Abstract
Purpose
The purpose of this study was to evaluate the radiographic characteristics and structural configurations of a series of patients with a primary degenerative arthritis of the second metatarsophalangeal joint.
Methods
We studied 37 feet that had undergone surgical treatment for primary degenerative arthritis of the second metatarsophalangeal joint. The patients were compared with a randomly selected control group, without arthritis of the second metatarsophalangeal joint. The first, second, and fourth metatarsal lengths, and the size of the second metatarsal head were measured on weight-bearing anteroposterior radiographs. The patients were classified on the basis of joint-space narrowing, subchondral sclerosis, osteophyte formation, and subchondral cystic change.
Results
The average second metatarsal length was significantly longer in the study group (P = 0.01). The average length of the first metatarsal relative to the fourth metatarsal was significantly shorter (P = 0.02) in the study group, while the average length of the second metatarsal relative to the fourth metatarsal was significantly longer (P = 0.01) in the study group. The average diameter of the second metatarsal head was significantly larger in the study group (P = 0.00), and the average ratio of this diameter relative to the length of the fourth metatarsal was significantly higher in the study group (P = 0.00). A total of four feet were classified as grade 0, nine as grade 1, 17 as grade 2, and seven as grade 3.
Conclusions
Second toe rigidus should be considered as a diagnosis in patients with painful limited dorsiflexion of the second metatarsophalangeal joint without evidence of Freiberg’s infraction or trauma.
Introduction
Degenerative arthritis of the joints of the foot and ankle typically occurs in middle-aged and older patients, but can occur in younger individuals after osteochondral injuries or trauma. Hallux rigidus describes a painful condition affecting the metatarsophalangeal joint of the great toe, characterised by restricted motion (mainly dorsiflexion) and proliferative periarticular bone formation. While there are numerous studies on hallux rigidus [1], second metatarsophalangeal joint arthritis is rarely mentioned in studies on second metatarsophalangeal joint instability [2], Freiberg’s infraction [3], or trauma. Moreover, we could not find any studies in the literature on primary degenerative arthritis of this joint.
Freiberg’s infraction of the second metatarsophalangeal joint results in widening of the joint space, and flattening and central collapse of the metatarsal head [4–6]. However, we have experienced many cases of degenerative osteoarthritis without any radiographic or intraoperative or histopathological evidence of avascular necrosis of the second metatarsal head. These cases did demonstrate degenerative spurs along the margin of the metatarsal head and base of the proximal phalanx, and cartilage denudation on the dorsal aspect of the metatarsal head (Fig. 1). The main problem with this condition is the limited dorsiflexion from abutment of the base of the proximal phalanx to the metatarsal head, in contrast with the second metatarsophalangeal joint instability.
Fig. 1.

Intraoperative picture, showing degenerative spurs along the margin of the metatarsal head and base of the proximal phalanx, as well as cartilage denudation on the dorsal aspect of the metatarsal head
The aim of our study was to evaluate the radiographic characteristics and structural configurations of a series of patients with a primary degenerative arthritis of the second metatarsophalangeal joint we termed “second toe rigidus.” We propose a new radiographic classification system for these lesions.
Materials and methods
We retrospectively reviewed consecutive debridements and cheilectomies of the second metatarsophalangeal joint in patients with symptomatic arthritic condition of that joint performed by a single surgeon (WCL) between 2002 and 2011. We excluded patients with evidence of Freiberg’s disease or a history of inflammatory arthritis, trauma, or Charcot arthropathy. Evidence of Freiberg’s disease was determined by radiographic or intraoperative findings as widening of the joint space, and flattening or central collapse of the metatarsal head and histopathological finding as avascular necrosis of the second metatarsal head. A total of 33 patients (37 feet), including six men and 27 women, with an average age of 57.1 years (range, 29–78 years) were included in the study. Clinically, all patients in the study group reported limited motion of the second metatarsophalangeal joint, particularly dorsiflexion (Fig. 2), and pain isolated to this joint that was refractory to shoe modification, nonsteroidal anti-inflammatory medication, or modification of activities. All patients were confirmed to have degenerative osteoarthritis without any evidence of avascular necrosis of the second metatarsal head based on preoperative radiographs, intraoperative findings and postoperative histopathological findings. The average hallux valgus and first–second intermetatarsal angles of the participants were 29.4° and 14.0° (ranges, 6°–47° and 7°–24°), respectively.
