Abstract
Patients with varus or valgus hindfoot deformities usually present with asymmetric ankle osteoarthritis. In-vitro biomechanical studies have shown that varus or valgus hindfoot deformity may lead to altered load distribution in the tibiotalar joint which may result in medial (varus) or lateral (valgus) tibiotalar joint degeneration in the short or medium term. The treatment of asymmetric ankle osteoarthritis remains challenging, because more than half of the tibiotalar joint surface is usually preserved. Therefore, joint-sacrificing procedures like total ankle replacement or ankle arthrodesis may not be the most appropriate treatment options. The short- and midterm results following realignment surgery, are very promising with substantial pain relief and functional improvement observed post-operatively. In this review article we describe the indications, surgical techniques, and results from of realignment surgery of the ankle joint in the current literature.
Keywords: Ankle osteoarthritis, Asymetric ankle osteoarthritis, Tibiotalar joint, Total ankle replacement, Ankle arthrodesis, Ankle realignment surgery, Ankle joit surgery, Supramalleollar osteotomies, Ankle osteotomy
Introduction
Osteoarthritis (OA), the degeneration of articular cartilage and is one of the most common human diseases. Approximately 1 % of the world’s adult population is affected by symptomatic ankle OA [1], resulting in a substantial economic burden for patients and health care systems [2]. Ankle OA has a lower incidence than OA of the knee or hip joints [3]; however, this disease should not be underestimated as the patients with end-stage ankle OA have mental and physical disability comparable to those of patients with end-stage hip OA [1]. In patients with post-traumatic ankle OA the degenerative changes often develop asymmetrically with a concomitant varus or valgus deformity of the hindfoot [4, 5]. In patients with asymmetric ankle OA only a part of the tibiotalar joint surface is involved in the osteoarthritic process: the medial ankle joint compartment in varus arthritic ankles and the lateral ankle joint compartment in valgus arthritic ankles [6, 7]. Numerous surgical procedures have been described to treat the different stages of ankle OA. These procedures can be divided into two categories: joint-preserving and joint-sacrificing procedures. Joint-preserving procedures include ankle arthroscopy/arthrotomy with joint debridement [8], distraction arthroplasty [9], different osteochondral resurfacing procedures [10] and corrective osteotomies [11]. Joint-sacrificing procedures such as ankle arthrodesis [12] and total ankle replacement [13, 14] may provide good functional results and post-operative pain relief in the short term, but may have potential complications and long-term problems [15–17]. Furthermore, patients with post-traumatic ankle OA are usually younger than patients with end-stage degenerative OA of the hip or knee [18]. Therefore, in younger and more active patients joint-preserving procedures may be a more optimal treatment option.
Aetiology of ankle osteoarthritis
Approximately 80 % of all patients with end-stage ankle OA have a post-traumatic aetiology [5, 7, 19, 20]: The most common reason for developing post-traumatic ankle OA is a fracture of the lower extremity. Horisberger et al. [5] analysed 257 consecutive patients with post-traumatic end-stage OA. Fracture types causing degenerative changes of the ankle joint were of the malleolar, tibial pilon, tibial shaft, talus and combined varieties with incidencies of 53.2, 29.1, 5.7, 2.8 and 9.2 %, respectively [5]. Stufkens et al. [21] performed a long-term follow-up study of a prospective cohort of 288 ankle fractures that were treated operatively between 1993 and 1997 [22]. In the initial study, arthroscopy was performed in all cases to assess the extent and location of intra-articular cartilage damage [22]. In a follow-up study [21] a total of 109 patients were available for clinical and radiographic assessment. Following factors were identified as independent predictors of the development of post-traumatic ankle OA: deep cartilage lesion on the anterior and lateral aspect of the talus and on the medial malleolus with odds ratios of 12.3, 5.4 and 5.2, respectively [21]. Sequelae of lower leg fractures may result in post-traumatic ankle OA, as well as repetitive ankle ligament lesions [23]. Valderrabano et al. [23] performed an aetiological, clinical and radiographic review of 33 ankles with ligamentous post-traumatic ankle OA. The majority of the patients (85 %) had injuries of the lateral ankle ligaments and 15 % had injury of the medial and medial-lateral ligaments. The mean latency time between injury and end-stage ankle OA was 34.3 years. In this study, lateral ankle sprains in sports were the main cause of ligamentous post-traumatic ankle OA with significant concomitant varus malalignment of the hindfoot [23]. Lübbeke et al. [24] conducted a retrospective cohort study including 372 patients treated with open reduction and internal fixation for malleolar fractures. In more than 30 % of patients advanced degenerative changes were observed in the ankle joint, especially following Weber C fractures and associated medial malleolar fractures. The latency time between injury and ankle OA was between 12 and 22 years. Additional risk factors for OA were substantial fracture dislocation, high body mass index, age greather than 30 years and length of time since surgery [24].
Indications and contraindications
The main indication for supramalleolar osteotomies is asymmetric ankle OA with concomitant valgus or varus deformities and a partially (at least 50 %) preserved tibiotalar joint surface [25, 26]. Another important indication for realignment osteotomies are isolated osteochondral lesion of the medial or lateral aspect of the tibiotalar joint [27]. Realignment surgery may also be performed before ankle joint-sacrificing surgeries like ankle arthrodesis and total ankle replacement. It has been shown, that biomechanical properties and clinical outcomes of total ankle replacement depend on alignment and position of prosthesis components [28–30].
The absolute contraindications for realignment surgery are end-stage degenerative changes of the complete tibiotalar joint, unmanageable hindfoot instability, acute or chronic infections, severe vascular or neurological deficiency and neuropathic disorders (e.g. Charcot arthropathy). Another absolute contraindication is the patient’s non-compliance regarding the post-operative rehabilitation (including avoiding weight-bearing).
A relative contraindication is advanced age: there is no definite age below which corrective osteotomies should be avoided; however, in patients older than 70 years and in poor general condition we do not recommend this surgical treatment. Another relative contraindication is substantially impaired bone quality of the distal tibia and/or talus (e.g. patients on long-term steroid medication or with large subchondral cysts, severe osteoporosis or rheumatic disease). Tobacco use is also a relative contraindication for supramalleolar osteotomy due to an expected higher rate of osseous non-union [31].
Radiographic assessment and pre-operative planning
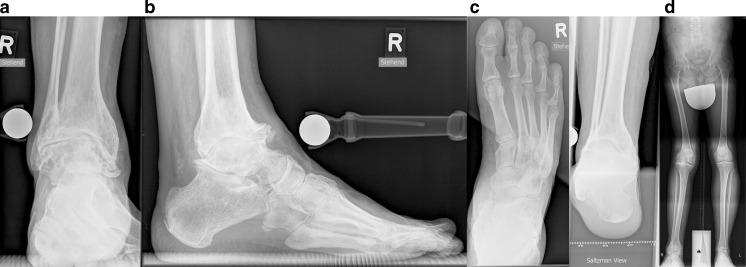
For radiographic assessment we routinely use conventional standardised weight-bearing radiographs in four planes including a lateral and dorsoplantar view of the foot and anteroposterior view of the ankle, and the Saltzman view (Fig. 1a–d) [32]. In addition, whole leg radiographs should be performed to assess osseous deformities of the lower extremity (Fig. 1e), especially around the knee joint.
Fig. 1.
Radiographic assessment of foot and ankle. Radiographic evaluation of affected ankles with weight-bearing radiographs, including anteroposterior view of the ankle (a), lateral (b) and dorsoplantar (c) views of the ankle, and Saltzman view of the hindfoot (d). Whole leg radiograph is used to assess concomitant deformities of the lower extremity (d)
In patients with degenerative changes of the tibiotalar and/or adjacent joints we suggest that single photon emission computed tomography/computed tomography (SPECT/CT) be performed to assess the exact localisation and biological activity of degenerative ankle changes and coexisting degenerative changes in the adjacent joints [33, 34]. SPECT/CT has been shown to have a high sensitivity for assessment of osseous structures in patients with chronic foot pain [35].
