total of 1,000 feet, that was considered the endpoint of the study. The study was authorised by the ethical committee of the authors’ institution; all the patients knew that it was an experimental procedure and gave their informed consent for inclusion in the study and report of outcomes.
Inclusion criteria for study enrolment were: (1) age between 20 and 65 years, (2) reducible mild or moderate hallux valgus, (3) HVA ≤ 40°, (4) IMA ≤ 20°, (5) arthritis of the 1st metatarsophalangeal joint up to grade 2 according to the Regnauld classification [52]. The exclusion criteria were: (1) stiffness of the first metatarsophalangeal joint, (2) severe arthritis of first metatarsophalangeal joint (more than Regnauld grade 2), (3) history of rheumatoid arthritis or other inflammatory diseases, (4) diabetes mellitus, (5) neurological disorders, (6) prior hallux surgery, (7) hypermobility of first metatarsophalangeal joint or first cuneo-metatarsal joint.
The average age at the time of surgery was 49 years (range 20–65 years). Two patients died of unrelated causes and 62 patients were lost to follow-up before a minimum of five years (range five to ten years), leaving 577 patients (896 feet) for final review.
Surgical technique (video)
Planning of the operation was performed by the senior author in terms of the obliquity of the bone cut, the extent of the medial-lateral or dorsal-plantar dislocation of the metatarsal head and the correction of the DMAA. Surgery involved two surgeons and it was performed under regional anaesthesia, with patients in supine position using a tourniquet. The average surgical time for hallux valgus correction was five minutes (range three to eight minutes).
By forcing the big toe into a varus position, a manual stretching of the adductor hallucis and lateral capsule was performed (Fig. 1).
Fig. 1.

Preoperative manual stretching of the adductor hallucis and the lateral capsule, forcing the big toe in varus and plantar flexed position
Surgery was performed from a medial approach through a one centimetre medial incision just proximal to the medial eminence, at the level of the neck of the first metatarsal bone, exposing the neck of the metatarsal bone with two small retractors (Fig. 2a, b).
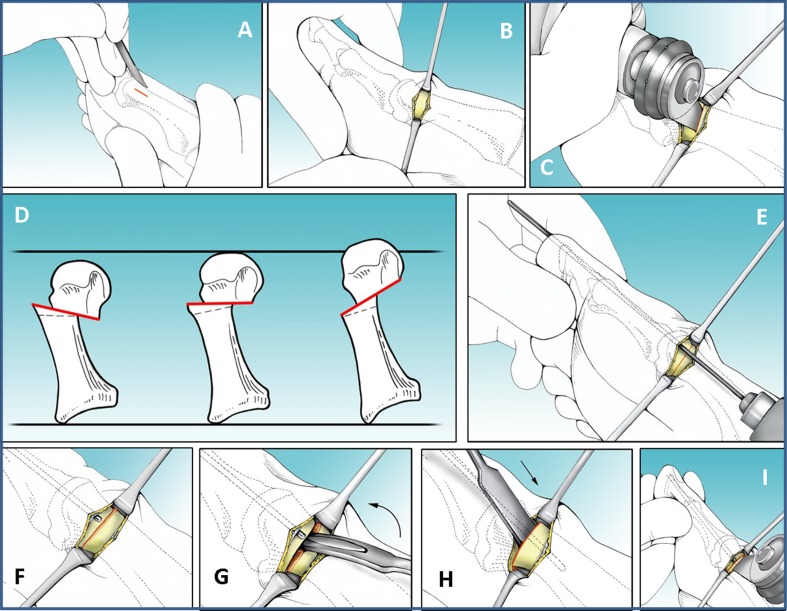
Fig. 2.
Surgical technique. One centimetre incision at the level of the neck of the 1st metatarsal bone (a). Exposure of the metatarsal neck (b). Metatarsal neck osteotomy using a pneumatic saw (c). Inclination of the osteotomy in the frontal plane, in order to maintain or modify the length of the first metatarsal bone (modified with kind permission from Springer Science+Business Media: Clin Orthop Relat Res. Giannini S, et al. The SERI Distal Metatarsal Osteotomy and Scarf Osteotomy Provide Similar Correction of Hallux Valgus. 2013 Epub Mar 14; Fig. 4b) (d). Kirschner wire insertion through the skin incision in a proximal-distal direction into the medial soft tissue adjacent to the bone (e). Kirschner wire is retaken from the tip of the toe (f) until its proximal end reaches the osteotomy line (g). Displacement of the metatarsal head to correct the pathoanatomy of the deformity (h). Kirschner wire reinsertion into the diaphyseal channel of the metatarsal bone, guided by the grooved lever, to stabilise the correction (i). Removal of a small bone wedge from the proximal stump of the osteotomy, if medially prominent (j)
The osteotomy is performed using an oscillating saw at about 15° of inclination in the sagittal plane (Fig. 2c). In the transverse plane, the inclination of the osteotomy changes with respect to the choice to elongate or shorten the metatarsal—it must be perpendicular to the foot axis (axis of the second metatarsal) if the length of the metatarsal has to be maintained. Conversely, if shortening of the metatarsal bone or decompression of the first metatarsophalangeal joint is necessary, such as in case of mild arthritis, the osteotomy is inclined in a distal to proximal direction up to 25°. Very rarely, if a lengthening of the first metatarsal bone is necessary (i.e. when the first metatarsal bone is shorter than the second, or if a mild first metatarsophalangeal joint instability is present), the osteotomy is inclined in a proximal to distal direction 15° (Fig. 2d).