Fig. 2.

Physical examination of a patient with second toe rigidus, revealing limited motion of the second metatarsophalangeal joint, especially with regard to dorsiflexion
We also evaluated a control group of 34 patients (50 feet), consisting of two men and 32 women, with an average age of 53.7 years (range, 24–75 years). All control subjects were selected from another study, and were similar to the study group subjects in terms of age, hallux valgus angle, and first–second intermetatarsal angle, and had no arthritis of the second metatarsophalangeal joint. The same exclusion criteria were applied for the control group. The average hallux valgus and first–second intermetatarsal angles in the control group were 31.2° and 15.1° (range, 20°–43° and 10°–20°), respectively.
All subjects, both study and control, underwent weight-bearing anteroposterior and lateral radiographs of the feet at one location and with the same equipment. Measurements were made using an electronic method created by the junior author (JHC). To assess the reliability of the radiographic measurements used in the study, an intraobserver measurement reliability study was conducted. First, second, and fourth metatarsal lengths were measured on anteroposterior radiographs, as described in Fig. 3. To identify whether the second metatarsal was long or the first metatarsal was short, we obtained the ratios of the first and second metatarsal lengths relative to the fourth metatarsal length. The fourth metatarsal also was chosen in a study by Davitt et al. [7], because it is easily measured and can serve as an internal control. The degree of metatarsus adductus also was measured. The technique used for measurement relates the position of the metatarsals relative to the midfoot; a normal value is 15° or more, mild adductus is 16°–19°, moderate is 20°–25°, and severe is >25° [8].
Fig. 3.
Anteroposterior radiograph of a foot. The length of the first metatarsal was measured from A to B, and the length of the second metatarsal was measured from C to D. The width of the bone of each metatarsal was measured at the junction of the diaphysis and metaphysis. A point midway along the width was identified, and a line was drawn connecting these points. The point at which this line intersected the most proximal and most distal aspects of the bone represented the length of the bone. AB was the length of the first metatarsal, and CD was the length of the second metatarsal. The fourth metatarsal was measured in the same way
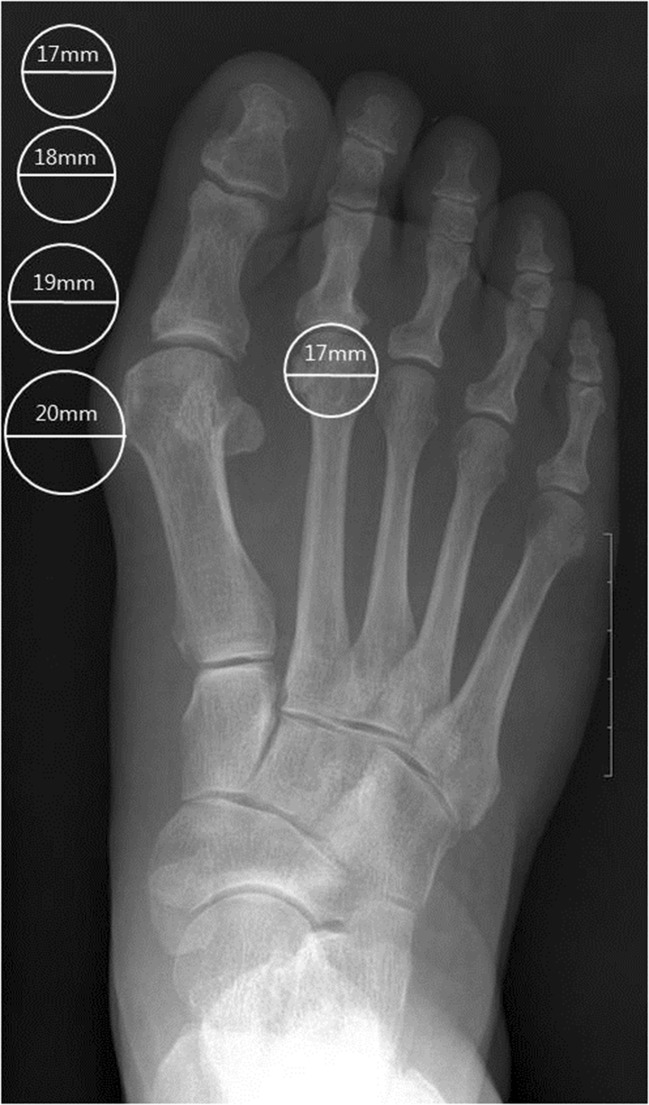
The size of the second metatarsal head was assessed by using a new method based on the anteroposterior radiographs. We placed the second metatarsal head overlay templates on the radiograph, and selected the size that most precisely matched the contour of the second metatarsal head with adequate lateral coverage (Fig. 4). We also compared the diameter of the second metatarsal head with the length of the fourth metatarsal.