For preoperative planning and the calculation of the degree of surgical correction we use weight-bearing anteroposterior and lateral radiographs of the ankle. One of the most important radiographic parameters for quantification of the supramalleolar varus or valgus deformity is the medial distal tibial angle. In the previously published radiographic [36] and cadaver [37] studies it has been measured as 92.4 ± 3.1° (range 84–100°) and 93.3 ± 3.2° (range 88–100°), respectively. Stufkens et al. [38] demonstrated that this angle differs between whole lower leg radiographs and mortise views of the ankle; therefore, it should be measured using standardised radiographs. Furthermore, Barg et al. [39] found a substantial disagreement in primary supramalleolar alignment (as measured using the medial distal tibial angle) between the mortise and Saltzman views. Another radiographic parameter which should be considered for the pre-operative planning is the talar tilt. The talar tilt is defined as the difference between the medial distal tibial angle and the tibiotalar angle (normal value 91.5 ± 1.2°) [40]. In neutrally aligned ankles the talar tilt should be less than 4° [6, 41].
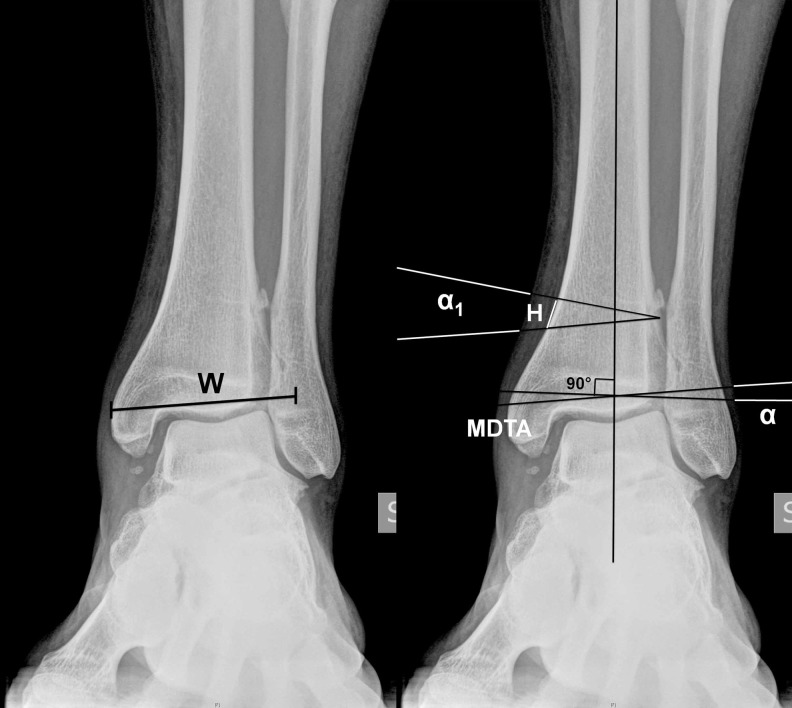
To determine the height of the wedge (H) to be removed, the width of the distal tibia (W) was measured using weight-bearing anteroposterior radiograph (Fig. 2a). The following calculation was used to determine the height of the wedge: H = tan α1 × W, where α1 is the amount of deformity with the desired overcorrection (Fig. 2b) [42, 43]. The proximal plane of the osteotomy was planned to be perpendicular to the medial tibial cortex. The corresponding distal plane was planned on the basis of the calculated height of the osteotomy wedge as described above.
Fig. 2.
Pre-operative planning. Pre-operative weight-bearing anteroposterior radiograph is used for the planning of a supramalleolar medial closing wedge osteotomy. aW width of the distal part of the tibia (in this case 62 mm). bMDTA medial distal tibial angle (in this case 97.5°), α valgus deformity (in this case 97.5°), α1 amount of valgus deformity with desired overcorrection (in this case 7.5 + 2° = 9.5°), H height of the wedge to be removed (in this case tan 9.5° × 62 mm = 10 mm)
Surgical techniques
In patients with supramalleolar valgus or varus deformities, the surgeon can choose from three surgical options: medial closing wedge osteotomy (anti-valgus osteotomy) and medial opening wedge osteotomy or lateral closing wedge osteotomy (anti-varus osteotomy).
Both types of corrective osteotomy (anti-valgus and anti-varus) can be performed using general or regional anaesthesia. The patient is placed in a supine position with the heel on the edge of the table. A radiolucent operating table is required for use of intraoperative fluoroscopy. The ipsilateral back is lifted until a strictly upward position of the foot is obtained. A pad is placed under the lower leg for elevation and fluoroscopy during surgery. A tourniquet (usually between 280 and 350 mmHg) is applied on the ipsilateral thigh. In most patients, prior to the osseous reconstructive surgery, anterior ankle arthroscopy [16] is performed to assess cartilage degeneration using the Outerbridge classification [44]. If necessary, loose bodies are removed and anterior ankle impingement is debrided. In patients with a cartilage Outerbridge grade IV lesion cartilage debridement and microfracturing should be performed.
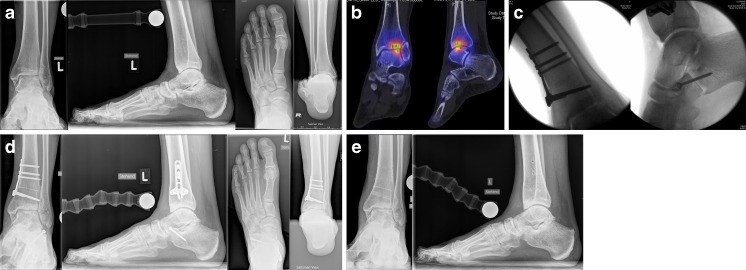
Medial closing wedge osteotomy (Fig. 3)
Fig. 3.
Medial closing wedge osteotomy and corrective Z-shaped osteotomy of the fibula. a Pre-operative weight-bearing radiographs show post-traumatic valgus tilting of the talus within the mortise and malunion of the fibula with substantial shortening and external rotation. Saltzman view shows the valgus hindfoot alignment. b First, corrective Z-shaped osteotomy of the fibula was performed to achieve elongation of the fibula and derotation as well as an aligned ankle mortise. Then medial closing wedge osteotomy was performed to address the valgus hindfoot deformity. c Post-operative weight-bearing radiographs show completed osseous healing at the site of osteotomies at the 1-year follow-up. Saltzman view shows normal hindfoot alignment. d After hardware removal patient is pain-free with no restrictions of sports activities
A medial longitudinal incision is made over the distal tibia and medial malleolus. After periosteal incision soft tissues are retracted en bloc using two Hohmann hooks. This may help to avoid injury of the neurovascular and tendon structures of the posterior and anterior compartments. The plane of the osteotomy is determined under fluoroscopic image intensification, and two distal Kirschner wires are placed parallel to the tibiotalar joint space in order to prevent changes in sagittal distal tibia slope. Two proximal Kirschner wires are placed according to the pre-operatively planned angle. Using a wide saw blade (in order to avoid an uneven osteotomy surface which may compromise post-operative healing) the osteotomy is performed with water irrigation to reduce thermal damage during the cut. The osteotomy may be refined using a chisel or osteotome. The lateral cortex is typically preserved to enhance the intrinsic stability of the osteotomy, and so the intact fibula does not hinder the desired tibial correction. The closed osteotomy is stabilised using a T-shaped 3.5-mm LCP plate with angular stabilizing screws and eccentric compressive screws immediately proximal to the osteotomy. The most proximal plate holes also require angular stabilizing screws. To increase the pressure at the site of the osteotomy, a compression device may also be used. The periosteum is closed over the osteotomy with 2-0 absorbable sutures.