A 2-mm Kirschner wire is inserted to stabilise the osteotomy. At first it is inserted in the distal direction through the incision into the soft tissues adjacent to the bone along the longitudinal axis of the great toe, coming out at its tip at three to four millimetres from the nail (Fig. 2e). The wire is withdrawn from the tip of the toe until its proximal end reaches the osteotomy line (Fig. 2f–g). Then, using a small grooved lever to access the osteotomy, the Kirschner wire is inserted in a retrograde fashion through the osteotomy site into the diaphyseal channel of the first metatarsal bone up to the base of the metatarsal (Fig. 2h–i). If the proximal stump of the osteotomy was medially prominent, a small wedge of bone was removed, using the pneumatic saw (Fig. 2j).
Before K-wire fixation, the metatarsal head can be moved in the transverse plane and rotated to correct the distal metatarsal articular angle (DMAA) (Fig. 3a). In the sagittal plane, the adjustment of the plantar/dorsal dislocation or rotation of the metatarsal head is obtained by introducing the Kirschner wire higher or lower in the soft tissues (Fig. 3b). Lesser toes correction is then performed, if required.
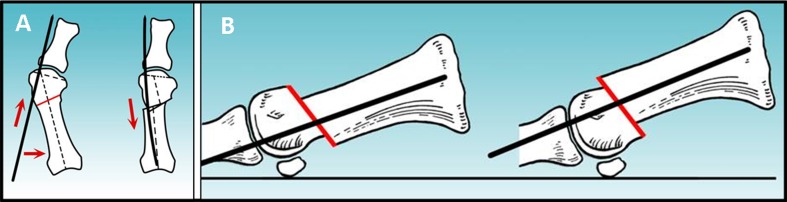
Fig. 3.
Kirschner wire is introduced into the soft tissue obliquely as many degrees as necessary to obtain adequate correction of the DMAA (a). Kirschner wire is introduced higher or lower into the soft tissues to obtain, respectively, plantar or dorsal dislocation of the metatarsal head (modified with kind permission from Springer Science+Business Media: Clin Orthop Relat Res. Giannini S, et al. The SERI Distal Metatarsal Osteotomy and Scarf Osteotomy Provide Similar Correction of Hallux Valgus. 2013 Epub Mar 14; Fig. 4a) (b)
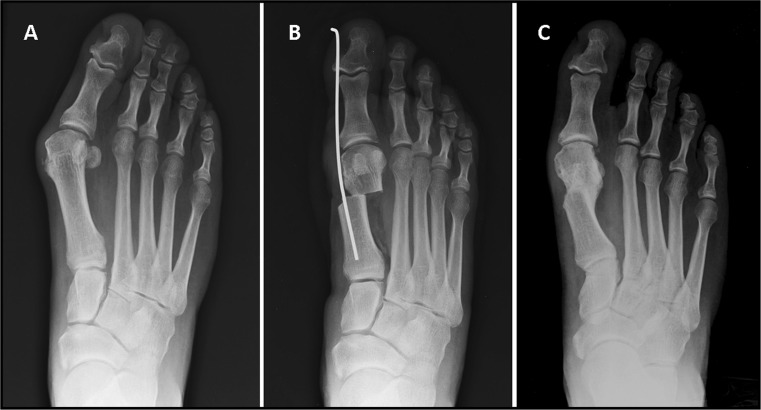
All patients are discharged the same day or one day after surgery. As in other surgical techniques of hallux valgus correction, ambulation is allowed immediately using postoperative shoes that transfer weight bearing to the hindfoot; foot elevation is advised when the patient is at rest. After 30 days, the dressing, the suture, and the Kirschner wire are removed and X-rays performed (Fig. 4). Progressive rehabilitation with passive and active exercises, cycling, and swimming are advised. Comfortable shoes are prescribed and gradual recovery of normal walking is encouraged.
Fig. 4.
A 44-year-old woman with moderate hallux valgus. Preoperative radiographic aspect of the deformity (a). Postoperative radiographic view showing the osteotomy and the correction maintained by the Kirschner wire (b). Radiographic aspect at 7-year follow-up showing the correction of the deformity with complete healing of the osteotomy and remodelling of the metatarsal bone (c)
Clinical and radiological evaluation
Preoperative planning included a complete clinical history of the patient, and a physical and radiographic examination. At preoperative assessment, all the patients complained of pain and limitation in shoe-wearing; no patients were operated upon for cosmetic concerns in absence of pain. All patients were clinically and radiographically evaluated preoperatively, one, three and six months after surgery, and then yearly until the last follow-up by four authors not involved in surgery. The average follow-up was seven years, with a range of five to ten years.
Clinical evaluation of the patients included assessment of the severity of the prominent medial eminence, the range of motion of the first metatarsophalangeal joint and the reducibility of the deformity. The range of motion of the first metatarsophalangeal joint was measured using a hinged goniometer placed on the medial aspect of the foot along the long axis of the first metatarsal bone and the long axis of the proximal phalanx as landmarks. A range of motion of 75° or more was considered normal, moderate stiffness was recorded with a range of motion between 30–74° and severe stiffness in case of range of motion lower than 30° [53]. The reducibility of the deformity was tested by pushing laterally on the head of the first metatarsal bone and simultaneously pulling the first toe medially. At the same time, all the deformities affecting the lesser toes and the stability of the other metatarsophalangeal joints were evaluated. Soft tissue conditions such as bursitis, callosities and ingrown nails were assessed. Clinical evaluation was summarised in the hallux–metatarsophalangeal–interphalangeal scale proposed by the American Orthopaedic Foot and Ankle Society (AOFAS) [53]. This system provides a score ranging from 0 to 100 points, which takes into consideration pain (maximum score, 40 points), functional capacity (maximum score, 45 points), and hallux alignment (maximum score, 15 points). Preoperative scores were compared with data collected at follow-up. Intraoperative, early and late postoperative complications were also collected for each patient.
