Abstract
No consensus had been reached about the optimal method for syndesmotic fixation. The present study analysed syndesmotic fixation based on the highest level of clinical evidence in order to obtain more reliable results. Medline, Embase and Cochrane database were searched through the OVID retrieval engine. Manual searching was undertaken afterward to identify additional studies. Only randomized controlled trials (RCT) and prospective comparative studies were selected for final inclusion. Study screening and data extraction were completed independently by two reviewers. All study characteristics were summarized into a table. The extracted data were used for data analysis. Twelve studies were finally included: six of them were RCTs, two were quasi-randomized studies and four were prospective comparative studies. Four comparisons with traditional metallic screw were identified in terms of bioabsorbable screws, tricortical fixation method, suture-button device as well as non-fixation choice in low syndesmotic injuries. Both absorbable screws and the tricortical fixation method showed almost no better results than traditional quadricortical metallic screw (p > 0.05). Additionally, existing studies could not illustrate their efficiency of reducing hardware removal rate. The suture button technique had significantly better functional score (p = 0.003), ankle motion (p = 0.02), time to full weightbearing (p < 0.0001) and much less complications (p = 0.0008) based on short and intermediate term follow-up data. Transfixation in low syndesmotic injuries showed poorer results than the non fixed group in all outcome measurements, but didn’t reach a significant level (p > 0.05). The present evidence still couldn’t find superior performance of the bioabsorbable screw and tricortical fixation method. Their true effects in decreasing second operation rate need further specific studies. Better results of the suture-button made it a promising technique, but it still needs long-term testing and cost-efficiency studies. The patients with low syndemotic injuries should be well assessed before fixation determination and the indication of screw placement in such conditions needs to be further defined.
Keywords: Ankle fractures, Syndesmotic injuries, Suture button technique, Bioabsorbable screw, Distal tibio-fibular injury
Introduction
It was estimated that 90,000 ankle fractures occur in the United Kingdom every year in the population aged 20–65 years. Among them, up to 13 % of fractures had associated distal syndesmotic injuries [1, 2]. Till now, no gold standard was available for diagnosis of tibiofibular syndesmotic injury [3, 4]. The current prevailing methods were intra-operative hook test or 7.5NM external rotation stress test [5–8].
Anatomical reduction of the ankle mortise is a critical factor for satisfactory functional recovery and even 1 mm lateral shift of the talus would cause a decrease of the tibiotalar contact area by 42 % [9]. Various syndesmotic fixation techniques have been introduced over recent decades including transyndesmotic screws [10, 11], Kirschner wires [12], syndesmotic staples [13], syndesmotic bolt [14], bioabsorbable implants [15] and recently emerged suture-button devices [16]. Nevertheless, none of them has been proved to be optimal. Transyndesmotic screw was the most commonly used method but also has obvious flaws both clinically and biomechanically [17, 18]. Thus, many uncertainties about the syndesmotic screw technique still exists in terms of the height of screw placement, number of cortices engaged, size of screws and necessity for screw removal [19].
Due to the great amount of controversies about distal tibiofibular syndesmotic fixation, several authors have reviewed related literature in order to find preferred opinions. Schepers [20] has compared the clinical and biomechanical outcomes of the suture-button device to the traditional syndesmotic screw and found a relatively shorter recovery period and lower removal rate in the suture-button group. He also reported there is no better result for syndesmotic screw removal [21]. Daas et al. [22] demonstrated a faster rehabilitation with suture-button fixation than syndesmotic screw.
However, all these systematic reviews didn’t limit the literature quality, therefore, a large portion of the included studies were retrospective cohort studies or case series with no control group. We suppose that these studies would bring some bias and, consequently, reduce the reliability and validity of their conclusions. Additionally, several high quality studies have been published over the past several years and, to the authors’ knowledge, high level systematic review of syndesmosis fixation is still unavailable up to now. Therefore, we believe that it is necessary to obtain the most reliable evidence with regard to the distal tibiofibular syndesmostic fixation.
Methods
Inclusion criteria
Studies that met all the following criteria were included: (1) clinical study, (2) study designs to be randomized controlled trial or prospective comparative study, (3) the main objective of the study should be directly concerning distal tibiofibular syndesmotic fixation, (4) all subjects should be adults aged more than 18 years and have been clearly diagnosed as syndesmotic injuries, (5) patients should receive operative management and internal fixation of tibiofibular syndesmosis, (6) study compares the syndesmotic fixation patients to the non-fixed group if it met above requirements, and (7) no restriction to article language.
Exclusion criteria
The literature which was excluded consisted of: (1) retrospective studies, (2) studies without a control group, (3) poor quality prospective comparative studies (obvious heterogeneities between two groups), and (4) follow-up duration of less than three months or study subjects to be less than 20 in all.
Search strategy
Retrieval was conducted by searching databases of Medline (1946 to present with daily update), Embase and Cochrane Central Register of Controlled Trials through the OVID search engine. Publication years were limited from 1990 to May 2013. In order to identify additional studies, we manually searched the database of Medline (In-Process & Other Non-Indexed Citations) and Journals @ Ovid by using the keyword of “syndesmo$” or “tibiofibular”.
