Abstract
Introduction
Total ankle arthroplasty is increasingly used as an alternative to arthrodesis to treat advanced ankle arthritis. However, the outcomes and postoperative complications are poorly described.
Patients and methods
Between March 2005 and May 2010 114 S.T.A.R. prostheses were implanted by one surgeon at our institution. We retrospectively analysed the demographics, clinical outcomes and radiographic characteristics of 100 ankle prostheses (97 patients).
Results
The average follow up was 36 months. The average preoperative AOFAS score of 36.87 (22–58) significantly increased to 75.99 postoperative. A total of 87 % of the patients reported a better life quality. Twenty-seven ankles incurred complications after primary surgery, and 21 prostheses required revision surgery, including four patients who required arthrodesis.
Conclusion
Our study shows a high satisfaction rate after total ankle replacement and clear pain relief. Patients with a body mass Index higher than 30 showed a higher rate of complications. Compared with ankle fusion, the rates of complications are comparable.
Introduction
Despite high numbers of failures in early generations of total ankle arthroplasty (TAA), a continued and increasing interest in the use of these devices for end-stage arthritis as an alternative to arthrodesis of the ankle exists [1–5]. However, while some studies report encouraging mid-term results, the rate of complications after TAA is high compared to total hip and knee replacement [6–10].
The primary purpose of this retrospective study was to report the complication rate of all patients at a single institution undergoing a total ankle arthroplasty with a minimum follow-up of two years. In addition, patient satisfaction, implant survivorship, and risk factors for complications were analysed.
Patients and methods
This study was IRB approved. Between March 2005 and May 2010, 114 S.T.A.R.® prostheses (Small Bone Innovations, Inc., New York, USA) in 97 patients were implanted by the senior author (W.K.) at a single institution. The patient population consisted of 53 females and 44 males with an average age of 63 years (range 41–80) and an average BMI of 28.4 (range 21.7–38.6). The etiologies of arthritis in the 97 patients are presented in Table 1.
Table 1.
Indications for surgery
| Indication for surgery | Number of cases |
|---|---|
| Post-traumatic arthritis | 81 |
| Rheumatoid arthritis | 9 |
| Primary osteoarthritis | 8 |
| Secondary osteoarthritis due to haematochromatosis | 2 |
Pre-operative assessment included a thorough history and physical examination and evaluation of the AOFAS score. Patients with a valgus or varus deformity of greater than 15° were excluded [3].
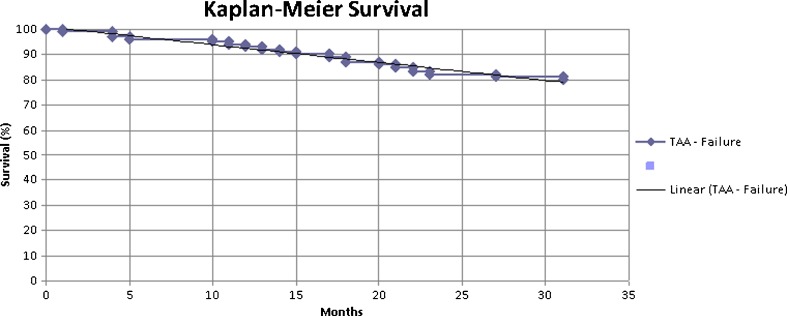
Postoperatively, patients were examined clinically at six weeks, at one year and at two years using the AOFAS score. In addition, they were asked about their satisfaction and if they would have the surgery again, using a standardized questionnaire. Furthermore, patient’s charts were reviewed to retrieve information regarding potential risk factors such as diabetes, peripheral vascular disease, rheumatoid arthritis and smoking. Radiographic assessment included serial postoperative radiographs using anteroposterior (AP) and lateral views of the upper ankle joint immediately after surgery, six weeks after surgery and yearly thereafter. Wound healing problems were defined as the inability of the skin to within three weeks after surgery. Statistical analysis was performed at our clinical centre using SPSS (IBM®) together with our clinic statistician. The Kaplan-Meier survivorship curve was generated utilizing Microsoft Excel.