Radiographic examination included dorso-plantar and lateral view standing radiographs of the forefoot, in order to assess the congruency of the first metatarsophalangeal joint, and also of the other metatarsophalangeal joints (Fig. 4). Radiographic analysis permitted quantification of the hallux valgus angle (HVA), the intermetatarsal angle (IMA) and the distal metatarsal articular angle (DMAA), according to the guidelines of the American Orthopaedic Foot and Ankle Society ad Hoc Committee on Angular Measurements [54] and the grade of degenerative arthritis of the first metatarsophalangeal joint according to the Regnauld classification [52]. In the dorso-plantar view we also assessed the grade of dislocation of sesamoids using the methods recommended by the AOFAS committee [55]. Three months after surgery, radiographic evaluation was performed on standing radiographs in order to properly assess HVA, IMA, DMAA and sesamoids position, assuming these as early postoperative data. Each radiographic feature and healing status of the osteotomies were assessed by four independent observers not involved with either surgery or postoperative care, and when opinion differed among the four observers, a combined assessment was performed and agreement was reached. The osteotomy was considered healed if there was bridging bone formation on at least two cortical projections and no radiolucency between metatarsal head and the metatarsal shaft was observable. During the follow-up an accurate radiographic analysis was performed in order to check possible cases of non-union, delayed union, mal-union of the osteotomy or osteonecrosis of the metatarsal head. HVA ≥ 20° was considered a recurrence of hallux valgus [56] and HVA ≤ 0° was considered an iatrogenic hallux varus [9].
Statistical analysis
All continuous data (HVA, IMA and DMAA) were expressed in terms of mean and standard deviation of mean. One way ANOVA for repeated measures was performed to analyse differences between preoperative and postoperative data at follow-up. Kendall tau test was performed to analyse the correlation among radiographic parameters and clinical outcome and complications at follow-up. For all tests p < 0.05 was considered significant. Statistical analysis was carried out using the Statistical Package for the Social Sciences (SPSS) software version 15.0 (SPSS Inc., Chicago, USA).
Results
Clinical results
Preoperatively, a normal range of motion of the first metatarsophalangeal joint or mild restriction was observed in 556 feet (62 %), moderate stiffness in 308 feet (34 %) and severe stiffness in 32 feet (4 %). At final available follow-up, worsening of stiffness was observed in 61 feet. The stiffness of the first metatarsophalangeal joint at follow-up correlated with the presence and grade of degenerative arthritis of the joint observed preoperatively (p = 0.01).
The average AOFAS score significantly improved at last follow-up to an average of 89 ± 10.3, while preoperatively it was 46.8 ± 16.7 (p < 0.001). Separate components of the AOFAS score are reported in Table 1.
Table 1.
Details (mean, range) of the clinical evaluation of the separate constituents of the AOFAS score
| AOFAS score (points) | Pre-operative | At follow-up | p value |
|---|---|---|---|
| Global (max 100) | 46.8 ± 16.7 (15–78) | 89 ± 10.3 (50–100) | <0.001 |
| Pain (max 40) | 18 (0–30) | 33 (20–40) | <0.001 |
| Function (max 45) | 29 (0–32) | 40 (27–45) | <0.001 |
| Alignment (max 15) | 3 (0–8) | 13 (8–15) | <0.001 |
Radiological results
The mean HVA value decreased from 32° ± 8.3 preoperatively to 13.3° ± 6.4 at last follow-up (p < 0.05). The mean IMA value decreased from 14.3° ± 3.3 preoperatively to 6.9° ± 3.6 at last follow-up (p < 0.05). The mean DMAA value decreased from 13.5° ± 5.3 preoperatively to 6.5° ± 4.4 at last follow-up (p < 0.05). The median sesamoids position was graded as 1 ± 1 at last follow-up, while preoperatively it was graded 2 ± 1 (Table 2).
Table 2.
Radiological results
| Measure | HVA | IMA | DMAA | Sesamoids position (number of feet for each position) | |||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ||||
| Pre-operative | 32° ± 8.3° (25–50°) | 14.3° ± 3.3° (10–18°) | 13.5° ± 5.3° (7–32°) | 0 | 204 | 388 | 304 |
| Last follow-up | 13.3° ± 6.4° (4–28°) | 6.9° ± 3.6° (2–14°) | 6.5° ± 4.4° (4–15°) | 370 | 337 | 170 | 19 |
| P value | <0.001 | <0.001 | 0.03 | <0.001 | |||
HVA hallux valgus angle, IMA intermetatarsal angle, DMAA distal metatarsal articular angle
Degenerative arthritis of the 1st metatarsophalangeal joint was absent in 526 feet (59 %), mild (grade 1) in 292 feet (32 %), and moderate (grade 2) in 78 feet (9 %) preoperatively. Worsening at last follow-up was observed in 50 feet (5.6 %). We noticed a correlation between the preoperative degree of degenerative arthritis and its worsening at follow-up (p < 0.05); moreover, a significant correlation between the presence of preoperative degenerative arthritis and poorer clinical results at last follow-up was observed (p = 0.02). Eleven patients affected by grade 3 degenerative arthritis were subjected to revision surgery; in four feet, presenting severe grade of degenerative arthritis at follow-up, arthrodesis of the metatarsophalangeal joint was performed, while cheilectomy was performed in the remaining seven patients.