Corrective Z-shaped osteotomy of the fibula (Fig. 3)
Distal fibular malunion may occur in up to one third of all cases after fibular reconstruction [45]. Malunions of the fibula should not be accepted because even small displacements of the fibula (e.g. 2 mm shortening, 2 mm lateral shift or 5° of external rotation) may dramatically change the biomechanics of the tibiotalar joint [46]. The length and rotation of the fibula is assessed intraoperatively using fluoroscopy. A longitudinal incision is made over the distal fibula. Z-shaped osteotomy is performed using an oscillating saw and osteotomy fragments are mobilised until the appropriate length of the fibula is achieved. A bone wedge is removed additionally in patients with rotational deformity. Appropriate fibular position is defined by the following criteria [47]: (1) appropriate closure of the medial clear space with restoration of the medial gutter, (2) anatomical position of the talus within the mortise and (3) restoration of anatomical landmarks as described by Weber and Simpson [48]. Final fixation of the fibular osteotomy is performed using one or two lag screws and 3.5 LCP angular stable plate.
Lateral lengthening calcaneal osteotomy (Fig. 4)
Fig. 4.
Medial closing wedge osteotomy and lateral lengthening calcaneal osteotomy. a Pre-operative weight-bearing radiographs show incipient degenerative changes of the lateral tibiotalar joint with slight valgus tilting of the talus within the mortise. Saltzman view shows the valgus hindfoot alignment. b SPECT/CT shows biologically active subchondral cysts in the lateral tibiotalar joint. c Supramalleolar medial closing wedge osteotomy and lateral lengthening calcaneal osteotomy were performed to correct the valgus malalignment of the hindfoot and pes planovalgus et abductus deformity. d Post-operative weight-bearing radiographs show completed osseous healing at the site of osteotomies at the 1-year follow-up. Saltzman view shows normal hindfoot alignment. e After hardware removal patient is pain-free with no restrictions of sports activities
After performing supramalleolar corrective osteotomy the position of the calcaneus should be proven clinically and radiographically using fluoroscopy. In patients with remaining valgus position of the calcaneus and abduction deformity of the mid- and forefoot, the deformity should be corrected at the inframalleolar level by lateral lengthening calcaneal osteotomy [49, 50]. The sinus tarsi and the posterior facet of the subtalar joint are exposed using an oblique incision over the lateral aspect of the hindfoot. The lateral calcaneal wall is osteotomised using an oscillating saw or a chisel. The medial calcaneal cortex should remain preserved so as not to compromise the intrinsic stability of the osteotomy. The osteotomy is widened until a physiological position of the hindfoot (correction of valgus) and midfoot (correction of abductus and restoration of the medial arch) is achieved. The osteotomy gap can be filled with allograft or autograft [51, 52]. The osteotomy is finally fixed using a 3.5-mm cortical AO screw or using a small plate.
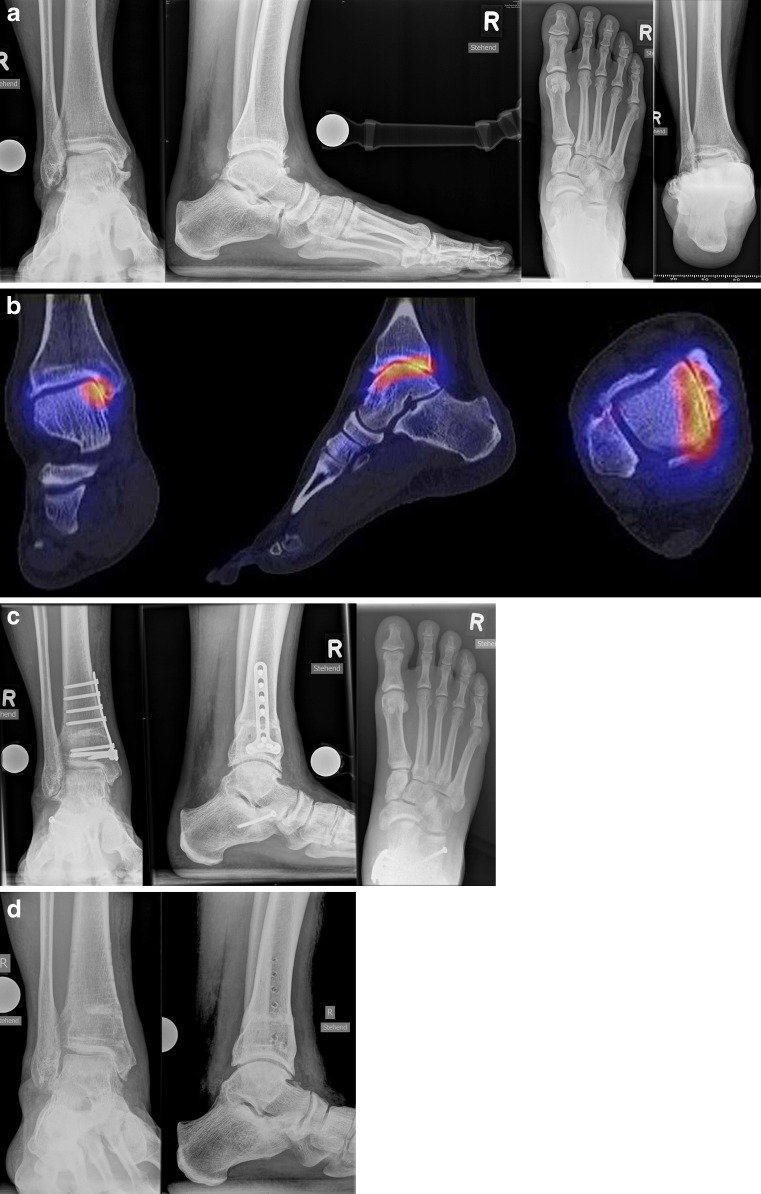
Medial opening wedge osteotomy (Fig. 5)
Fig. 5.
Medial opening wedge osteotomy. a Pre-operative weight-bearing radiographs show varus tilting of the talus within the mortise. However, the Saltzman view shows the valgus heel position, as the patient has peritalar instability with Z-shaped hindfoot deformity. b SPECT/CT shows biologically active degenerative changes of the medial tibiotalar joint. c Supramalleolar medial opening wedge osteotomy was performed to address the varus tilt of the talus and lateral lengthening calcaneal osteotomy to address the inframalleolar valgus deformity of the hindfoot. Post-operative weight-bearing radiographs show completed osseous healing at the site of osteotomies at the 1-year follow-up. d After hardware removal patient is pain-free with no restrictions of sports activities
The medial opening wedge osteotomy is indicated in cases with a varus deformity less than 10° and performed in a manner similar to the medial closing wedge osteotomy. However, only one Kirschner wire is necessary for orientation and saw blade guidance. The gap can be filled with allograft or autograft harvested from the ipsilateral iliac crest bone. The fixation of the osteotomy is performed as described above (medial closing wedge osteotomy). If during the osteotomy opening the lateral cortex could not be preserved an additional fixation of compromised lateral cortex using e.g. a one third tubular plate should be performed through a small additional lateral incision.
Lateral closing wedge osteotomy (Fig. 6)
Fig. 6.
Lateral closing wedge osteotomy. a Pre-operative weight-bearing radiographs show varus tilting of the talus within the mortise and degenerative changes of the medial tibiotalar joint and the subtalar joint. Saltzman view shows the varus hindfoot alignment. b Supramalleolar lateral closing wedge osteotomy, corrective osteotomy of the fibula and valgisation subtalar arthrodesis were performed. Post-operative weight-bearing radiographs show completed osseous healing at the site of osteotomies and subtalar arthrodesis. Saltzman view shows normal hindfoot alignment
In patients with a pre-operative varus deformity of more than 10° an extensive medial opening wedge osteotomy may not be possible because the fibula may restrict the degree of correction [6, 53]. Therefore, a lateral approach including an osteotomy of the fibula is required. An incision is made over the anterior margin of the distal fibula. A Z-shaped osteotomy of the fibula (Valderrabano osteotomy [54]) is performed using an oscillating saw where shortening of the fibula is achieved by removal of a bone block. The simple transverse fibular osteotomy has substantially less intrinsic stability which may result in fibular malposition [53, 55]. After the fibula is cut, Kirschner wires are drilled into the tibia according to the angle measured during pre-operative planning. After a fluoroscopic check of the Kirschner wire position the periosteum is incised and mobilised using a raspatory. The tibial lateral closing wedge osteotomy is performed under protection with Hohmann hooks through the same incision as the fibular shortening osteotomy and fixed using a 3.5 LCP angular stable plate.