Study review and selection
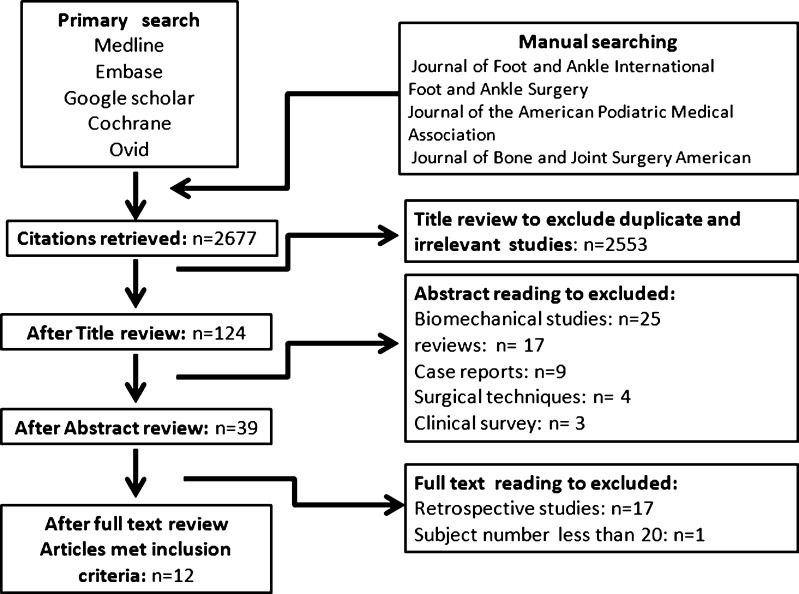
Two authors independently selected eligible studies from the primary search results using the above criteria. The included researches were checked and agreement was reached for the final determination of included studies. For each reviewer, repeated articles from different databases were first identified and the excess ones were therefore removed. Of the remainder, title screening was used to identify the articles with respect to the distal tibiofibular syndesmotic injuries or treatment. Then abstracts of each article were read to exclude biomechanical studies, case reports, reviews, clinical surveys and surgical techniques. Careful full-text review was performed for the remaining ones and only the studies which strictly met the criteria could be eventually enrolled.
Data extraction
Data extraction was completed according to a standard form which was made before the beginning of the present review. It was primarily extracted by the first author and then checked by the other two authors. The form consists of three parts which were basic information (authors and publishing years), study design and method, along with outcome measurement results.
Results
In total 1,287 references were found in the primary search. Among them, 868 articles were gained through Medline (1946 to present with daily update), Embase and Cochrane Central Register of Controlled Trials. The remaining 419 items were obtained by manually searching. Thirty clinical studies were left through screening, and fulltext review was performed according to pre-defined eligibility criteria. There were 17 retrospective studies and another one turned out to be with subject number less than 20. The whole screening process was shown in a flow diagram (Fig. 1). Therefore, 12 studies were finally included [23–34] and are summarized in Table 1.
Fig. 1.
Flow chart representing study selection
Table 1.
Included trials and characteristics
| References | Study design | LOE | Comparison | Follow-up duration | Outcome measurement | Results | Main conclusions |
|---|---|---|---|---|---|---|---|
| Thordarson [23] | RCT | Level I | Absorbable screw 17 patients stainless steel screw 15 patients | Mean 11 months | Subjective complains; ankle ROM; MCS; revision rate; complications | No difference were existed between two groups. No loss of reduction and osteolysis in all patients | PLA absorbable is an attractive alternative to reduce subsequent removal without increasing complications |
| Kaukonen et al. [24] | RCT | Level I | bioabsorbable screw 20 patients; metallic screw 18 patients | Mean 35 months; range 17–51 | Subjective evaluation; ankle ROM; MCS; Return to sports; complications | Bioabsorbable screw group had better returned to sports level and less swelling (but no significant difference). No difference in joint motion (P = 0.854) and MCS | PLA absorbable screws worked slightly better than metallic ones |
| Hu et al. [25] | Quasi-randomized study | Level II | Absorbable PDLLA screw 22 patients; metallic screw 25 patients | 13.5 ± 3.0 months | Ankle ROM; AOFAS scores; TFO; TFCS; complications | No dislocation and hardware failure in both group. No difference in AOFAS (P = 0.665); Ankle ROM (P = 0.947); TFO (P = 0.360); TFCS (P = 0.531) | PDLLA absorbable screw was a reliable treatment for syndesmotic injuries. It also obviated secondary operations |
| Sinisaari et al. [26] | Prospective comparative study | Level II | Absorbable PLA screw 18 patients; metallic screws 12 patients | 12 months | Ankle ROM; OMS scores; TFCS; TFO; revision rate; complications | No significant difference was detected in any outcome | Syndesmotic rupture fixation could be done by bioabsorbable PLA screw |
| Wikerøy et al. [27] | RCT | Level I | Tricortical screw fixation 25 patients; quadricortical screw fixation 23 patients | Mean 8.4 years; range 7.7–8.9 | Ankle ROM; OMS scores; VAS scores; syndesmotic width; synostosis; articular height; complications | No differences in OMS scores (P = 0.9); VAS scores (P = 0.8) and complication. Quadricortical fixation had better dorsiflexion (P = 0.03). | Both quadricortical and two tricortical screws fixation achieved good results in syndesmotic injuries |
| Moore et al. [28] | Quasi-randomized study | Level II | Tricortical screw fixation 59 patients; quadricortical screw fixation 61 patients | 150 days | Raidolucency; complications | No difference in loss of reduction (P = 0.871); screw breakage (P = 0.689); need for hardware removal (P = 0.731) | Three or four cortical fixation had similar clinical results and can be both used in syndesmotic ruptures |
| Høiness and Strømsøe [29] | RCT | Level I | Tricortical screw fixation 34 patients; quadricortical screw fixation 30 patients | One year | Ankle ROM; OMS score; displacement; ankle joint space; revision; complication | OMS score was significantly higher in the tricortical group at three months (P = 0.025), but no difference at one year (P = 0.192); no significant difference in joint motion | Two tricortical screws improves early function but no difference in functional score, pain and dorsiflexion at one year |
| Cottom et al. [30] | Prospective comparative study | Level II | suture-button fixation in 25 patients; metallic screw fixation in 25 patients | Mean 9.4 months | Modified AOFAS score; SF-12 score; TFO; TFCS; MCS; revision; time to full weightbearing; complications | No significant differences in weight bearing time; modified AOFAS score; SF-12 score; MCS; TFO. TFCS was significantly smaller in suture-button group | Suture-button device was as effective as traditional internal screw fixation |