Complications
Radiographic control at follow-up showed a complete healing of the osteotomy with bone remodelling at the metatarsal bone, even when bony contact was minimal (Fig. 3). No cases of non-union of the osteotomy occurred in this study population. Dorsal malunion was observed in eight feet (1 %). No radiographic evidence of avascular necrosis of the metatarsal was observed.
Recurrence was observed in 47 feet (5.3 %). In ten of these cases who complained of pain at the first metatarsophalangeal joint refractory to conservative treatment, revision surgery was performed again, correcting the deformity with the SERI technique. No statistically significant correlation between early postoperative DMAA greater than 10° and recurrence of hallux valgus was observed (p = 0.06). Higher risk of recurrence was noted in those cases presenting early postoperative grade 2 and 3 sesamoids dislocations (p < 0.05). Recurrence of the deformity significantly correlated with poorer clinical outcome at follow-up (p < 0.05). No hallux varus occurred. After dressing removal, in 21 feet (2 %) a mild skin inflammatory reaction was present around the outlet of the Kirschner wire at the tip of the toe. No patient developed a deep wound infection. Twelve patients (1.3 %) developed a deep venous thrombosis.
Discussion
The aim of the surgical treatment of hallux valgus is the correction of the deformity with a morphological and functional rebalance of the first metatarsophalangeal joint and the first ray [21–41]. Several types of distal metatarsal osteotomies have been reported with a high rate of good clinical and radiographic outcomes [15, 21, 22, 33–37, 41]. Each technique differs in terms of surgical approach, bone cut and type of fixation device. Chevron osteotomy is one of the most common procedures used to treat mild to moderate hallux valgus and several authors have reported good clinical outcomes [26, 40, 43, 46, 57]. Despite the good results obtained with this technique, considering the need to correct the increased DMAA, several authors have proposed new techniques, such as bi-planar chevron osteotomy or tri-planar distal metatarsal osteotomy with different results [22–24, 26, 33, 36]. A minimally invasive distal metatarsal osteotomy for correction of hallux valgus, whose characteristics have been summarised in the acronym SERI (simple, effective, rapid and inexpensive) [29, 50, 51, 58] has been designed, and we have prospectively followed up for at least five years the first 1,000 consecutive cases treated by this technique to evaluate (1) whether it was effective for the treatment of symptomatic hallux valgus, (2) whether its efficacy was maintained over time, and (3) to evaluate the complication rates related to this technique.
We are aware of the limitations of this study. The first limitation relates to the selection of patients, since a non-homogeneous series is reported, because of the wide age range and the different grade of the deformities and because of the association with lesser toe deformities. The second limitation relates to radiographic assessment; in fact, while the preoperative intra-observer and inter-observer reliability for HVA and IMA is excellent [55, 59–62], the assessment of DMAA remains a diagnostic challenge, with poor intra-observer and inter-observer reliability [11, 57, 61, 63]. Four of the observers were not directly involved in the treatment and we believe that clinical and radiographic assessment are less subjected to bias. Third, we speculate that the presence of associated lesser toes deformities could condition the final results, particularly affecting clinical parameters such as pain and limitation in activities of daily living and shoe wearing; however, currently we are unable to correctly quantify how these associated deformities might actually affect the final outcome. However, we believe that further studies are needed to analyse this issue in detail in order to confirm or refute our hypothesis.
In our study, the clinical evaluation according to the AOFAS score demonstrated that the SERI technique is effective in treating mild to moderate hallux valgus in terms of relief from symptoms and functional improvement. Moreover, radiographic analysis showed the effectiveness of the SERI technique in correcting the main parameters of the deformity (HVA, IMA, DMAA, sesamoids dislocation). Different authors have reported good results with distal metatarsal osteotomy according to a specific follow-up period (one to five years) [22, 36, 40, 63], but it is known that short-term and middle-term follow ups do not significantly differ from each other in terms of clinical and radiological results.
Many complications have been reported related to distal metatarsal osteotomies [15, 16, 20, 21, 26, 29, 32–35, 38, 40–43, 45–49, 56, 59, 64–70]. Osteonecrosis of the metatarsal head is one of the most severe complications after distal metatarsal osteotomies, with a reported incidence ranging from 0 % to 40 % [15, 21, 30, 32, 69, 71]. Khun et al. [72] prospectively used an intraoperative laser Doppler to demonstrate that the combination of chevron osteotomy, medial capsular release and lateral release plus adductor tenotomy resulted in a cumulative decrease in blood flow to the metatarsal head of 71 %. Moreover they noted that the greatest insult to blood flow (43 % decline) occurred during medial capsulotomy. In our series we did not observe osteonecrosis of the metatarsal head, and we believe that this result may be related to the capsular sparing with the SERI technique.