Surgical technique
All operations were performed with the use of a tourniquet, using a standard anterolateral midline incision approach in the interval between the extensor hallucis longus and anterior tibialis tendon. After the incision of the anterior capsule, subperiostal mobilization of the soft tissues was performed and the tibiotalar joint was adequately exposed. Routine bone preparation included removal of tibial or talar osteophytes, resection of the tibial and talar articular cartilage and implantation of the components after soft tissue balancing using cementless techniques. Additional procedures included percutaneous lengthening of the Achilles tendon (12 patients), subtalar fusion (five patients), and a calcaneus osteotomy (three patients) to correct the hindfoot alignment.
Routine postoperative protocol included perioperative antibiotics (third generation cephalosporin) for 24 hours and immobilization of the patient until postoperative swelling resolved, usually within 48–72 hours after surgery. Patients were then allowed to be partial weight bearing with 30 kg, using walking aids and a long walking boot for three weeks and were then advanced to full weight bearing in a walker boot between four and six weeks after surgery. Sutures were removed 14 days after the surgery.
Results
One hundred cases (97 patients) out of 114 were included in this retrospective review. Three patients were deceased and six patients were lost to follow-up. Two patients were unable to attend routine clinical exams or to answer the questionnaire and therefore were excluded. Another two patients were unable to attend clinical follow-up visits due to arthritic problems and other medical comorbidities, unrelated to surgery. For all patients included, a complete clinical and radiographic follow-up was available at 2.5 years.
The pre-operative AOFAS score increased from 36.87 (range 22–58) pre-operatively to 75.99 (range 42–96) postoperative (p < 0.005). When patients were asked about quality of life after surgery and whether they would undergo surgery again, 87/97 (90 %) patients reported a better life quality after surgery and 82/97 (85 %) patients would make a decision to undergo ankle replacement again. Seventy-two of the cases in our study had no complications and good pain relief with improved function following total ankle replacement.
There were 21 revision surgeries (21 %) after the index procedure. Six cases had to be revised due to aseptic loosening (6 %), and two of these cases had multiple revisions before they finally were converted to an arthrodesis. In five of these cases one or both components had failed due to technical error. Two of these cases showed progressive osteolysis on either the tibial or talar component. The osteolytic defects were filled using autologous bone on the tibia and talus, but the components were not grossly loose during surgery as we pre-operatively suspected and thought would be a sign of loosening. A total of 50 % of the aseptic cases were due to patients having a BMI > 30 (p = 0.01). Other comorbidities were not statistically significant for occurrence of aseptic loosening (smoking [one] /cardiovascular disease [one], p = 0.06).
Four prosthesis (4 %) had to be revised due to deep infection. Of these four infections, one was converted to an ankle fusion that later required plastic surgery coverage using a muscle flap and the three others were revised using a two stage revision, with a short-term cement spacer with intravenous antibiotics and subsequent cemented total ankle arthroplasty.
One patient was revised due to chronic and continued pain after implantation of TAA. She had been on chronic pain medication before surgery and continued to have pain after the TAA was removed and fusion was performed.
A total of ten revision procedures were required due to recurrent arthrofibrosis or bony impingement, resulting in reduced mobility and range of motion. The complications were treated with open debridement and arthrolysis as well as removal of recurrent osteophytes and downsizing of the talar component in four cases. Three of these cases received an Achilles tendon lengthening. In all of these cases, components were well fixed and seemed well aligned.
Six prosthesis (6 %) showed delayed wound healing which was treated nonoperatively with oral antibiotics and wound debridement. They all did well thereafter. Of these six, three had a BMI over 30, and two of them had been smoking for more than 12 years (12 pack years) as a possible risk factor for wound healing problems.
For better illustration the overall survivorship data is presented as a Kaplan-Meier survival curve (Fig. 1).
Fig. 1.
Survivorship data of the prostheses
Intraoperative complications included fractures of the lateral malleoli in two cases. One of them was noted intraoperatively and was treated with open reduction and plating of the fracture, the other case showed a fissure of the malleolus, discovered on postoperative radiographs. This required no treatment and went on to heal uneventfully without surgery (Table 2).
Table 2.