| Naqvi et al. [31] | Prospective comparative study | Level II | Suture-button fixation 23 patients; screw fixation 23 patients | 2.5 years; range 1.5–3.5 | AOFAS score; FADI score; syndesmotic width; MCS; TFO; TFCS; revision; complications | Syndesmotic width was significantly smaller in suture-button (P = 0.01); No difference in AOFAS and FADI score; significantly more malreduction in screw fixation (P = 0.04) | Suture-button devices was not only a feasible method of syndesmotic fixation, but also be slight better than traditional screw |
| Coetzee and Ebeling [32] | RCT | Level I | Suture-button fixation 12 patients; screw fixation 12 patients | Mean 18 months | Subjective results; ankle ROM; AOFAS score; complications | No significant difference in AOFAS score; ankle ROM and subjective stiffness was significantly better in suture-button | Suture-button device lead to better objective ankle motion as well as decreased stiffness and discomfort since it stabilize syndesmosis without eliminating normal motion |
| Pakarinen et al. [33] | RCT | Level I | None fixation 11 patients; syndesmotic screw fixation 13 patients | Mean 61 weeks; range 53–112 | Ankle range of motion; OMS score; VAS score; RAND 36-item health survey; TFCS; | No significant difference in OMS score (P = 0.5); VAS score (P = 0.38) and RAND 36 scores (P = 0.23) | Syndesmotic injuries are rare in SER ankle fractures; syndesmotic fixation did not influence the results at one-year follow-up compared with no fixation |
| Kennedy et al. [34] | Prospective comparative study | Level II | None fixation 19 patients; tricortical syndesmotic screw fixation 26 patients | 2.9 years; range 2.8–4.2 | Subjective outcomes; ankle ROM; functional score; complications | No significant difference in subjective outcomes (P = 0.86); ankle motion (P = 0.94); fracture dislocation was a predictor for poor results | Fixed or non-fixed syndesmosis had similar results in low Weber C ankle fracture |
TFCS tibiofibular clear space, TFO tibiofibular overlap, MCS medial clear space, OMS Olerud–Molander score, AOFAS American Orthopedic Foot & Ankle Society scoring system, VAS visual analogue scale
Four separate comparisons about distal syndesmotic fixation were covered in these eligible studies: (1) clinical outcomes of absorbable implants versus traditional screws, (2) clinical outcomes of tricortical screw fixation versus more widely used one quadricortical screw fixation, (3) the newly emerged suture-button technique versus screw placement, (4) whether it was necessary to fix the low syndesmotic injury (to be less than 5 cm from the proximal ankle joint surface) in cases of Weber B and low Weber C fracture.
Eight of the included studies were randomized controlled trials while the other four were prospective comparative studies. One RCT was written in Chinese and was translated into English so that it can be provided when necessary. Six of them were classified as level I clinical evidence with the concealed randomized allocation method and low lost to follow-up rate. The other two were quasi-randomization trials. Only two RCTs and one prospective comparative study had an examiner who was blinded to the group allocation. The data analysis results of all extracted data are shown in Tables 2, 3, 4 and 5.
Table 2.
Data analysis of absorbable screw versus metallic screw
| Outcome measurement | Studies | Patients | Statistical method | Effect size | P value |
|---|---|---|---|---|---|
| 01. Unable to return to sports | 1 | 38 | Odds ratio M-H, fixed, 95 % CI | 0.35 [0.07,1.7] | 0.19 |
| 02. Ankle dorsiflexion | 2 | 85 | Mean difference IV, fixed, 95 % CI | −0.21 [−2.65.2.23] | 0.87 |
| 03. Ankle plantarflexion | 2 | 85 | Mean difference IV, fixed, 95 % CI | 1.87 [−0.66,4.4] | 0.15 |
| 04. TFCS | 2 | 77 | Mean difference IV, fixed, 95 % CI | −0.04 [−0.34, 0.25] | 0.78 |
| 05. TFO | 2 | 77 | Mean difference IV, fixed, 95 % CI | −0.28 [−0.69, 0.13] | 0.47 |
| 06. Complication | 4 | 147 | Odds ratio M-H, fixed, 95 % CI | 1.23 [0.29, 5.17] | 0.53 |
| 07. Subjective satisfaction | 2 | 70 | Only reported no difference between two groups |
CI confidence interval, TFCS tibiofibular clear space, TFO tibiofibular overlap
Table 3.
Data analysis of tricortical fixation versus quadricortical fixation
| Outcome measurement | Studies | Patients | Statistical method | Effect size | P value |
|---|---|---|---|---|---|
| 01. OMS score at three months | 1 | 64 | Mean difference IV, fixed, 95 % CI | −10.70 [−19.7, −1.7] | 0.02* |
| 02. OMS score at one year | 1 | 64 | Mean difference IV, fixed, 95 % CI | −5.5 [−13.77, 2.77] | 0.19 |
| 03. OMS score at eight years | 1 | 48 | Mean difference IV, fixed, 95 % CI | 0.5 [−10.63, 11.63] | 0.93 |
| 04. Radiologic problems at one year | 1 | 64 | Odds ratio M-H, fixed, 95 % CI | 0.34 [0.1, 1.16] | 0.09 |
| 05. Radiologic problems at eight years | 1 | 48 | Odds ratio M-H, fixed, 95 % CI | 1.05 [0.32, 3.45] | 0.93 |
| 06. Ankle dorsiflexion at one year | 1 | 64 | Mean difference IV, fixed, 95 % CI | 1.7 [−1.94, 5.34] | 0.36 |
| 07. Ankle dorsiflexion at eight years | 1 | 48 | Mean difference IV, fixed, 95 % CI | 7.6 [0.42, 14.78] | 0.04* |
| 08. Complications within one year | 2 | 184 | Odds ratio M-H, fixed, 95 % CI | 1.16 [0.56, 2.41] | 0.68 |
| 09. Complications at eight years | 1 | 48 | Odds ratio M-H, fixed, 95 % CI | 0.68 [0.21, 2.18] | 0.51 |
CI confidence interval, OMS Olerud–Molander score
* Indicates statistical significance
Table 4.