Nonunions or malunions are occasionally observed after the distal metatarsal osteotomies, mostly because the internal fixation is not stable enough [32, 33, 37, 46]. In our series we did not observe nonunions and only rarely malunions (1 %). We believe that the osteotomy’s inclination of 15° in the sagittal plane represents an important feature because it ensures an adequate stability of the osteotomy with a correct distribution of the weight-bearing (once it is allowed) in correspondence with the metatarsal head and the osteotomy, thus promoting healing of the osteotomy without compromising the correction obtained with surgery. Moreover, bending of the Kirschner wire allows an elastic fixation of the osteotomy, stabilised by a “three-point (toe–osteotomy line–metatarsal base) fixation” opposing the deformity, obtained by the forced flexion of the wire during the introduction in the diaphyseal channel. With this feature, we consider it extremely important to use a Kirschner wire that is adequately thick (two millimetres) in order to not compromise the stability of the fixation.
The prevalence of postoperative recurrence of hallux valgus ranges from 2.5 % to 38 % following distal metatarsal osteotomies [32, 33, 37, 45, 46, 56]. In our series a low rate (5.3 %) of recurrence was observed. A higher rate of recurrence was observed in feet presenting higher grades of sesamoid dislocation (grade ≥ 2). We think that the versatility of this technique, allowing correction of all the parameters of the deformity, particularly sesamoids dislocation, might represent a protective factor against the recurrence of hallux valgus.
Hallux varus as a complication of hallux valgus surgery, resulting from overcorrection, has been reported in the literature with an incidence, ranging from 0 % to 15 % [9, 29–32, 36, 73–75]. No postoperative hallux varus was observed in our series. The resection of the medial prominence, the muscle imbalance at the proximal phalangeal base and excision of fibular sesamoid, excessive medial capsulorraphy and overcorrection of IMA are assumed as important factors in the development of hallux varus [9, 46]. The SERI technique does not include any of these procedures and this may account for the lack of postoperative hallux varus deformity observed in our series.
We observed a worsening of degenerative arthritis of the first metatarsophalangeal joint in 50 feet (5.6 %) at the last follow-up, mostly in those feet presenting more severe degenerative arthritis preoperatively, and this was correlated with stiffness of the metatarsophalangeal joint and poorer clinical outcome. Therefore we believe that patients with degenerative arthritis of the first metatarsophalangeal joint might require a different surgical approach.
In conclusion we consider that the SERI technique is “simple”, because it does not include the removal of the medial eminence or lateral release, and it requires only a Kirschner wire for the fixation. Moreover, it is minimally invasive but performed under direct line of vision, without the need of intraoperative X-rays. This technique is “effective”, because using different inclinations of the bone cut in transverse planes and with a different displacement of the metatarsal head (lateral, dorsal, plantar, medial tilting or rotation), it is possible to correct the peculiar pathoanatomy of each deformity, with high rate of excellent and good results, and is durable over time. The surgical time spent is about five minutes and therefore the SERI technique is “rapid”. Finally this technique is “inexpensive” because no special instruments are needed, hardware is limited to one Kirschner wire for fixation, and surgical time is limited and associated with a low complication rate. We also advise that it is extremely important in performing the SERI technique to be aware of the specific features of the technique itself, since poor results are mostly the result of an incorrect indication or to an incorrect surgical technique.
Electronic supplementary material
(WMV 31575 kb)
References
- 1.Coughlin MJ. Hallux valgus. J Bone Joint Surg Am. 1996;78:932–966. [PubMed] [Google Scholar]
- 2.Hardy RH, Clapham JCR. Observations on hallux valgus; based on a controlled series. J Bone Joint Surg Br. 1951;33:376–391. doi: 10.1302/0301-620X.33B3.376. [DOI] [PubMed] [Google Scholar]
- 3.Hardy RH, Clapham JCR. Hallux valgus. Lancet. 1952;1:1180–1183. doi: 10.1016/S0140-6736(52)91086-6. [DOI] [PubMed] [Google Scholar]
- 4.Coughlin MJ. Juvenile hallux valgus: etiology and treatment. Foot Ankle Int. 1995;16:682–697. doi: 10.1177/107110079501601104. [DOI] [PubMed] [Google Scholar]