Post-operative management
The dressing and splint are removed and changed on the second post-operative day. Early physiotherapy with lymphatic drainage and active motion can be started. A pneumatic foot cuff (with intermittent pressure up to 140 mmHg) may be used to reduce post-operative swelling. All patients receive thromboprophylaxis with subcutaneous low molecular weight heparin or oral medication with rivaroxaban starting 12 hours pre-operatively and continuing daily for six weeks post-operatively. When the wound conditions are appropriate, meaning a dry wound without any secretion, the foot/ankle is placed in a stabilising walker for six to eight weeks during which only partial weight-bearing up to 15 kg is allowed. The first follow-up is scheduled six to eight weeks post-operatively and includes clinical and radiographic assessment. In patients with appropriate osseous healing at the site of the osteotomy the walker can be removed and full weight-bearing is increased in a stepwise manner. Ambulatory physiotherapy is continued and included extending active and passive ankle motion, stretching and strengthening of the lower leg musculature, and proprioceptive exercises. In patients with persistent swelling, we recommend the use of compression stockings. Sports and recreational activities can be resumed three to four months post-operatively [56].
Complications
Complications are generally rare with supramalleolar osteotomies [57, 58]; however, there are limited data regarding the intraoperative and post-operative complications in patients who underwent supramalleolar corrective osteotomies (Table 1).
Table 1.
Literature review regarding complications in patients who underwent supramalleolar osteotomies
| Study | LOE | Patients | Surgical technique | Complications |
|---|---|---|---|---|
| Cheng et al. (2001) [59] | IV | 18 (18 ankles) | Medial opening wedge OT with oblique OT of the fibula (18) | Late infection (1), implant failure with delayed union (2) |
| Harstall et al. (2007) [60] | IV | 9 (9 ankles) | Lateral closing wedge OT (9) | None |
| Hintermann et al. (2008) [61] | IV | 74 (74 ankles) | Medial closing wedge OT (38), medial opening wedge OT (8), lateral closing wedge OT (11), others (17) | Progression of ankle OA requiring TAR (2), unmanageable ankle instability requiring ankle arthrodesis (1) |
| Horn et al. (2011) [62] | IV | 52 (52 ankles) | Six-axis deformity correction using circular external Ilizarov fixation (52) | Superficial pin site infections (27), cellulitis requiring i.v. antibiotics (4), osteomyelitis requiring surgical debridement (1), non-union (3), septic ankle arthritis requiring arthrotomy and debridement (2), subsequent ankle arthrodesis due to recurrence of pain (3) |
| Knupp et al. (2008) [53] | IV | 12 (12 ankles) | Medial opening wedge OT or lateral closing wedge OT (12) | None |
| Knupp et al. (2009) [55] | IV | 12 (12 ankles) | Medial opening wedge OT (7), lateral closing wedge OT (5) | None |
| Knupp et al. (2011) [6] | II | 92 (94 ankles) | Medial closing wedge OT (61), lateral closing wedge OT or medial opening wedge OT (33) | Superficial wound healing problems (5), deep infection requiring surgical debridement (1), reconstruction of anterior tibial tendon due to laceration (1), painful neuroma of the saphenous nerve (2), progression of ankle OA requiring TAR (9) or ankle arthrodesis (1) |
| Lee and Cho (2009) [63] | V | n.a. | Oblique medial opening wedge OT without fibular OT for varus deformity | None |
| Neumann et al. (2007) [64] | IV | 27 (27 ankles) | Lateral closing wedge OT (27) | Progression of ankle OA requiring TAR (3) or ankle arthrodesis (3) |
| Pagenstert et al. (2007) [65] | IV | 35 (35 ankles) | Medial closing wedge OT (18), medial opening wedge OT (7), lateral closing wedge OT (4), others (6) | Progression of ankle OA requiring TAR (3), recurrent deformity (2), non-union requiring grafting (1), superficial wound infection requiring debridement (1), delayed wound healing (1), deep vein thrombosis (1) |
| Pagenstert et al. (2008) [56] | II | 35 (35 ankles) | n.a. | Progression of ankle OA requiring TAR (3), non-union (2), recurrent deformity (2), wound healing problems (2), painful hardware requiring implant removal (7) |
| Pagenstert et al. (2009) [66] | IV | 14 (14 ankles) | Medial closing wedge OT (14) | Progression of ankle OA requiring TAR (2), non-union requiring grafting (1), deformity undercorrection requiring revision surgery (1) |
| Stamatis et al. (2003) [67] | IV | 12 (13 ankles) | Medial closing wedge OT (7), medial opening wedge OT (6) | Delayed union requiring bone grafting (1), decreased ankle ROM (3), superficial infection (1) |
| Takakura et al. (1995) [68] | IV | 18 (18 ankles) | Medial opening -wedge OT (18) | Delayed union (4), undercorrection (2) |
| Takakura et al. (1998) [69] | IV | 9 (9 ankles) | Medial opening wedge OT (9) | Delayed union (2), decreased ROM (6), persistent medial pain (2) |
i.v. intravenous, LOE level of evidence, n.a. not available, OA osteoarthritis, OT osteotomy, ROM range of motion, TAR total ankle replacement
Intra-operative complications may include injuries of neurovascular structures and tendons. Therefore, exact anatomical knowledge of surgical approaches is required. Wound healing problems and infections may be resolved by i.v. antibiotics and/or surgical debridement and irrigation.
Malunion or non-union at the osteotomy site may occur in the short or medium term after realignment surgery. Possible reasons for these complications include inappropriate surgical technique (e.g. compromising the opposite cortex), non-anatomical reduction of the osteotomy or secondary displacement of the osteotomy (e.g. due to non-compliance during the post-operative rehabilitation or hardware failure).
In patients with painful hardware, this should be removed after osseous healing of the osteotomy has been confirmed clinically and radiographically (e.g. using CT or SPECT/CT).
A possible post-operative complication after reconstructive surgery is the progression of the osteoarthritic process requiring further surgical treatment (e.g. total ankle replacement or ankle arthrodesis). In a prospective study by Knupp et al. [6] including 94 ankles with varus or valgus deformity ten ankles failed and were converted to total ankle replacement (nine ankles) or ankle arthrodesis (one ankle). Patients with type I valgus deformity (talar tilt ≤4°, congruent joint) where the fibular length was not adjusted, patients with type III varus deformity (joint space narrowing in the medial gutter) and patients with ankle joint instability had tendencies towards worse outcome or failures [6].
Results after realignment surgery
Realignment surgery as a joint-preserving surgical treatment option in patients with asymmetric painful ankle OA is gaining increasing acceptance among foot and ankle surgeons. The short- and midterm results following realignment surgery of the ankle joint in the current literature are very promising (Table 2).
Table 2.