Data analysis of suture-button fixation versus screw fixation
| Outcome measurement | Studies | Patients | Statistical method | Effect size | P value |
|---|---|---|---|---|---|
| 01. AOFAS score | 3 | 120 | Mean difference IV, fixed, 95 % CI | −4.28 [−7.15, −1.41] | 0.003* |
| 02. Time to full weightbearing | 2 | 96 | Mean difference IV, fixed, 95 % CI | −3.17 [−3.78, −2.56] | P < 0.0001* |
| 03. Ankle dorsiflexion | 1 | 24 | Mean difference IV, fixed, 95 % CI | −3.4 [−6.41, 0.41] | 0.08 |
| 04. Ankle plantarflexion | 1 | 24 | Mean difference IV, fixed, 95 % CI | −10.0 [−18.6, −1.4] | 0.02* |
| 05. MCS | 2 | 96 | Mean difference IV, fixed, 95 % CI | −0.01 [−0.19, 0.17] | 0.89 |
| 06. TFO | 2 | 96 | Mean difference IV, fixed, 95 % CI | 0.33 [−0.42, 1.07] | 0.39 |
| 07. TFCS | 2 | 96 | Mean difference IV, fixed, 95 % CI | −0.96 [−1.34, −0.58] | P < 0.0001* |
| 08. Complications | 3 | 120 | Odds ratio M-H, fixed, 95 % CI | 0.12 [0.03, 0.41] | 0.0008* |
CI confidence interval, TFCS tibiofibular clear space, TFO tibiofibular overlap, MCS medial clear space, AOFAS American Orthopedic Foot & Ankle Society scoring system
* Indicates statistical significance
Table 5.
Data analysis for comparison of fix or not in low syndesmotic injuries
| Outcome measurement | Studies | Patients | Statistical method | Effect size | P value |
|---|---|---|---|---|---|
| 01. Ankle dorsiflexion | 1 | 24 | Mean difference IV, fixed, 95 % CI | −1.0 [−8.01, 6.01] | 0.78 |
| 02. Ankle plantarflexion | 1 | 24 | Mean difference IV, fixed, 95 % CI | 5 [−1.25, 11.25] | 0.12 |
| 03. OMS score | 1 | 24 | Mean difference IV, fixed, 95 % CI | −4.0 [−54.12, 46.12] | 0.88 |
| 04. VAS score | 1 | 24 | Mean difference IV, fixed, 95 % CI | −14.2 [−29.91, 1.51] | 0.08 |
| 05. Complication | 1 | 45 | Odds ratio M-H, fixed, 95 % CI | 0.25 [0.01, 5.54] | 0.38 |
CI confidence interval, OMS Olerud–Molander score, VAS visual analogue scale
Absorbable implants or metallic screws
Four studies were concerned with comparison of absorbable and metallic screws. Two of them were randomized controlled trials; the others were a quasi-randomized trial and a prospective study. Overall 147 patients with syndesmotic injuries were included and 77 received absorbable screw fixation. All syndesmotic injuries were diagnosed radiographically before surgery and further confirmed by hook test intraoperatively. PLLA (polylevolactic acid) screw was employed in three studies while the other used PDLLA (poly-DL-lactic acid) screw. Average follow-up duration was 13.36 ± 2.63 months.
All metallic screws were routinely removed six to eight weeks after primary operation while only two symptomatic patients (2.6 %) needed removal in the absorbable screw group. No significant difference was found in terms of subjective satisfaction, return to previous sports (p = 0.19) and ankle range of motion (dorsiflexion p = 0.87; plantarflexion p = 0.15). Complications occurred in four patients of the absorbable group (5.2 %) consisting of one deep infection, one moderate foreign body reaction and two palpable remnants. There were three wound infections in the metallic screw group (4.3 %) and two of them happened after routine implant removal. No significant difference was found with regard to complication incidence (p = 0.53).
Tricortical versus quadricortical fixation
Two RCTs and one quasi-randomized study were included for comparison of tricortical and quadricortical fixation. In total 232 patients with syndesmotic instability (diagnosed with hook tests during operations) were enrolled and 118 of them received 3.5-mm tricortical screw fixation. One study displayed long-term results with a mean follow-up time of 8.4 years. The other two reported short-term results (150 days and one year).
Tricortical fixation had significantly better OMS score (Olerud–Molander score) at three months after surgery (p = 0.02); while in long-term follow-up, a significant difference was detected in ankle dorsiflexion favouring quadricortical fixation (p = 0.04). The short-term complication rate in both groups was 20.1 % with problems of malreduction, loss of reduction, screw failure and wound infections. In long-term follow-up results, 25 % of patients developed ankle arthritis (five in tricortical and seven in quadricortical). No significant difference was found between the two fixation methods for both long-term (p = 0.68) and short-term (p = 0.51) complication rate. Moreover, the short-term (p = 0.09) and long-term (p = 0.93) radiographic evaluation had no significant differences either.