- 5.Piqué-Vidal C, Solé MT, Antich J. Hallux valgus inheritance: pedigree research in 350 patients with bunion deformity. J Foot Ankle Surg. 2007;46:149–154. doi: 10.1053/j.jfas.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 6.Barnicot NA, Hardy RH. The position of the hallux in West Africans. J Anat. 1955;89:355–361. [PMC free article] [PubMed] [Google Scholar]
- 7.Barouk LS, Diebold P. Hallux valgus congenital. Med Chir Pied. 1991;7:65–112. [Google Scholar]
- 8.Coughlin MJ, Jones CP. Hallux valgus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007;28:759–777. doi: 10.3113/FAI.2007.0759. [DOI] [PubMed] [Google Scholar]
- 9.Devos Bevernage B, Leemrijse T. Hallux varus: classification and treatment. Foot Ankle Clin. 2009;14:51–65. doi: 10.1016/j.fcl.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 10.Dragonetti L. Inquadramento eziopatogenetico e clinico dell’alluce abdotto-valgo. In: Malerba F, Dragonetti L, Giannini S, editors. Progressi in Medicina e Chirurgia del Piede. Bologna: L’Alluce Valgo. Aulo Gaggi Editore; 1997. pp. 155–165. [Google Scholar]
- 11.Easley ME, Trnka HJ. Current concepts review: hallux valgus part I: pathomechanics, clinical assessment, and nonoperative management. Foot Ankle Int. 2007;28:654–659. doi: 10.3113/FAI.2007.0654. [DOI] [PubMed] [Google Scholar]
- 12.Engle E, Morton DJ. Notes of foot disorders among natives of the Belgian Congo. J Bone Joint Surg Am. 1931;13:311–319. [Google Scholar]
- 13.James CS. Footprints and feet of natives of Soloman Island. Lancet. 1939;2:1390–1393. doi: 10.1016/S0140-6736(00)73938-9. [DOI] [Google Scholar]
- 14.Johnston O. Further studies of the inheritance of hand and foot anomalies. Clin Orthop Relat Res. 1956;8:146–160. [PubMed] [Google Scholar]
- 15.Hohmann G. Der Hallux Valgus und die übrigen Zehenverkrümmungen. Ergeb Chir Orthop. 1925;18:308–376. doi: 10.1007/978-3-642-91224-5_4. [DOI] [Google Scholar]
- 16.Mann RA, Coughlin MJ. Adult hallux valgus. In: Coughlin MJ, Mann RA, editors. Surgery of the foot and ankle. St. Louis: Mosby; 1999. pp. 150–269. [Google Scholar]
- 17.Pontius J, Kieran D, Mahan T, Carter S. Characteristics of adolescent hallux abductus-valgus. A retrospective review. J Am Podiatr Med Assoc. 1994;84:208–218. doi: 10.7547/87507315-84-5-208. [DOI] [PubMed] [Google Scholar]
- 18.Root ML, Orien WP, Weed JH. Deformità dell’avampiede causate dall’anomala pronazione della sottoastragalica. In: Root ML, Orien WP, Weed JH, editors. La fuzionalità del piede normale e patologico. Padova: Piccin; 2001. pp. 333–435. [Google Scholar]
- 19.Sim-Fook L, Hodgson AR. A comparison of foot forms among the non-shoe and shoe-wearing Chinese population. J Bone Joint Surg Am. 1958;40:1058–1062. [PubMed] [Google Scholar]
- 20.Veri JP, Pirani SP, Claridge R. Crescentic proximal metatarsal osteotomy for moderate to severe hallux valgus: a mean 12.2 year follow-up study. Foot Ankle Int. 2001;22:817–822. doi: 10.1177/107110070102201007. [DOI] [PubMed] [Google Scholar]
- 21.Austin DW, Leventen EO. A new osteotomy for hallux valgus: a horizontally directed “V” displacement osteotomy of the metatarsal head for hallux valgus and primus varus. Clin Orthop Relat Res. 1981;157:25–30. [PubMed] [Google Scholar]
- 22.Bosch P, Markowski H, Rannicher V. Technik und erste Ergebnisse der subkutanen distalen Metatarsale-I-Osteotomie. Orthopaedische Praxis. 1990;26:51–56. [Google Scholar]
- 23.Chou LB, Mann RA, Casillas MM. Biplanar chevron osteotomy. Foot Ankle Int. 1998;19:579–584. doi: 10.1177/107110079801900902. [DOI] [PubMed] [Google Scholar]
- 24.Chang JT. Distal metaphyseal osteotomies in hallux abducto valgus surgery. In: Banks AS, Downey MS, Martin DE, Miller SJ, editors. McGlamry’s comprehensive textbook of foot and ankle surgery. Philadelphia: Lippincott, Williams & Wilkins; 2001. pp. 505–527. [Google Scholar]
- 25.Coetzee JC, Wickum D. The Lapidus procedure. A prospective cohort outcome study. Foot Ankle Int. 2004;25:526–531. doi: 10.1177/107110070402500803. [DOI] [PubMed] [Google Scholar]
- 26.Corte-Real NM, Moreira RM. Modified biplanar chevron osteotomy. Foot Ankle Int. 2009;30:1149–1153. doi: 10.3113/FAI.2009.1149. [DOI] [PubMed] [Google Scholar]
- 27.Chuckpaiwong B. Comparing proximal and distal metatarsal osteotomy for moderate to severe hallux valgus. Int Orthop. 2012;36:2275–2278. doi: 10.1007/s00264-012-1656-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fuhrmann RA, Zollinger-Kies H, Kundert HP. Mid-term results of Scarf osteotomy in hallux valgus. Int Orthop. 2010;34:981–989. doi: 10.1007/s00264-010-0958-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Giannini S, Ceccarelli F, Bevoni R, Vannini F. Hallux valgus surgery: the minimally invasive bunion correction (SERI) Tech Foot Ankle Surg. 2003;2:11–20. doi: 10.1097/00132587-200303000-00003. [DOI] [Google Scholar]
- 30.Groulier P, Curvale G. Postoperative iatrogenic hallux varus. Surgical treatment. Rev Chir Orthop Reparatrice Appar Mot. 1992;78:449–455. [PubMed] [Google Scholar]