Fig. 4.
Anteroposterior radiograph of a foot. The size of the second metatarsal head was measured by using the following method: We placed the second metatarsal head overlay templates on the radiograph, and selected the size that most precisely matched the contour of the second metatarsal head with adequate lateral coverage. The diameter interval between templates is 1 mm
The patients were then evaluated and classified (as grade 0, 1, 2, or 3) according to joint-space narrowing, subchondral sclerosis, osteophyte formation (dorsal, lateral, and medial), and subchondral cystic changes.
Statistical analysis was performed by using an independent Student’s t test, with the level of significance set at P < 0.05. The Spearman’s correlation test was used to evaluate the correlation between the radiographic classification and the parameters. The study was completed with appropriate institutional review board approval.
Results
Intraclass correlation coefficients (ICCs) were generated for all radiographic measurements. All measurements were higher than 0.75 (indicating acceptable reliability) and were employed in the study. There were no significant differences in age, hallux valgus angle, or first–second intermetatarsal angle between the study and control groups. The metatarsal lengths and differences between the two groups are shown in Table 1. The average second metatarsal length was significantly longer in the study group than in the control group (P = 0.01); however, the average lengths of the first and fourth metatarsals were not significantly different between the two groups.
Table 1.
Metatarsal length
| Number | Second toe rigidus group, mm | Control group, mm | P value |
|---|---|---|---|
| First metatarsal | 63.9 (4.1) | 64.4 (3.2) | 0.45 |
| Second metatarsal | 77.8 (6.0) | 74.8 (3.6) | 0.01 |
| Fourth metatarsal | 71.9 (5.3) | 70.6 (3.4) | 0.17 |
Results are presented as mean (SD)
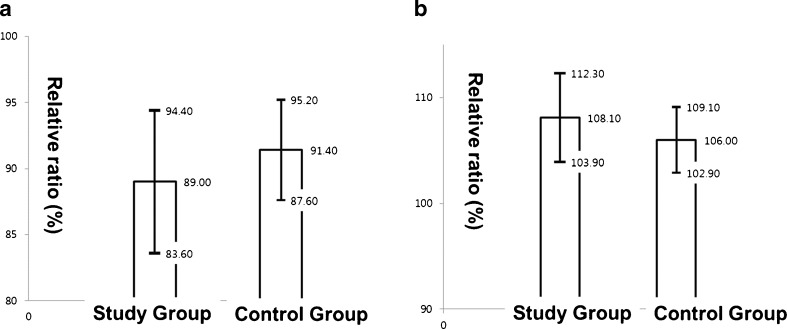
The average length of the first metatarsal relative to the fourth metatarsal (Fig. 5a) was significantly shorter (P = 0.02) in the study group (average, 89 % [95 % confidence interval (CI), 83.6 %–94.4 %]), compared with the control group (average, 91.4 % [95 % CI, 87.6 %–95.2 %]). The average length of the second metatarsal relative to the fourth metatarsal (Fig. 5b) was significantly longer (P = 0.01) in the study group (average, 108.1 % [95 % CI, 103.9 %–112.3 %]), compared with the control group (average, 106 % [95 % CI, 102.9 %–109.1 %]). These data suggest that patients with arthritis of the second metatarsophalangeal joint had both a long second metatarsal and a short first metatarsal, compared with patients without arthritis of this joint.