Literature review regarding functional outcome in patients who underwent supramalleolar osteotomies
| Study | LOE | Patients | Follow-up (years) | Surgical technique | Pain relief | Functional outcome | ROM |
|---|---|---|---|---|---|---|---|
| Cheng et al. (2001) [59] | IV | 18 (18 ankles) | 4.0 (2.1–6.8) | Medial opening wedge OT with oblique OT of the fibula (18) | 24.4 → 47.5a | 25.2 → 41.0b | n.a. |
| Harstall et al. (2007) [60] | IV | 9 (9 ankles) | 4.7 (1.3–7.3) | Lateral closing wedge OT (9) | 16 ± 8.8 → 30 ± 7.1c | 48 ± 16.0 → 74 ± 11.7d | n.a. |
| Hintermann et al. (2011) [47] | IV | 48 (48 ankles) | 7.1 (2–15) | Medial closing wedge OT (45), lateral opening wedge OT (3) | 41 patients pain-free, 6 patients VAS 2.1 | 48 → 86d | 41.2° → 40.1° |
| Knupp et al. (2011) [6] | II | 92 (94 ankles) | 3.6 (1.0–10.5) | Medial closing wedge OT (61), lateral closing wedge OT or medial opening wedge OT (33) | 4.6 ± 1.9 → 2.8 ± 2.3e | 55.6 ± 17.2 → 72.8 ± 18.9d | n.a. |
| Knupp et al. (2012) [42] | IV | 14 (14 ankles) | 4.2 (2.0–8.2) | Medial closing wedge OT (14) | 4.1 ± 1.7 → 2.2 ± 1.5e | 51.6 ± 12.3 → 77.8 ± 11.8d | 25 ± 12° → 29 ± 9° |
| Lee et al. (2011) [70] | IV | 16 (16 ankles) | 2.3 (1.0–6.5) | Medial opening wedge OT with oblique OT of the fibula (16) | n.a. | 62.3 ± 8.9 → 82.1 ± 11.4d | n.a. |
| Pagenstert et al. (2008) [56] | II | 35 (35 ankles) | 5.0 (3.0–10.5) | n.a. | 7.0 ± 1.6 → 2.7 ± 1.6e | 38.5 ± 17.2 → 85.4 ± 12.4d | 32.8 ± 14.0° → 37.7 ± 9.4° |
| Stamatis et al. (2003) [67] | IV | 12 (13 ankles) | 2.8 (1.0–4.9) | Medial closing wedge OT (7), medial opening wedge OT (6) | 14.6 ± 10.5 → 32.3 ± 5.9c | 53.8 ± 19.3 → 87.0 ± 10.1d | n.a. |
| Takakura et al. (1995) [68] | IV | 18 (18 ankles) | 6.9 (2.7–12.1) | Medial opening wedge OT (18) | 16.4 ± 4.6 → 34.6 ± 5.3f | 39.3 ± 4.1 → 48.4 ± 3.9g | n.a. |
| Takakura et al. (1998) [69] | IV | 9 (9 ankles) | 7.3 (2.3–13.2) | Medial opening wedge OT (9) | 20.0 ± 7.1 → 34.4 ± 5.3f | 48.9 ± 15.3 → 52.8 ± 12.0g | 62.9 ± 9.6° → 54.5 ± 9.8° |
LOE level of evidence, n.a. not available, OT osteotomy, ROM range of motion
aUsing 50-point pain scale
bUsing 50-point functional scale: functional outcome (40), ROM (10)
cUsing American Orthopaedic Foot and Ankle Society (AOFAS) pain subscale
dUsing AOFAS hindfoot score
eUsing visual analogue scale (VAS)
fUsing 40-point pain scale
gUsing 60-point functional scale: walking (20), activities of daily living (20), ROM (20)
Takakura et al. [68] presented midterm results of 18 patients who underwent opening wedge osteotomy due to varus ankle OA. The mean follow-up in this study was six years and 11 months with a range between 2.7 and 12.1 years. In the cohort, excellent, good and fair results were observed in six, nine and three ankles respectively. Fair results were explained by undercorrection of the deformity in two cases and little remaining articular cartilage in one case. In general, most patients experienced substantial functional improvement and post-operative pain relief [68]. The same group reported three years later additional results of nine patients who underwent medial opening wedge osteotomy with post-traumatic varus ankle deformity [69]. At a mean follow-up of 7.3 years the post-operative results were graded as excellent, good and fair in four, two and three patients, respectively. Osseous union at the site of the supramalleolar osteotomy occurred at a mean of 8.7 months post-operatively [69].
Cheng et al. [59] performed low tibial osteotomy in 18 patients including 6 cases with post-traumatic and 12 cases with degenerative ankle OA. At a mean follow-up of four years, ten and eight patients experienced good and excellent results, respectively [59].
Stamatis et al. [67] treated 23 ankles in 22 patients with supramalleolar osteotomies for painful distal tibial malalignment of at least 10° with or without radiographic evidence of ankle OA. All varus deformities were corrected using a medial opening wedge osteotomy and all valgus deformities using a medial closing wedge osteotomy. In two patients secondary surgery was necessary due to non-union of the osteotomy. The remaining osteotomies healed at a mean time of 14 weeks. Significant improvement of the American Orthopaedic Foot and Ankle Society (AOFAS) score and Takakura ankle score was observed in this cohort with no differences regarding the surgical technique (opening wedge vs closing wedge). In all patients substantial improvement of radiographic parameters and no evidence of progression of ankle OA was observed [67].
Pagenstert et al. [65] reported midterm results obtained from 35 consecutive patients who underwent realignment surgery due to varus or valgus ankle OA. At a mean follow-up of five years significant pain relief and functional improvement, including increased range of motion, was observed. Revision was necessary in ten ankles, including three patients who underwent total ankle replacement [65].
Neumann et al. [64] performed supramalleolar lateral closing wedge osteotomy in 27 patients with varus OA of the ankle. The mean pre-operative varus deformity of 27° was corrected to a mean of 6° varus post-operatively. Subsequently, three patients underwent total ankle replacement and three patients underwent ankle arthrodesis [64].
Harstall et al. [60] treated nine patients with varus ankle OA by supramalleolar lateral closing wedge osteotomy. There were no intra- or perioperative complications, with a mean osseous healing of 10 weeks. At a mean follow-up of 4.7 months, statistically significant improvement of clinical scores was observed. In one patient an ankle arthrodesis was performed due to progressive ankle OA [60].
Lee et al. [70] performed supramalleolar tibial osteotomy combined with fibular osteotomy in 16 patients for treatment of moderate medial ankle OA. The mean follow-up in this patient cohort was 2.3 years with a range between one and 6.5 years. In general, the mean AOFAS score, mean Takakura OA stage and mean values of all radiographic parameters improved significantly after the realignment surgery. In this study, patients with minimal talar tilt and neutral or varus heel alignment had a better post-operative outcome [70].
Knupp et al. [6] established a new classification of supramalleolar deformities and presented a treatment algorithm. This prospective study included 92 patients (94 ankles) with asymmetric ankle OA. At a mean follow-up of 3.6 years a significant improvement of clinical scores was observed with post-operative reduction of radiographic OA signs in patients with mid-stage ankle OA. In ten patients, conversion to total ankle replacement or ankle arthrodesis was necessary due to progression of ankle OA [6].
Hintermann et al. [47] performed a prospective study including 48 patients with malunited, pronation-external rotation fracture of the ankle. In all patients valgus malalignment of the distal tibia and malunion of the fibula were corrected. At a mean follow-up of 7.1 years, good or excellent results were obtained in 42 patients. Most patients (47 patients) were pain-free and six patients reported moderate pain with a mean visual analogue scale (VAS) score of 2.1 points. In one patient total ankle replacement was performed 26 months after corrective surgery [47].
Knupp et al. [42] treated 14 patients with overcorrected clubfoot deformity with medial closing wedge supramalleolar osteotomy. Additional osteotomies were performed if necessary including anterior closing wedge tibial osteotomy, calcaneal osteotomy and/or first cuneiform osteotomy. Osseous healing at the site of osteotomies occurred within eight weeks in all cases. Post-operatively, improvement of radiographic parameters, good functional results and post-operative pain relief were observed in all patients [42].
Future aspects of realignment surgery of the ankle joint
In 1995 Takakura et al. [68] published a clinical study entitled “Low tibial osteotomy for osteoarthritis of the ankle. Results of a new operation in 18 patients” in the Journal of Bone and Joint Surgery (British Volume). Japanese colleagues from Nara Medical University reported encouraging results in patients who underwent medial opening wedge osteotomy due to varus ankle OA [68]. Since then realignment procedure has been constantly gaining more acceptance as a therapeutic option in patients with moderate asymmetric ankle OA. Surgical technique, clinical outcomes and indications and contraindications for realignment surgery have been a “hot topic” in most foot and ankle symposiums in the last decade.