Suture-button fixation versus syndesmotic screw
Two prospective comparative studies and one RCT with a total of 120 patients (60 suture-button fixations, 60 syndesmotic screws) were included. Mean follow-up duration was 19.1 ± 14.5 months. Compared with conventional screw, the suture-button showed significantly higher AOFAS score (American Orthopedic Foot & Ankle Society scoring system) (p = 0.003), better ankle plantar flexion (p = 0.02) and shorter time to full weightbearing (p < 0.0001) according to the short- and medium-term results. For the radiographic evaluation, TFCS (tibiofibular clear space) was significantly smaller in the suture-button group (p < 0.0001), but no difference in the MCS (medical clear space) (p = 0.89) and TFO (tibiofibular overlap) (p = 0.39).
Only two suture-button devices needed secondary removal whilst 30 % of the screw implantations were routinely removed and 25 % needed to be removed due to various symptoms. The complications rates were 35.4 % in screw fixation and mainly consisted of hardware failure, loosening and malreduction. Complications happened in 3 % of suture-button fixation and significantly lower than with the metallic screw (p = 0.0008).
Fix or not for low syndesmotic injuries
One RCT involved SER (supination-external rotation) IV ankle fractures and one prospective comparative study of low weber C fractures was enrolled. Sixty-nine patients were included with low syndesmotic injuries to be less than 5 cm from the proximal ankle joint surface and clear diagnosis of instability through hook test or external rotation stress test intraoperatively. Thirty patients received syndesmotic transfixation with 3.5-mm metallic screws while the others had no fixation. There was no significant difference between the two groups with respect to range of motion (p = 0.78), VAS score (visual analogue scale) (p = 0.08), OMS score (p = 0.88) and complication rates (p = 0.38). However, all outcome measurements were relatively poorer in screw fixed patients and almost reached the significance level in VAS score and ankle range of motion.
Discussion
Syndesmotic injuries were commonly encountered clinical conditions since they occurred in isolation or associated with fibular fractures [35, 36]. Recently, many controversies have emerged in various aspects of syndesmotic fixation [19]. However, no systematic review has been reported to analyse the high level clinical evidence in this field. The present study summed up high-quality studies after strict screening in order to find more reliable outcomes.
Besides being few in number, randomized trials reporting on the syndesmotic fixation were generally of relatively poor quality. The most prominent flaws were inadequate subjective number, lack of blindness and high heterogeneity of outcome measurements. It had been estimated that a sample size of nearly 200 would be adequate to detect a significant difference of ankle range of motion between the two groups [33]. Furthermore, a study population of 60 only found a 20 % difference of Olerud–Molander ankle scores [33]. The functional scores, radiological evaluation and ankle range of motion were presented in a diversity of patterns and these variations would reduce the validity of our data analysis.
Nonetheless, despite the above limitations, the subject enrolled criteria and the diagnosis of syndesmotic instability were quite comparable among these studies. The group characteristics in each study were also well controlled.
Syndesmotic fixation was supposed to be necessary in cases of syndesmotic instability [37, 38]. Currently, trans-syndesmotic screw is still the predominant treatment [39]. However, the distal fibula had 1- to 2-mm lateral translation and 2° external rotation during ankle dorsiflexion in normal gait [40]. Implantation of the screw nearly eliminated all these normal syndesmotic motions [41]. Most surgeons routinely performed a second operation for screw removal [42, 43]. Thus, new materials, techniques and devices had appeared for better preservation of physiologic motion and, at the same time, avoid the secondary removal.
The absorbable syndesmotic screw was introduced in order to revolve secondary hardware removal of traditional metallic screw [44]. The current review found that only 2.6 % of the absorbable implanted patients needed a second operation. But unfortunately, this data could not strongly illustrate a reduced removal rate since all metallic screws were routinely removed. Additionally, absorbable screws showed no superior results in other evaluation aspects.
On the other side, absorbable screws had long been questioned about the biomechanical strength and foreign body reaction [24]. Our data analysis demonstrated that there is no loss of reduction, and this was consistent with the biomechanical study which concluded that the PLA screw had enough strength to resist postoperative forces when distal tibiofibular syndesmosis occurred. In recent years, PLLA material has been proven to be much more biocompatible than older PGA (polyglycolide) [45], and only one moderate foreign body reaction occurred in the absorbable group. Therefore, we felt that the main issue of absorbable syndesmotic screw had to switch from its biomechanical strength or foreign body reaction to its true benefits brought to the patients.
Tricortical screw fixation has been reported to have less biomechanical impact on normal syndesmotic motion [27] and would be a method to obviate second removal. The present review revealed 43 % fewer operations for implant removal in the tricortical group. However, this result was also not fully reliable since 52 % of the quadricoritcal patients received routine removal as initial protocol. The tricortical fixation group had better functional results at three months after surgery. Hoiness and Stromsoe [29] believed that this would be related to its advantage of relative dynamic syndesmotic fixation. However, there was no such difference at one-year followup. This may be due to reduced immobilization effect of quadricortical screw over time, and motion between distal tibia and fibula was gradually permitted [27]. In contrast, the tricortical fixation proved to be inferior in ankle range of motion in long-term results.
Moore et al. [28] reported that three cortical fixation was associated with more loss of reduction occurrence and contributed to its inadequate fixation strength. However our data analysis found neither significant difference of loss of reduction nor total complication incidence between the two methods. But there was still inadequate biomechanical evidence to stand for the efficiency of tricortical fixation.