- 31.Jawish R, Assoum H, Saliba E. Opening wedge osteotomy of the first cuneiform for the treatment of hallux valgus. Int Orthop. 2010;34:361–368. doi: 10.1007/s00264-009-0825-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kadakia AR, Smerek JP, Myerson MS. Radiographic results after percutaneous distal metatarsal osteotomy for correction of hallux valgus deformity. Foot Ankle Int. 2007;28:355–360. doi: 10.3113/FAI.2007.0355. [DOI] [PubMed] [Google Scholar]
- 33.Lamprecht E. Die retrokapitale Metatarsale-I-Osteotomie nach Kramer zur Behandlung des Hallux valgus. In: Meyer RP, Kappeler U, editors. Fußchirurgie in der Praxis. Germany: Springer-Verlag Berlin Heidelberg; 1996. pp. 145–157. [Google Scholar]
- 34.Lucijanic I, Bicanic G, Sonicki Z, Mirkovic M, Pecina M. Treatment of hallux valgus with three-dimensional modification of Mitchell's osteotomy: technique and results. J Am Podiatr Med Assoc. 2009;99:162–172. doi: 10.7547/0980162. [DOI] [PubMed] [Google Scholar]
- 35.Magerl F. Stabile Osteotomien zur Behandlung des Hallux valgus und Metatarsale I varum. Orthopade. 1982;11:170–180. [PubMed] [Google Scholar]
- 36.Magnan B, Pezzè L, Rossi N, Bartolozzi P. Percutaneous distal metatarsal osteotomy for correction of hallux valgus. J Bone Joint Surg Am. 2005;86:1191–1199. doi: 10.2106/JBJS.D.02280. [DOI] [PubMed] [Google Scholar]
- 37.Mitchell CL, Fleming JL, Allen R, Glenney C, Sanford G. Osteotomy-bunionectomy for hallux valgus. J Bone Joint Surg Am. 1958;40:41–58. [PubMed] [Google Scholar]
- 38.Nery CAB, Barroco RUB, Ressio C. Biplanar chevron osteotomy. Foot Ankle Int. 2002;23:792–798. doi: 10.1177/107110070202300903. [DOI] [PubMed] [Google Scholar]
- 39.Sanna P, Ruiu GA. Percutaneous distal osteotomy of the first metatarsal (PDO) for the surgical treatment of hallux valgus. Chir Organi Mov. 2005;90:365–369. [PubMed] [Google Scholar]
- 40.Trnka HJ, Zembsch A, Wiesauer H, Hungerford M, Salzer M, Ritschl P. Modified Austin procedure for correction of hallux valgus. Foot Ankle Int. 1997;18:119–127. doi: 10.1177/107110079701800302. [DOI] [PubMed] [Google Scholar]
- 41.Wilson JN. Oblique displacement osteotomy for hallux valgus. J Bone Joint Surg Br. 1963;45:552–556. [PubMed] [Google Scholar]
- 42.Pinney SJ, Song KR, Chou LB. Surgical treatment of mild hallux valgus deformity: the state of practice among academic foot and ankle surgeons. Foot Ankle Int. 2006;27:970–973. doi: 10.1177/107110070602701118. [DOI] [PubMed] [Google Scholar]
- 43.Pinney SJ, Song KR, Chou LB. Surgical treatment of severe hallux valgus: the state of practice among academic foot and ankle surgeons. Foot Ankle Int. 2006;27:1024–1029. doi: 10.1177/107110070602701205. [DOI] [PubMed] [Google Scholar]
- 44.Maffulli N, Longo UG, Oliva F, Denaro V, Coppola C. Bosch osteotomy and scarf osteotomy for hallux valgus correction. Orthop Clin N Am. 2009;40:515–524. doi: 10.1016/j.ocl.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 45.Myerson MS. Hallux valgus. In: Myerson MS, editor. Foot and ankle disorders. Philadelphia: WB Saunders; 2000. pp. 213–285. [Google Scholar]
- 46.Wulker N. Hallux valgus: distal first metatarsal osteotomy. In: Wulker N, Stephens MM, Cracchiolo A, editors. An atlas of foot and ankle surgery. Abingdon: Taylor & Francis; 2005. pp. 9–17. [Google Scholar]
- 47.Nikolaou VS, Korres D, Xypnitos F, Lazarettos J, Lallos S, Sapkas G, Efstathopoulos N. Fixation of Mitchell’s osteotomy with bioabsorbable pins for treatment of hallux valgus deformity. Int Orthop. 2009;33:701–706. doi: 10.1007/s00264-008-0664-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Park CH, Ahn JY, Kim YM, Lee WC (2013) Plate fixation for proximal chevron osteotomy has greater risk for hallux valgus recurrence than Kirschner wire fixation. Int Orthop 37(6):1085–1092 [DOI] [PMC free article] [PubMed]
- 49.Grace DL. Metatarsal osteotomy: which operation? J Foot Surg. 1987;82:501–506. [Google Scholar]
- 50.Giannini S, Faldini C, Vannini F, Digennaro V, Bevoni R, Luciani D. The minimally invasive osteotomy “S.E.R.I”. (simple, effective, rapid, inexpensive) for correction of bunionette deformity. Foot Ankle Int. 2008;29:282–286. doi: 10.3113/FAI.2008.0282. [DOI] [PubMed] [Google Scholar]
- 51.Giannini S, Faldini C, Vannini F, Cadossi M, Luciani D. The minimally invasive hallux valgus correction (SERI) In: Wiesel SW, editor. Operative technique in orthopaedic surgery. Philadelphia: Lippincott, Williams & Wilkins; 2001. pp. 3505–3511. [Google Scholar]
- 52.Regnauld B. Hallux rigidus. In: Elson R, editor. The foot. Berlin: Springer; 1986. pp. 335–350. [Google Scholar]