Reasons for revision surgery
| Reason for revision surgery | Patients, n | Additional risk factors | Final surgery |
|---|---|---|---|
| Aseptic loosening | 6 | Three obesity, one smoker, one cardiovascular disease | Two arthrodesis |
| Deep infection | 4 | Two obesity, one osteoporosis, one cardiovascular disease | One arthrodesis |
| Chronic pain | 1 | Arthrodesis | |
| Arthrofibrosis/impingement | 10 |
Discussion
The interest in TAA continues to rise with currently more than 20 TAA designs available worldwide. TAA in general is considered to be a cost-effective alternative to arthrodesis. Compared with total ankle arthroplasty, ankle fusion is associated with a higher rate of pseudarthrosis, loss of mobility and progressive arthritis in the adjacent joints. Furthermore, ankle fusion has a complication rate up to 60 %. The main reasons for revision following arthrodesis are nonunion, malunion, infection and wound complications [11–14].
In regards to functional outcome and gait, as well as the patient’s quality of life, TAA has been shown to have better results than ankle arthrodesis because arthrodesis of the ankle leads to an abnormal gait and the rehabilitation time is much longer [14, 15]. Furthermore, a lot of patients show a slower velocity, slower cadence and shorter stride after ankle fusion [11, 12, 16].
On the other hand studies performed recently show a similar complication rate between ankle fusion and ankle replacement [13, 17–19].
The third generation of the STAR® ankle prosthesis include a minimally constrained design which utilizes a mobile meniscal-bearing polyethylene insert, uncemented fixation and a three-component design. Using the third generation implants Wood et al. [3] reported a five- and ten-year survivorship of 93 % and 80 % for the STAR prosthesis while Nunley et al. showed a survivorship of 88 % after 24–104 months [10].
Even with these improvements the complication rates still vary between 20 % and 28 %. The current literature shows revision rates between 14 % and 32 % after five years [1, 20–23]. Although our study had an average follow-up of 2.5 years our results are comparable to other studies. Systematic review of the literature shows that 27–60 % of the patients report persistent discomfort following TAA. The most common reasons for revision of TAA are aseptic loosening, especially of the talar component, osteolysis and osteonecrosis of the talus. Furthermore, instability and intra- or postoperative fracture, implant failure, subsidence, especially of the talus component, deep infection and wound healing problems are common reasons for failure of a total ankle replacement.
Valderrabano et al. and Henricson showed that the complexity of total ankle surgery is represented by the high rate of additional operations required due to malleolar impingement, the necessity to correct hindfoot varus, arthritis of the other joints surrounding the ankle and arthrofibrosis [9]. Single staged, multilevel operations might not be the best option concerning the high complication rate [3, 19, 24]. However, studies have shown that complication rates following TAA decrease with increasing surgeon experience [21].
In addition to surgeon factors, studies have evaluated risk factors for the survivorship of total ankle replacement. Whalen et al. showed that coronary artery disease or peripheral vascular disease and a smoking history of greater than 12-pack-years are risk factors for wound necrosis [22]. Other independent variables suspected to increase the likelihood of complications include a high body mass index (BMI), diabetes, sex, age under 60, long tourniquet times, and inflammatory arthritis [23, 25, 26]. Although BMI and age might be risk factors for complications, they are not contraindications to TAA. However, it is suggested that the STAR prosthesis be implanted in individuals who weigh less than 120 kg. The only absolute contraindications include ongoing persistent infection in the joint, osteonecrosis of the talus, and poor bone quality.