The suture-button technique is relatively new and it provides dynamic fixation of the distal syndesmosis [16, 46]. The physiologic micromotion could be more preserved than traditional rigid fixation. Our results supported this viewpoint since we found significantly better functional recovery and ankle joint motion in the suture-button group with much fewer complications. Meanwhile, the TFCS and time to full weightbearing were also significantly better than syndesmotic screws. Theoretically, routine removal of suture-button was not necessary. But recent literature has reported about local soft tissue irritation of suture-button, and Naqvi et al. [46] had recommended hardware removal. The present review only found one local irritation and one superficial infection in 60 patients. Avoidance of an additional operation would compensate for the excessive cost of suture-button implant but the accurate cost-efficiency outcomes need specific studies.
The better results of the suture-button technique in short- and intermediate-term followup has made it a promising way for syndesmotic injury treatment. But undeniably, the current studies in this field are of relative low quality and the exact performance of suture-button fixation in the long term also needs further reports.
Boden’s classical biomechanical study [47] suggested that syndesmotic screw should only be applied when syndesmotic injury was 3–4.5 cm higher than the proximal tibiotalar articular surface combined with deltoid ligament disruption. This conclusion has been further testified by other researchers [48, 49] and has been accepted by many surgeons in their clinical practice. However, trans-syndesmotic fixation was also considered when the external rotation stress test or hook test showed instability.
Our analysis demonstrated there is no significant difference for syndesmotic screw implantation in low syndesmotic injuries. This would partly contribute to the recent biomechanical finding that medial structure was the primary factor of ankle stability [50, 51]. On the other side, although all these patients were clearly diagnosed as syndesmotic instability though intra-operative external rotation stress test, we surprisingly found that all outcome measurements were relatively poorer for the fixed group. Such findings prompted that unnecessary screw placement would not only impose additional problems such as secondary operation and increasing cost, but also would bring reserve effects on final recovery. The relatively inferior outcomes could strongly relate to the disappearing of normal syndesmotic micro-movement after fixation. The current evidence demonstrated no benefit for screw fixation in low syndesmotic injured patients. Therefore, carefully evaluation should be conducted before fixation determination in such cases and, more importantly, the indication of syndesmotic screw should be further researched and defined.
Conclusion
There were still many uncertainties about syndesmotic fixation. Bioabsorbable screw and tricortical fixation method seldom showed better results than the traditional one four cortical screw fixation. At present, no reliable data supported their efficiency in hardware removal rate reduction. The suture-button device is a flexible fixation method and seems to be promising. It had led to better functional outcomes and lower complication rates in short- and intermediate-term followup, but still premature due to lack of long-term results and cost-efficiency studies. The screw fixation in low syndesmotic injury showed marginally poorer results. More high-quality RCTs are required to further explicit the indication of syndemostic screw placement in such conditions.
Acknowledgments
This research was funded by the national natural science foundation of china (Grant No.81171670).
References
- 1.Dattani R, Patnaik S, Kantak A, Srikanth B, Selvan TP. Injuries to the tibiofibular syndesmosis. J Bone Joint Surg Br. 2008;90:405–410. doi: 10.1302/0301-620X.90B4.19750. [DOI] [PubMed] [Google Scholar]
- 2.Stein G, Eichler C, Ettmann L, Koebke J, Müller LP, Thelen U, Skouras E. Tibiofibular screw fixation for syndesmotic ruptures: a biomechanical analysis. Surg Radiol Anat. 2012;34:593–597. doi: 10.1007/s00276-012-0956-5. [DOI] [PubMed] [Google Scholar]
- 3.Park JC, McLaurin TM. Acute syndesmosis injuries associated with ankle fractures: current perspectives in management. Bull Nyu Hosp Jt Dis. 2009;67:39–44. [PubMed] [Google Scholar]
- 4.Dubin JC, Comeau D, McClelland RI. Lateral and syndesmotic ankle sprain injuries: a narrative literature review. J Chiropr Med. 2011;10:204–219. doi: 10.1016/j.jcm.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bekerom MP. Diagnosing syndesmotic instability in ankle fractures. World J Orthop. 2011;2(7):51–56. doi: 10.5312/wjo.v2.i7.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Monga P, Kumar A, Simons A, Panikker V. Management of distal tibio-fibular syndesmotic injuries: a snapshot of current practice. Acta Orthop Belg. 2008;74:365–369. [PubMed] [Google Scholar]
- 7.Pakarinen H, Flinkkilä T, Ohtonen P, Hyvönen P, Lakovaara M, Leppilahti J, Ristiniemi J. Intraoperative assessment of the stability of the distal tibiofibular joint in supination-external rotation injuries of the ankle: sensitivity, specificity, and reliability of two clinical tests. J Bone Joint Surg Am. 2011;93:2057–2061. doi: 10.2106/JBJS.J.01287. [DOI] [PubMed] [Google Scholar]