- 53.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating system for the ankle-hindfoot, midfoot, hallux and lesser toes. Foot Ankle Int. 1994;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 54.Coughlin MJ, Saltzman CL, Nunley JA. Angular measurements in the evaluation of hallux valgus deformities: a report of the Ad Hoc Committee of the American Orthopaedic Foot and Ankle Society on angular measurements. Foot Ankle Int. 2002;23:68–74. doi: 10.1177/107110070202300114. [DOI] [PubMed] [Google Scholar]
- 55.Smith RW, Reynolds JC, Stewart MJ. Hallux valgus assessment: report of research committee of American Orthopaedic Foot and Ankle Society. Foot Ankle. 1984;5:92–103. doi: 10.1177/107110078400500208. [DOI] [PubMed] [Google Scholar]
- 56.Okuda R, Kinoshita M, Yasuda T, Jotoku T, Kitano N, Shima H. Postoperative incomplete reduction of the sesamoids as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am. 2009;91:1637–1645. doi: 10.2106/JBJS.H.00796. [DOI] [PubMed] [Google Scholar]
- 57.Coughlin MJ. Hallux valgus in men: effect of the distal metatarsal articular angle on hallux valgus correction. Foot Ankle Int. 1997;18:463–470. doi: 10.1177/107110079701800802. [DOI] [PubMed] [Google Scholar]
- 58.Giannini S, Cavallo M, Faldini C, Luciani D, Vannini F (2013) The SERI distal metatarsal osteotomy and scarf osteotomy provide similar correction of hallux valgus. Clin Orthop Relat Res 471(7):2305–2311 [DOI] [PMC free article] [PubMed]
- 59.Easley ME, Trnka HJ. Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int. 2007;28:748–758. doi: 10.3113/FAI.2007.0748. [DOI] [PubMed] [Google Scholar]
- 60.Coughlin MJ, Freund E, Roger A. Mann award. The reliability of angular measurements in hallux valgus deformities. Foot Ankle Int. 2001;22:369–379. doi: 10.1177/107110070102200503. [DOI] [PubMed] [Google Scholar]
- 61.Saltzman CL, Brandser EA, Berbaum KS, DeGnore L, Holmes JR, Katcherian DA, Teasdall RD, Alexander IJ. Reliability of standard foot radiographic measurements. Foot Ankle Int. 1994;15:661–665. doi: 10.1177/107110079401501206. [DOI] [PubMed] [Google Scholar]
- 62.Schneider W, Csepan R, Knahr K. Reproducibility of the radiographic metatarsophalangeal angle in hallux surgery. J Bone Joint Surg Am. 2003;85:494–499. doi: 10.2106/00004623-200303000-00015. [DOI] [PubMed] [Google Scholar]
- 63.Chi TD, Davitt J, Younger A, Holt S, Sangeorzan BJ. Intra- and inter-observer reliability of the distal metatarsal articular angle in adult hallux valgus. Foot Ankle Int. 2002;23:722–726. doi: 10.1177/107110070202300808. [DOI] [PubMed] [Google Scholar]
- 64.Oliva F, Longo UG, Maffulli N. Minimally invasive hallux valgus correction. Orthop Clin N Am. 2009;40:525–530. doi: 10.1016/j.ocl.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 65.Becker A. First metatarsal malunion. Foot Ankle Clin N Am. 2009;14:77–90. doi: 10.1016/j.fcl.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 66.Belczyk R, Stapleton JJ, Grossman JP, Zgonis T. Complications and revisional hallux valgus surgery. Clin Podiatr Med Surg. 2009;26:475–484. doi: 10.1016/j.cpm.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 67.Nyska M. Principles of first metatarsal osteotomies. Foot Ankle Clin. 2001;6:399–408. doi: 10.1016/S1083-7515(03)00104-9. [DOI] [PubMed] [Google Scholar]
- 68.Okuda R, Kinoshita M, Morikawa J, Jotoku T, Abe M. Surgical treatment for hallux valgus with painful plantar callosities. Foot Ankle Int. 2001;22:203–208. doi: 10.1177/107110070102200306. [DOI] [PubMed] [Google Scholar]
- 69.Vora AM, Myerson MS. First metatarsal osteotomy nonunion and malunion. Foot Ankle Clin. 2005;10:35–54. doi: 10.1016/j.fcl.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 70.Weil LS. Scarf osteotomy for correction of hallux valgus. Historical perspective, surgical technique, and results. Foot Ankle Clin. 2000;5:559–580. [PubMed] [Google Scholar]
- 71.Resch S, Stenstrom A, Gustafson T. Circulatory disturbance of the first metatarsal head after chevron osteotomy as shown by bone scintigraphy. Foot Ankle. 1992;13:137–142. doi: 10.1177/107110079201300305. [DOI] [PubMed] [Google Scholar]
- 72.Kuhn MA, Lippert FG, 3rd, Phipps MJ, Williams C. Blood flow to the metatarsal head after chevron bunionectomy. Foot Ankle Int. 2005;26:526–529. doi: 10.1177/107110070502600705. [DOI] [PubMed] [Google Scholar]
- 73.Goldman FD, Siegel J. Extensor hallucis longus tendon transfer for correction of hallux varus. J Foot Ankle Surg. 1993;32:126–131. [PubMed] [Google Scholar]
- 74.Dhillon MS, Bali K, Prabhakar S. Controversies in calcaneus fracture management: a systematic review of the literature. Musculoskelet Surg. 2011;95:171–181. doi: 10.1007/s12306-011-0114-y. [DOI] [PubMed] [Google Scholar]
- 75.Hawkins FB. Acquired hallux valgus: cause, prevention and correction. Clin Orthop Relat Res. 1971;76:169–176. doi: 10.1097/00003086-197105000-00024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(WMV 31575 kb)