Fig. 5.
a Graph showing the length of the first metatarsal as a percentage of the fourth metatarsal ([first metatarsal length × 100]/fourth metatarsal length). This ratio was significantly lower in the study group than in the control group (P = 0.02). b Graph showing the length of the second metatarsal as a percentage of the fourth metatarsal ([second metatarsal length × 100]/fourth metatarsal length). This ratio was significantly higher in the study group than in the control group (P = 0.01)
There was no significant difference in the metatarsus adductus angle between the two groups. The study group had an average angle of 17.2° (SD, 4°), and showed a tendency toward a mild adductus position of the metatarsals relative to the midfoot.
The mean (SD) and P value for the difference between the two groups with regard to the diameter of the second metatarsal head and the ratio of the diameter of the second metatarsal head relative to the length of the fourth metatarsal are shown Table 2. The average diameter of the second metatarsal head was significantly larger in the study group than in the control group (P = 0.00), and the average ratio of the diameter of the second metatarsal head relative to the length of the fourth metatarsal was significantly higher in the study group than in the control group (P = 0.00). Therefore, patients with arthritis of the second metatarsophalangeal joint had an expanded shape of the second metatarsal head, compared with the control group.
Table 2.
Second metatarsal head size
| Parameter | Second toe rigidus group | Control group | P value |
|---|---|---|---|
| Diameter, mm | 17.2 (1.3) | 15.9 (0.8) | .00 |
| Ratio to 4MTa, % | 24.2 (2.7) | 22.5 (1.2) | .00 |
Results are presented as mean (SD)
a Ratio of diameter of second metatarsal head relative to length of fourth metatarsal
The amount of second metatarsophalangeal joint degeneration was graded according to findings on anteroposterior radiographs, including joint-space narrowing, subchondral sclerosis, osteophyte formation (lateral, medial), and subchondral cystic changes. Lateral radiographs were used to assess dorsal osteophyte formation. We classified the patients according to 4 grades: grade 0, visible and well-preserved joint space, like a nearly normal joint; grade 1, mild to moderate osteophyte formation, joint-space narrowing, and subchondral sclerosis; grade 2, marked osteophyte formation, joint-space narrowing, and subchondral sclerosis; grade 3, marked osteophyte formation, loss of visible joint space, and presence of subchondral cysts. Four feet were classified as grade 0, nine as grade 1 (nine with mild narrowing of the joint space and four with osteophyte formation), 17 as grade 2, and seven as grade 3 (Fig. 6). No significant relationship was found between the grade of the second metatarsophalangeal joint arthritis and all the radiographic parameters.
Fig. 6.
Radiographs demonstrating the classification of second toe rigidus. A Radiograph demonstrating grade 0 second toe rigidus with a well-preserved joint space. B Radiograph demonstrating grade 1 second toe rigidus with marginal osteophyte formation and mild joint-space narrowing. C Radiograph demonstrating grade 2 second toe rigidus with marked osteophyte formation, marked joint-space narrowing, and subchondral sclerosis. D Radiograph demonstrating grade 3 second toe rigidus with loss of the joint space, and the presence of a subchondral bone cyst
Discussion
The purpose of this study was to evaluate the radiographic characteristics and structural configurations of a series of patients with primary degenerative arthritis of the second metatarsophalangeal joint. Primary or nontraumatic degenerative arthritis of this joint has not been discussed in the literature, and only fleetingly mentioned in descriptions of second metatarsophalangeal joint instability [2], and Freiberg’s infraction [3]. In this study, all patients with primary degenerative arthritis of the second metatarsophalangeal joint report a generalised decrease in motion, with particular limitation in dorsiflexion, of this joint. This clinical manifestation differs from that of second metatarsophalangeal joint instability. Hoskinson [4] noted that the earliest radiographic finding in Freiberg’s infraction is widening of the joint space. Subsequently, there is an increase in bone density within the subchondral bone and central joint depression, followed by an area of rarefaction proximal to the subchondral bone surrounded by a sclerotic rim. In contrast to the radiographic findings in Freiberg’s infraction, the findings in primary arthritis of the second metatarsophalangeal joint are similar to those in degenerative arthritis of the other joints, especially hallux rigidus [1]. Narrowing of the joint space and osteophytic changes, primarily involving the dorsal aspect of the joint, were seen in this study. We also found degenerative spurs along the margin of the metatarsal head and base of the proximal phalanx, and cartilage denudation on the dorsal aspect of the metatarsal head in all the patients intraoperatively. In addition, degenerative changes without evidence of avascular necrosis were shown on histological examination. On the basis of these radiographic, intraoperative findings and histopathological examination, we propose a new diagnosis, which we have termed “second toe rigidus” (Table 3).