- 8.Jones MH, Amendola A. Syndesmosis sprains of the ankle. Clin Orthop Relat Res. 2007;455:173–175. doi: 10.1097/BLO.0b013e31802eb471. [DOI] [PubMed] [Google Scholar]
- 9.Ramsey PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg. 1976;58:356–357. [PubMed] [Google Scholar]
- 10.Jordan TH, Talarico RH, Schuberth JM. The radiographic fate of the syndesmosis after trans-syndesmotic screw removal in displaced ankle fractures. J Foot Ankle Sur. 2011;50:407–412. doi: 10.1053/j.jfas.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 11.Schepers T, Van Lieshout EMM, De Vries MR. Complications of syndesmotic screw removal. Foot Ankle Int. 2011;32:1040–1044. doi: 10.3113/FAI.2011.1040. [DOI] [PubMed] [Google Scholar]
- 12.Manzotti A, Baiguini P, Tecchio P. The use of a Kirshner wire in the stabilization of tibial-fibular syndesmosis in type-C ankle fractures according to Weber. Minerva Ortopedica Traumatologica. 1997;48(11):425–428. [Google Scholar]
- 13.ElRayes M, Hammoda A. Screw versus staple in stabilization of diastasis of tibiofibular syndesmosis. J Foot Ankle Surg. 2007;13:5–9. doi: 10.1016/j.fas.2006.06.005. [DOI] [Google Scholar]
- 14.De Vil J, Bonte F. Bolt fixation for syndesmotic injuries. Injury. 2009;40:1176–1179. doi: 10.1016/j.injury.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 15.Joukainen A, Partio EK, Waris P, Joukainen J, Kröger H, Törmälä P, Rokkanen P. Bioabsorbable screw fixation for the treatment of ankle fractures. J Orthop Sci. 2007;12(1):28–34. doi: 10.1007/s00776-006-1077-y. [DOI] [PubMed] [Google Scholar]
- 16.Thornes B, Shannon F, Guiney AM. Suture-button syndesmosis fixation: accelerated rehabilitation and improved outcomes. Clin Orthop Relat Res. 2005;431:207–212. doi: 10.1097/01.blo.0000151845.75230.a0. [DOI] [PubMed] [Google Scholar]
- 17.Stuart K, Panchbhavi VK. The fate of syndesmotic screws. Foot Ankle Int. 2011;32:519–525. doi: 10.3113/FAI.2011.0519. [DOI] [PubMed] [Google Scholar]
- 18.Huber T, Schmoelz W, Bolderl A. Motion of the fibula relative to the tibia and its alterations with syndesmosis screws: a cadaver study. Foot Ankle Surg. 2012;18(3):203–209. doi: 10.1016/j.fas.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 19.Bekerom MP, Hogervorst M, Bolhuis HW. Operative aspects of the syndesmotic screw: review of current concepts. Injury. 2008;39:491–498. doi: 10.1016/j.injury.2007.11.425. [DOI] [PubMed] [Google Scholar]
- 20.Schepers T. Acute distal tibiofibular syndesmosis injury: a systematic review of suture-button versus syndesmotic screw repair. Int Orthop. 2012;36:1199–1206. doi: 10.1007/s00264-012-1500-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schepers T. To retain or remove the syndesmotic screw: a review of literature. Arch Orthop Trauma Surg. 2011;131:879–883. doi: 10.1007/s00402-010-1225-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Daas A, Zuuren WJ, Pelet S, Noort A, Bekerom MPJ. Flexible stabilization of the distal tibiofibular syndesmosis: clinical and biomechanical considerations: a review of the literature. Strateg Trauma Limb Reconstr. 2012;7:123–129. doi: 10.1007/s11751-012-0147-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thordarson DB, Samuelson M, Shepherd LE, et al. Bioabsorbable versus stainless steel screw fixation of the syndesmosis in pronation-lateral rotation ankle fractures a prospective randomized trial. Foot Ankle Int. 2001;22(4):335–338. doi: 10.1177/107110070102200411. [DOI] [PubMed] [Google Scholar]
- 24.Kaukonen JP, Lamberg T, Korkala O, Pajarinen J. Fixation of syndesmotic ruptures in 38 patients with a malleolar fracture- a randomized study comparing a metallic and a bioabsorbable screw. J Orthop Trauma. 2005;19(6):392–396. doi: 10.1097/01.bot.0000155313.50627.f6. [DOI] [PubMed] [Google Scholar]
- 25.Hu YL, Yuan WQ, Wang LF, Liu HF, Jin D. A prospective randomized trial of poly-DL-lactic acid absorbable and metallic screws for treatment of syndesmotic disruptions. Nan Fang Yi Ke Da Xue Xue Bao. 2010;30:2360–2362. [PubMed] [Google Scholar]
- 26.Sinisaari IP, Lüthje PM, Mikkonen RH. Ruptured tibio-fibular syndesmosis: comparison study of metallic to bioabsorbable fixation. Foot Ankle Int. 2002;23(8):744–748. doi: 10.1177/107110070202300811. [DOI] [PubMed] [Google Scholar]
- 27.Wikerøy AK, Høiness PR, Andreassen GS. No difference in functional and radiographic results 8.4 years after quadricortical compared with tricortical syndesmosis fixation in ankle fractures. J Orthop Trauma. 2010;24(1):17–23. doi: 10.1097/BOT.0b013e3181bedca1. [DOI] [PubMed] [Google Scholar]
- 28.Moore JA, Jr, Shank JR, Morgan SJ. Syndesmosis fixation: a comparison of three and four cortices of screw fixation without hardware removal. Foot Ankle Int. 2006;27(8):567–572. doi: 10.1177/107110070602700801. [DOI] [PubMed] [Google Scholar]