In our experience, supramalleolar realignment surgery predictably leads good clinical results, correction of the hindfoot deformity and high patient satisfaction [53, 55, 56, 65, 66]. One key for long-term success is appropriate patient selection. All absolute or relative contraindications should be recognised. The origin and dimensions of the deformity should be carefully analysed during exacting pre-operative planning. Concomitant problems, including additional osseous deformities (e.g. inframalleolar deformities—valgus or varus position of the heel) or ligamental instabilities, should be recognised and addressed as a one-stage procedure. Recently, Tanaka—one of the authors of the first publication from the year 1995 [68]—published a review article presenting his philosophy and treatment algorithm for realignment surgery entitled “The concept of ankle joint preserving surgery: why does supramalleolar osteotomy work and how to decide when to do an osteotomy or joint replacement” [11]. He underlined the importance of correct patient selection and pointed to the fact that there are no comparative studies between supramalleolar osteotomy and other surgical treatment options [11].
One of the main advantages of realignment surgery is that it is a joint-preserving procedure. Most patients show high satisfaction with the surgery [47, 65] allowing them to return to normal sports and recreational activities [56]. Even in cases with progression of degenerative changes of the tibiotalar joint requiring a second surgery (total ankle replacement or ankle arthrodesis) the patients may benefit from realignment surgery. It has been shown that total ankle replacement performed in a well-aligned hindfoot showed a better post-operative outcome [71–75].
Summary
Patients with supramalleolar valgus or varus deformity have pathologically altered pressure distribution patterns in the tibiotalar joint [76–79], resulting in the development of asymmetric ankle OA. Realignment surgery may restore normal biomechanics of the ankle joint with pain relief, functional improvement and slowing of the degenerative process [47, 65, 68, 69]. Additional long-term studies should be performed to address positive and negative predictors influencing the long-term success after this surgery.
References
- 1.Glazebrook M, Daniels T, Younger A, Foote CJ, Penner M, Wing K, Lau J, Leighton R, Dunbar M. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J Bone Joint Surg Am. 2008;90(3):499–505. doi: 10.2106/JBJS.F.01299. [DOI] [PubMed] [Google Scholar]
- 2.Buckwalter JA, Saltzman C, Brown T (2004) The impact of osteoarthritis: implications for research. Clin Orthop Relat Res (427 Suppl):S6–S15 [DOI] [PubMed]
- 3.Horváth G, Than P, Bellyei A, Kranicz J, Illés T. Prevalence of degenerative joint complaints of the lower extremity: a representative study. Int Orthop. 2006;30(2):118–122. doi: 10.1007/s00264-005-0033-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horisberger M, Hintermann B, Valderrabano V. Alterations of plantar pressure distribution in posttraumatic end-stage ankle osteoarthritis. Clin Biomech (Bristol, Avon) 2009;24(3):303–307. doi: 10.1016/j.clinbiomech.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 5.Horisberger M, Valderrabano V, Hintermann B. Posttraumatic ankle osteoarthritis after ankle-related fractures. J Orthop Trauma. 2009;23(1):60–67. doi: 10.1097/BOT.0b013e31818915d9. [DOI] [PubMed] [Google Scholar]
- 6.Knupp M, Stufkens SA, Bolliger L, Barg A, Hintermann B. Classification and treatment of supramalleolar deformities. Foot Ankle Int. 2011;32:1023–1031. doi: 10.3113/FAI.2011.1023. [DOI] [PubMed] [Google Scholar]
- 7.Valderrabano V, Horisberger M, Russell I, Dougall H, Hintermann B. Etiology of ankle osteoarthritis. Clin Orthop Relat Res. 2009;467(7):1800–1806. doi: 10.1007/s11999-008-0543-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogilvie-Harris DJ, Sekyi-Otu A. Arthroscopic debridement for the osteoarthritic ankle. Arthroscopy. 1995;11(4):433–436. doi: 10.1016/0749-8063(95)90197-3. [DOI] [PubMed] [Google Scholar]
- 9.Saltzman CL, Hillis SL, Stolley MP, Anderson DD, Amendola A. Motion versus fixed distraction of the joint in the treatment of ankle osteoarthritis: a prospective randomized controlled trial. J Bone Joint Surg Am. 2012;94(11):961–970. doi: 10.2106/JBJS.K.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wiewiorski M, Barg A, Valderrabano V (2013) Cartilage reconstruction in osteochondral lesions of the talus (OCLT). Foot Ankle Clin (accepted for publication) [DOI] [PubMed]
- 11.Tanaka Y. The concept of ankle joint preserving surgery: why does supramalleolar osteotomy work and how to decide when to do an osteotomy or joint replacement. Foot Ankle Clin. 2012;17(4):545–553. doi: 10.1016/j.fcl.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Ahmad J, Raikin SM. Ankle arthrodesis: the simple and the complex. Foot Ankle Clin. 2008;13(3):381–400. doi: 10.1016/j.fcl.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 13.Barg A, Knupp M, Henninger HB, Zwicky L, Hintermann B. Total ankle replacement using HINTEGRA, an unconstrained, three-component system: surgical technique and pitfalls. Foot Ankle Clin. 2012;17(4):607–635. doi: 10.1016/j.fcl.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 14.Valderrabano V, Pagenstert GI, Müller AM, Paul J, Henninger HB, Barg A. Mobile- and fixed-bearing total ankle prostheses: is there really a difference? Foot Ankle Clin. 2012;17(4):565–585. doi: 10.1016/j.fcl.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 15.Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am. 2001;83-A(2):219–228. doi: 10.2106/00004623-200102000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Glazebrook MA, Ganapathy V, Bridge MA, Stone JW, Allard JP. Evidence-based indications for ankle arthroscopy. Arthroscopy. 2009;25(12):1478–1490. doi: 10.1016/j.arthro.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Haddad SL, Coetzee JC, Estok R, Fahrbach K, Banel D, Nalysnyk L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg Am. 2007;89(9):1899–1905. doi: 10.2106/JBJS.F.01149. [DOI] [PubMed] [Google Scholar]
- 18.Brown TD, Johnston RC, Saltzman CL, Marsh JL, Buckwalter JA. Posttraumatic osteoarthritis: a first estimate of incidence, prevalence, and burden of disease. J Orthop Trauma. 2006;20(10):739–744. doi: 10.1097/01.bot.0000246468.80635.ef. [DOI] [PubMed] [Google Scholar]
- 19.Egloff C, Hügle T, Valderrabano V (2012) Biomechanics and pathomechanisms of osteoarthritis. Swiss Med Wkly 142:w13583. doi:10.4414/smw.2012.13583 [DOI] [PubMed]
- 20.Saltzman CL, Salamon ML, Blanchard GM, Huff T, Hayes A, Buckwalter JA, Amendola A. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44–46. [PMC free article] [PubMed] [Google Scholar]