Table 3.
Radiographic classification of second toe rigidus
| Grade | Radiographic findingsa |
|---|---|
| 0 | Normal |
| 1 | Mild to moderate osteophyte formation, minimal joint-space narrowing, minimal subchondral sclerosis |
| 2 | Marked osteophyte formation, marked joint-space narrowing, marked subchondral sclerosis |
| 3 | Same as grade 2 but with loss of joint space and subchondral bone cyst formation |
aWeight bearing and anteroposterior and lateral radiographs
In an earlier literature review, a similar case of second toe rigidus was reported [9]. Histopathological examination of the second metatarsal head in the 55-year-old patient revealed no evidence of osteonecrosis. Instead, it showed that shearing had occurred through the tidemark to separate the articular cartilage. The authors reported osteochondral disruption of the second metatarsal head as a variant of Freiberg’s infraction, but we believe the patient’s lesion could be considered second toe rigidus.
This study revealed that the diameter of the second metatarsal head and the ratio of the diameter of the second metatarsal head relative to the length of the fourth metatarsal were large and high, respectively, in the second toe rigidus group. These findings were considered the result of degenerative change with proliferative periarticular bone formation in the second metatarsal head. We suggest that an increase in the second metatarsal head size may be considered an early sign of the disease in patients with limited motion.
We found that the second metatarsal was long in the second toe rigidus group. Also, in comparison with the fourth metatarsal, the first metatarsal was short and the second metatarsal was long. The second metatarsal is the longest [10], and has been shown to sustain the greatest stresses during normal activity [11]. The keystone configuration of the tarsometatarsal joint confers substantial stability to the second metatarsal base. Therefore, this bone is the least mobile, potentially increasing the stress on the metatarsal head distally. Furthermore, toe dorsiflexion pushes the metatarsal head downwards toward the sole during the toe-off phase, generating compressive and shear forces at the dorsal aspect of the head, and damaging the articular cartilage as the base of the proximal phalanx rides dorsally over the metatarsal. These facts may explain the association between second toe rigidus and a functionally long second metatarsal.
A widened first–second intermetatarsal angle theoretically would affect the measurement of the second metatarsal length. Davitt et al. [7] addressed this issue by measuring the functional length, which they defined as the length of the first metatarsal as projected along the axis of the second metatarsal. In our study, there was no significant difference between the two groups with regard to the intermetatarsal angle; therefore, the groups could be compared without using the functional lengths.
The metatarsus adductus angle was measured to assess the possibility that adduction of the second metatarsal might increase the incidence of arthritis by causing geometric change in the second metatarsophalangeal joint. Although there is one report [12] suggesting that metatarsus adductus has a relationship to the development of osteoarthritis of the second tarsometatarsal joint, there was no significant difference in the metatarsus adductus angle between the study group and control group in our study.
This study has some limitations. First, the number of patients was small due to the rare nature of this condition. Second, the study was performed as a retrospective review of the radiographic images. We tried to minimise variations due to radiographic technique by using the same X-ray machine in the same manner for all subjects. Finally, the analysed data were all relative measurements with internal controls.