- 29.Høiness P, Strømsøe K. Tricortical versus quadricortical syndesmosis fixation in ankle fractures: a prospective, randomized study comparing two methods of syndesmosis fixation. J Orthop Trauma. 2004;18(6):331–337. doi: 10.1097/00005131-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 30.Cottom JM, Hyer CF, Philbin TM, Berlet GC. Transosseous fixation of the distal tibiofibular syndesmosis: comparison of an interosseous suture and endobutton to traditional screw fixation in 50 cases. J Foot Ankle Int. 2009;48(6):620–630. doi: 10.1053/j.jfas.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 31.Naqvi GA, Cunningham P, Lynch B, Galvin R, Awan N. Fixation of ankle syndesmotic injuries: comparison of TightRope fixation and syndesmotic screw fixation for accuracy of syndesmotic reduction. Am J Sports Med. 2012;40(12):2828–2835. doi: 10.1177/0363546512461480. [DOI] [PubMed] [Google Scholar]
- 32.Coetzee JC, Ebeling P. Treatment of syndesmoses disruptions: a prospective, randomized study comparing conventional screw fixation vs TightRope fiber wire fixation—medium term results. South Afr Orthop J. 2009;8(1):32–37. [Google Scholar]
- 33.Pakarinen HJ, Flinkkilä TE, Ohtonen PP. Syndesmotic fixation in supination-external rotation ankle fractures: a prospective randomized study. Foot Ankle Int. 2011;32:1103–1109. doi: 10.3113/FAI.2011.1103. [DOI] [PubMed] [Google Scholar]
- 34.Kennedy JG, Soffe KE, Dalla Vedova P, Stephens MM, O’Brien T, Walsh MG, McManus F. Evaluation of the syndesmotic screw in low Weber C ankle fractures. J Orthop Trauma. 2000;14(5):359–366. doi: 10.1097/00005131-200006000-00010. [DOI] [PubMed] [Google Scholar]
- 35.Valkering KP, Vergroesen DA, Nolte PA. Isolated syndesmosis ankle injury. Orthopedics. 2012;35(12):e1705–e1710. doi: 10.3928/01477447-20121120-13. [DOI] [PubMed] [Google Scholar]
- 36.Pakarinen H. Stability-based classification for ankle fracture management and the syndesmosis injury in ankle fractures due to a supination external rotation mechanism of injury. Acta Orthop Suppl. 2012;83(347):1–26. doi: 10.3109/17453674.2012.745657. [DOI] [PubMed] [Google Scholar]
- 37.Ebraheim NA, Elgafy H, Padanilam T (2003) Syndesmotic disruption in lowfibular fractures associated with deltoid ligament injury. Clin Orthop Relat Res 409:260–267 [DOI] [PubMed]
- 38.Schepers T, van Zuuren WJ, van den Bekerom MP. The management of acute distal tibio-fibular syndesmotic injuries: results of a nationwide survey. Injury. 2012;43(10):1718–1723. doi: 10.1016/j.injury.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 39.Stein G, Eichler C, Ettmann L, Koebke J, Müller LP, Thelen U, Skouras E. Tibiofibular screw fixation for syndesmotic ruptures: a biomechanical analysis. Surg Radiol Anat. 2012;34(7):593–597. doi: 10.1007/s00276-012-0956-5. [DOI] [PubMed] [Google Scholar]
- 40.Sasse M, Nigg BM, Stefanyshyn DJ. Tibiotalar motion—effect of fibular displacement and deltoid ligament transection: in vitro study. Foot Ankle Int. 1999;20(11):733–737. doi: 10.1177/107110079902001110. [DOI] [PubMed] [Google Scholar]
- 41.Olerud C. The effects of the syndesmotic screw on the extension capacity of the ankle joint. Arch Orthop Trauma Surg. 1985;104:299–304. doi: 10.1007/BF00435946. [DOI] [PubMed] [Google Scholar]
- 42.Miller AN, Paul O, Boraiah S, Parker RJ, Helfet DL, Lorich DG. Functional outcomes after syndesmotic screw fixation and removal. J Orthop Trauma. 2010;24:12–16. doi: 10.1097/BOT.0b013e3181c6e199. [DOI] [PubMed] [Google Scholar]
- 43.Hsu YT, Wu CC, Lee WC, Fan KF, Tseng IC, Lee PC. Surgical treatment of syndesmotic diastasis: emphasis on effect of syndesmotic screw on ankle function. Int Orthop. 2011;35:359–364. doi: 10.1007/s00264-010-1147-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ahmad J, Raikin SM, Pour AE, Haytmanek C. Bioabsorbable screw fixation of the syndesmosis in unstable ankle injuries. Foot Ankle Int. 2009;30(2):99–105. doi: 10.3113/FAI.2009.0099. [DOI] [PubMed] [Google Scholar]
- 45.Hovis WD, Kaiser BW, Watson JT, Bucholz RW. Treatment of syndesmotic disruptions of the ankle with bioabsorbable screw fixation. J Bone Joint Surg Am. 2002;84:26–31. doi: 10.2106/00004623-200201000-00005. [DOI] [PubMed] [Google Scholar]
- 46.Naqvi GA, Shafqat A, Awan N. Tightrope fixation of ankle syndesmosis injuries: clinical outcome, complications and technique modification. Injury. 2012;43:838–842. doi: 10.1016/j.injury.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 47.Boden SD, Labropoulos PA, McCowin P. Mechanical considerations for the syndesmosis screw—a cadaver study. J Bone Joint Surg Am. 1989;71:1548–1555. [PubMed] [Google Scholar]
- 48.Bekerom MP, Haverkamp D, Kerkhoffs GM. Syndesmotic stabilization in pronation external rotation ankle fractures. Clin Orthop Relat Res. 2010;468:991–995. doi: 10.1007/s11999-009-0823-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Park JC, McLaurin TM. Acute syndesmosis injuries associated with ankle fractures: current perspectives in management. Bull NYU Hosp Jt Dis. 2009;67(1):39–44. [PubMed] [Google Scholar]
- 50.Schuberth JM, Collman DR, Rush SM, Ford LA. Deltoid ligament integrity in lateral malleolar fractures: a comparative analysis of arthroscopic and radiographic assessments. J Foot Ankle Surg. 2004;43(1):20–29. doi: 10.1053/j.jfas.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 51.Michelson JD, Waldman B. An axially loaded model of the ankle after pronation external rotation injury. Clin Orthop. 1996;328:285–293. doi: 10.1097/00003086-199607000-00043. [DOI] [PubMed] [Google Scholar]