- 21.Stufkens SA, Knupp M, Horisberger M, Lampert C, Hintermann B. Cartilage lesions and the development of osteoarthritis after internal fixation of ankle fractures: a prospective study. J Bone Joint Surg Am. 2010;92(2):279–286. doi: 10.2106/JBJS.H.01635. [DOI] [PubMed] [Google Scholar]
- 22.Hintermann B, Boss A, Schäfer D. Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med. 2002;30(3):402–409. doi: 10.1177/03635465020300031601. [DOI] [PubMed] [Google Scholar]
- 23.Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006;34(4):612–620. doi: 10.1177/0363546505281813. [DOI] [PubMed] [Google Scholar]
- 24.Lübbeke A, Salvo D, Stern R, Hoffmeyer P, Holzer N, Assal M. Risk factors for post-traumatic osteoarthritis of the ankle: an eighteen year follow-up study. Int Orthop. 2012;36(7):1403–1410. doi: 10.1007/s00264-011-1472-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Easley ME. Surgical treatment of the arthritic varus ankle. Foot Ankle Clin. 2012;17(4):665–686. doi: 10.1016/j.fcl.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 26.Barg A, Pagenstert GI, Leumann AG, Müller AM, Henninger HB, Valderrabano V. Treatment of the arthritic valgus ankle. Foot Ankle Clin. 2012;17(4):647–663. doi: 10.1016/j.fcl.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 27.Valderrabano V, Miska M, Leumann A, Wiewiorski M. Reconstruction of osteochondral lesions of the talus with autologous spongiosa grafts and autologous matrix-induced chondrogenesis. Am J Sports Med. 2013;41(3):519–527. doi: 10.1177/0363546513476671. [DOI] [PubMed] [Google Scholar]
- 28.Barg A, Elsner A, Anderson AE, Hintermann B. The effect of three-component total ankle replacement malalignment on clinical outcome: pain relief and functional outcome in 317 consecutive patients. J Bone Joint Surg Am. 2011;93(21):1969–1978. doi: 10.2106/JBJS.J.01415. [DOI] [PubMed] [Google Scholar]
- 29.Cenni F, Leardini A, Cheli A, Catani F, Belvedere C, Romagnoli M, Giannini S. Position of the prosthesis components in total ankle replacement and the effect on motion at the replaced joint. Int Orthop. 2012;36(3):571–578. doi: 10.1007/s00264-011-1323-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Espinosa N, Walti M, Favre P, Snedeker JG. Misalignment of total ankle components can induce high joint contact pressures. J Bone Joint Surg Am. 2010;92(5):1179–1187. doi: 10.2106/JBJS.I.00287. [DOI] [PubMed] [Google Scholar]
- 31.Lee JJ, Patel R, Biermann JS, Dougherty PJ. The musculoskeletal effects of cigarette smoking. J Bone Joint Surg Am. 2013;95(9):850–859. doi: 10.2106/JBJS.L.00375. [DOI] [PubMed] [Google Scholar]
- 32.Saltzman CL, el-Khoury GY. The hindfoot alignment view. Foot Ankle Int. 1995;16(9):572–576. doi: 10.1177/107110079501600911. [DOI] [PubMed] [Google Scholar]
- 33.Knupp M, Pagenstert GI, Barg A, Bolliger L, Easley ME, Hintermann B. SPECT-CT compared with conventional imaging modalities for the assessment of the varus and valgus malaligned hindfoot. J Orthop Res. 2009;27(11):1461–1466. doi: 10.1002/jor.20922. [DOI] [PubMed] [Google Scholar]
- 34.Pagenstert GI, Barg A, Leumann AG, Rasch H, Müller-Brand J, Hintermann B, Valderrabano V. SPECT-CT imaging in degenerative joint disease of the foot and ankle. J Bone Joint Surg Br. 2009;91(9):1191–1196. doi: 10.1302/0301-620X.91B9.22570. [DOI] [PubMed] [Google Scholar]
- 35.Kretzschmar M, Wiewiorski M, Rasch H, Jacob AL, Bilecen D, Walter MA, Valderrabano V. 99mTc-DPD-SPECT/CT predicts the outcome of imaging-guided diagnostic anaesthetic injections: a prospective cohort study. Eur J Radiol. 2011;80(3):e410–e415. doi: 10.1016/j.ejrad.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 36.Knupp M, Ledermann H, Magerkurth O, Hintermann B. The surgical tibiotalar angle: a radiologic study. Foot Ankle Int. 2005;26(9):713–716. doi: 10.1177/107110070502600909. [DOI] [PubMed] [Google Scholar]
- 37.Inman VT. The joints of the ankle. Baltimore: Williams & Wilkins; 1976. [Google Scholar]
- 38.Stufkens SA, Barg A, Bolliger L, Stucinskas J, Knupp M, Hintermann B. Measurement of the medial distal tibial angle. Foot Ankle Int. 2011;32:288–293. doi: 10.3113/FAI.2011.0288. [DOI] [PubMed] [Google Scholar]
- 39.Barg A, Harris MD, Henninger HB, Amendola RL, Saltzman CL, Hintermann B, Anderson AE. Medial distal tibial angle: comparison between weightbearing mortise view and hindfoot alignment view. Foot Ankle Int. 2012;33(8):655–661. doi: 10.3113/FAI.2012.0655. [DOI] [PubMed] [Google Scholar]
- 40.Tanaka Y, Takakura Y, Fujii T, Kumai T, Sugimoto K. Hindfoot alignment of hallux valgus evaluated by a weightbearing subtalar x-ray view. Foot Ankle Int. 1999;20(10):640–645. doi: 10.1177/107110079902001005. [DOI] [PubMed] [Google Scholar]
- 41.Cox JS, Hewes TF. “Normal” talar tilt angle. Clin Orthop Relat Res. 1979;140:37–41. [PubMed] [Google Scholar]
- 42.Knupp M, Barg A, Bolliger L, Hintermann B. Reconstructive surgery for overcorrected clubfoot in adults. J Bone Joint Surg Am. 2012;94(15):e1101–e1107. doi: 10.2106/JBJS.K.00538. [DOI] [PubMed] [Google Scholar]
- 43.Warnock KM, Johnson BD, Wright JB, Ambrose CG, Clanton TO, McGarvey WC. Calculation of the opening wedge for a low tibial osteotomy. Foot Ankle Int. 2004;25(11):778–782. doi: 10.1177/107110070402501104. [DOI] [PubMed] [Google Scholar]
- 44.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 45.Chu A, Weiner L. Distal fibula malunions. J Am Acad Orthop Surg. 2009;17(4):220–230. doi: 10.5435/00124635-200904000-00003. [DOI] [PubMed] [Google Scholar]
- 46.Thordarson DB, Motamed S, Hedman T, Ebramzadeh E, Bakshian S. The effect of fibular malreduction on contact pressures in an ankle fracture malunion model. J Bone Joint Surg Am. 1997;79(12):1809–1815. doi: 10.2106/00004623-199712000-00006. [DOI] [PubMed] [Google Scholar]
- 47.Hintermann B, Barg A, Knupp M. Corrective supramalleolar osteotomy for malunited pronation-external rotation fractures of the ankle. J Bone Joint Surg Br. 2011;93(10):1367–1372. doi: 10.1302/0301-620X.93B10.26944. [DOI] [PubMed] [Google Scholar]
- 48.Weber BG, Simpson LA. Corrective lengthening osteotomy of the fibula. Clin Orthop Relat Res. 1985;199(199):61–67. [PubMed] [Google Scholar]
- 49.Hintermann B, Valderrabano V. Lateral column lengthening by calcaneal osteotomy. Tech Foot Ankle. 2003;2:84–90. doi: 10.1097/00132587-200306000-00003. [DOI] [Google Scholar]
- 50.Hintermann B, Valderrabano V, Kundert HP. Lengthening of the lateral column and reconstruction of the medial soft tissue for treatment of acquired flatfoot deformity associated with insufficiency of the posterior tibial tendon. Foot Ankle Int. 1999;20(10):622–629. doi: 10.1177/107110079902001002. [DOI] [PubMed] [Google Scholar]