In summary, second toe rigidus should be considered a diagnosis in patients with painful limited dorsiflexion of the second metatarsophalangeal joint without evidence of Freiberg’s infraction or trauma. We suggest that a functionally long second metatarsal is a possible mechanical aetiology for this condition. We propose that second toe rigidus be classified according to 4-graded radiographic findings, including joint-space narrowing, osteophyte formation, subchondral sclerosis, and subchondral cyst formation. This study is the first step in developing the diagnosis and treatment strategies for this rare condition.
Acknowledgments
We wish to thank Ms HY Lee for her help with the chart reviews during this study.
Author contributions
All authors have contributed to the conception and design of the study; acquisition, analysis and interpretation of data; and drafting and final approval of the article. Dr. WC Lee takes responsibility for the integrity of the work.
Conflict of interest
All authors have no conflicts of interest.
References
- 1.Coughlin MJ, Shurnas PS. Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am. 2003;85-A:2072–2088. [PubMed] [Google Scholar]
- 2.Coughlin MJ. Second metatarsophalangeal joint instability in the athlete. Foot Ankle. 1993;14:309–319. doi: 10.1177/107110079301400601. [DOI] [PubMed] [Google Scholar]
- 3.Carmont MR, Rees RJ, Blundell CM. Current concepts review: Freiberg’s disease. Foot Ankle Int Am Orthop Foot Ankle Soc Swiss Foot Ankle Soc. 2009;30:167–176. doi: 10.3113/FAI.2009.0167. [DOI] [PubMed] [Google Scholar]
- 4.Hoskinson J. Freiberg’s disease: a review of the long-term results. Proc R Soc Med. 1974;67:106–107. doi: 10.1177/003591577406700209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee SK, Chung MS, Baek GH, Oh JH, Lee YH, Gong HS. Treatment of Freiberg disease with intra-articular dorsal wedge osteotomy and absorbable pin fixation. Foot Ankle Int Am Orthop Foot Ankle Soc Swiss Foot Ankle Soc. 2007;28:43–48. doi: 10.3113/FAI.2007.0008. [DOI] [PubMed] [Google Scholar]
- 6.Smillie IS. Treatment of Freiberg’s infraction. Proc R Soc Med. 1967;60:29–31. doi: 10.1177/003591576706000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davitt JS, Kadel N, Sangeorzan BJ, Hansen ST, Jr, Holt SK, Donaldson-Fletcher E. An association between functional second metatarsal length and midfoot arthrosis. J Bone Joint Surg Am. 2005;87:795–800. doi: 10.2106/JBJS.C.01238. [DOI] [PubMed] [Google Scholar]
- 8.Kaz AJ, Coughlin MJ. Crossover second toe: demographics, etiology, and radiographic assessment. Foot Ankle Int Am Orthop Foot Ankle Soc Swiss Foot Ankle Soc. 2007;28:1223–1237. doi: 10.3113/FAI.2007.1223. [DOI] [PubMed] [Google Scholar]
- 9.Young MC, Fornasier VL, Cameron HU. Osteochondral disruption of the second metatarsal: a variant of Freiberg’s infraction? Foot Ankle. 1987;8:103–109. doi: 10.1177/107110078700800206. [DOI] [PubMed] [Google Scholar]
- 10.Sarrafian SK (1993) Anatomy of the foot and ankle: Descriptive, anatomical and functional. Lippincott Williams & Wilkins, Philadelphia
- 11.Donahue SW, Sharkey NA. Strains in the metatarsals during the stance phase of gait: implications for stress fractures. J Bone Joint Surg Am. 1999;81:1236–1244. doi: 10.2106/00004623-199909000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Ito K, Tanaka Y, Takakura Y. Degenerative osteoarthrosis of tarsometatarsal joints in hallux valgus: a radiographic study. J Orthop Sc Offi J Jpn Orthop Assoc. 2003;8:629–634. doi: 10.1007/s00776-003-0691-1. [DOI] [PubMed] [Google Scholar]