- 51.Dolan CM, Henning JA, Anderson JG, Bohay DR, Kornmesser MJ, Endres TJ. Randomized prospective study comparing tri-cortical iliac crest autograft to allograft in the lateral column lengthening component for operative correction of adult acquired flatfoot deformity. Foot Ankle Int. 2007;28(1):8–12. doi: 10.3113/FAI.2007.0002. [DOI] [PubMed] [Google Scholar]
- 52.Grier KM, Walling AK. The use of tricortical autograft versus allograft in lateral column lengthening for adult acquired flatfoot deformity: an analysis of union rates and complications. Foot Ankle Int. 2010;31(9):760–769. doi: 10.3113/FAI.2010.0760. [DOI] [PubMed] [Google Scholar]
- 53.Knupp M, Pagenstert G, Valderrabano V, Hintermann B. Osteotomies in varus malalignment of the ankle. Oper Orthop Traumatol. 2008;20(3):262–273. doi: 10.1007/s00064-008-1308-9. [DOI] [PubMed] [Google Scholar]
- 54.Barg A, Pagenstert G, Leumann A, Valderrabano V. Malleolar osteotomy—osteotomy as approach. Orthopade. 2013;42(5):309–321. doi: 10.1007/s00132-012-2007-7. [DOI] [PubMed] [Google Scholar]
- 55.Knupp M, Stufkens SA, Pagenstert G, Hintermann B, Valderrabano V. Supramalleolar osteotomy for tibiotalar varus malalignment. Tech Foot Ankle. 2009;8:17–23. doi: 10.1097/BTF.0b013e31818ee7b4. [DOI] [Google Scholar]
- 56.Pagenstert G, Leumann A, Hintermann B, Valderrabano V. Sports and recreation activity of varus and valgus ankle osteoarthritis before and after realignment surgery. Foot Ankle Int. 2008;29(10):985–993. doi: 10.3113/FAI.2008.0985. [DOI] [PubMed] [Google Scholar]
- 57.Becker AS, Myerson MS. The indications and technique of supramalleolar osteotomy. Foot Ankle Clin. 2009;14(3):549–561. doi: 10.1016/j.fcl.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 58.Benthien RA, Myerson MS. Supramalleolar osteotomy for ankle deformity and arthritis. Foot Ankle Clin. 2004;9(3):475–487. doi: 10.1016/j.fcl.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 59.Cheng YM, Huang PJ, Hong SH, Lin SY, Liao CC, Chiang HC, Chen LC. Low tibial osteotomy for moderate ankle arthritis. Arch Orthop Trauma Surg. 2001;121(6):355–358. doi: 10.1007/s004020000243. [DOI] [PubMed] [Google Scholar]
- 60.Harstall R, Lehmann O, Krause F, Weber M. Supramalleolar lateral closing wedge osteotomy for the treatment of varus ankle arthrosis. Foot Ankle Int. 2007;28(5):542–548. doi: 10.3113/FAI.2007.0542. [DOI] [PubMed] [Google Scholar]
- 61.Hintermann B, Knupp M, Barg A. Osteotomies of the distal tibia and hindfoot for ankle realignment. Orthopade. 2008;37(3):212–213. doi: 10.1007/s00132-008-1214-8. [DOI] [PubMed] [Google Scholar]
- 62.Horn DM, Fragomen AT, Rozbruch SR. Supramalleolar osteotomy using circular external fixation with six-axis deformity correction of the distal tibia. Foot Ankle Int. 2011;32(10):986–993. doi: 10.3113/FAI.2011.0986. [DOI] [PubMed] [Google Scholar]
- 63.Lee KB, Cho YJ. Oblique supramalleolar opening wedge osteotomy without fibular osteotomy for varus deformity of the ankle. Foot Ankle Int. 2009;30(6):565–567. doi: 10.3113/FAI.2009.0565. [DOI] [PubMed] [Google Scholar]
- 64.Neumann HW, Lieske S, Schenk K. Supramalleolar, subtractive valgus osteotomy of the tibia in the management of ankle joint degeneration with varus deformity. Oper Orthop Traumatol. 2007;19(5–6):511–526. doi: 10.1007/s00064-007-1025-7. [DOI] [PubMed] [Google Scholar]
- 65.Pagenstert GI, Hintermann B, Barg A, Leumann A, Valderrabano V. Realignment surgery as alternative treatment of varus and valgus ankle osteoarthritis. Clin Orthop Relat Res. 2007;462:156–168. doi: 10.1097/BLO.0b013e318124a462. [DOI] [PubMed] [Google Scholar]
- 66.Pagenstert G, Knupp M, Valderrabano V, Hintermann B. Realignment surgery for valgus ankle osteoarthritis. Oper Orthop Traumatol. 2009;21(1):77–87. doi: 10.1007/s00064-009-1607-9. [DOI] [PubMed] [Google Scholar]
- 67.Stamatis ED, Cooper PS, Myerson MS. Supramalleolar osteotomy for the treatment of distal tibial angular deformities and arthritis of the ankle joint. Foot Ankle Int. 2003;24(10):754–764. doi: 10.1177/107110070302401004. [DOI] [PubMed] [Google Scholar]
- 68.Takakura Y, Tanaka Y, Kumai T, Tamai S. Low tibial osteotomy for osteoarthritis of the ankle. Results of a new operation in 18 patients. J Bone Joint Surg Br. 1995;77(1):50–54. [PubMed] [Google Scholar]
- 69.Takakura Y, Takaoka T, Tanaka Y, Yajima H, Tamai S. Results of opening-wedge osteotomy for the treatment of a post-traumatic varus deformity of the ankle. J Bone Joint Surg Am. 1998;80(2):213–218. doi: 10.2106/00004623-199802000-00008. [DOI] [PubMed] [Google Scholar]
- 70.Lee WC, Moon JS, Lee K, Byun WJ, Lee SH. Indications for supramalleolar osteotomy in patients with ankle osteoarthritis and varus deformity. J Bone Joint Surg Am. 2011;93(13):1243–1248. doi: 10.2106/JBJS.J.00249. [DOI] [PubMed] [Google Scholar]
- 71.Brunner S, Knupp M, Hintermann B. Total ankle replacement for the valgus unstable osteoarthritic ankle. Tech Foot Ankle. 2010;9:165–174. doi: 10.1097/BTF.0b013e3181fc861c. [DOI] [Google Scholar]
- 72.Kim BS, Choi WJ, Kim YS, Lee JW. Total ankle replacement in moderate to severe varus deformity of the ankle. J Bone Joint Surg Br. 2009;91(9):1183–1190. doi: 10.1302/0301-620X.91B9.22411. [DOI] [PubMed] [Google Scholar]
- 73.Kim BS, Lee JW. Total ankle replacement for the varus unstable osteoarthritic ankle. Tech Foot Ankle. 2010;9:157–167. doi: 10.1097/BTF.0b013e3181fcde82. [DOI] [Google Scholar]
- 74.Knupp M, Stufkens SA, Bolliger L, Brunner S, Hintermann B. Total ankle replacement and supramalleolar osteotomies for malaligned osteoarthritis ankle. Tech Foot Ankle. 2010;9:175–181. doi: 10.1097/BTF.0b013e3181ff273e. [DOI] [Google Scholar]
- 75.Wood PL, Deakin S. Total ankle replacement. The results in 200 ankles. J Bone Joint Surg Br. 2003;85(3):334–341. doi: 10.1302/0301-620X.85B3.13849. [DOI] [PubMed] [Google Scholar]
- 76.Knupp M, Stufkens SA, van Bergen CJ, Blankevoort L, Bolliger L, van Dijk CN, Hintermann B. Effect of supramalleolar varus and valgus deformities on the tibiotalar joint: a cadaveric study. Foot Ankle Int. 2011;32(6):609–615. doi: 10.3113/FAI.2011.0609. [DOI] [PubMed] [Google Scholar]
- 77.Ting AJ, Tarr RR, Sarmiento A, Wagner K, Resnick C. The role of subtalar motion and ankle contact pressure changes from angular deformities of the tibia. Foot Ankle. 1987;7(5):290–299. doi: 10.1177/107110078700700505. [DOI] [PubMed] [Google Scholar]
- 78.Tarr RR, Resnick CT, Wagner KS, Sarmiento A. Changes in tibiotalar joint contact areas following experimentally induced tibial angular deformities. Clin Orthop Relat Res. 1985;199:72–80. [PubMed] [Google Scholar]
- 79.Wagner KS, Tarr RR, Resnick C, Sarmiento A. The effect of simulated tibial deformities on the ankle joint during the gait cycle. Foot Ankle. 1984;5(3):131–141. doi: 10.1177/107110078400500306. [DOI] [PubMed] [Google Scholar]