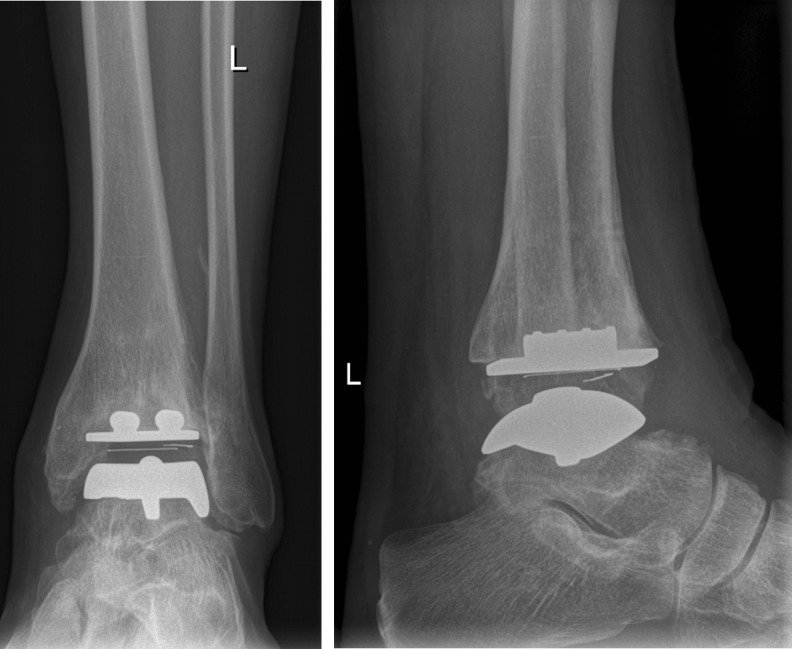
Seventy two of the cases in our study had no complications and good pain relief with improved function following total ankle replacement (c.f. Figs. 2 and 3). Eighty two of our patients were satisfied enough that they would have their ankle replaced again. Eighty seven of our patients reported a better life quality after primary or revision surgery at the time of examination. One limitation to our study is that we did not utilise psychometric data. It would perhaps be an interesting study to use, for example, the SF 36 in a further study like Esparragoza et al. did in their study [17].
Fig. 2.
Pre-operative conditions in one patient of the study population with severe arthritis of the upper ankle joint in AP (a) and lateral (b) views
Fig. 3.
The same patient as in Fig. 2 at the two-year follow-up visit in our clinic with no signs of aseptic loosening, subluxation or implant failure in AP (a) and lateral (b) views
Our survival and complication rates are similar to those of other studies using the STAR prosthesis and other designs [1–3, 6, 7, 10]. Though the majority of the patients in our cohort were satisfied with their result, TAA does show a higher complication rate than joint replacement surgeries of the hip and knee. Thus, patients must be properly informed and their expectations must be reasonable before considering TAA.
Wound healing problems in general occurred in 6 % of our cohort. Interestingly, in most of the cases these were located at the mid-portion of the anterior incision. They mostly occurred when patients started mobilization using crutches and a walker boot, where an anterior lid was fixed anteriorly using straps. Patients also often complained about soft tissue irritations during that time. We therefore changed our postoperative protocol and mobilized patients using the same type of walking boot but without the anterior lid. We noticed that these changes significantly decreased the incidence of wound healing problems. In a series of 42 TAAs in 2010 performed by the same surgeon (W.K.), only two cases of wound healing problems occurred after modification of this regimen (unpublished data). Nonetheless it should be stressed again that subtle preparation and handling of the soft tissues at the time of surgery remains of utmost importance.
Ten cases needed to receive additional operations. The main reason was the development of ossifications/osteophytes, especially in the area of the medial malleolus or the anterior part of the ankle, leading to impingement and loss of mobility. One case had a dislocation of the polyethylene. Another common reason was a tendoachilles contracture leading to equinus, which led to reduced ankle range of motion, especially when present in combination with arthrofibrosis.
The limitations of our study include the retrospective design and the lack of comparison to a matched cohort of patients who received an ankle arthrodesis. In addition, some bias may have been introduced since the senior author and operating surgeon recorded the AOFAS score for all patients, especially because the AOFAS score mostly takes pain into consideration. Other important outcomes like gait and postoperative joint alignment are neglected. However, to our knowledge there is no standardised score in foot and ankle surgery that has a similar validity and we use it like other authors [3, 8, 10].
Finally, the duration of follow-up was short and our complication rate comparable to other studies with average follow-up time relatively long. However, the authors’ purpose was to establish the early complication rates associated with total ankle arthroplasty, using a relatively large cohort of patients, given that TAA is not performed frequently in most societies.
Conclusion
Although complications after total ankle replacement are frequent, TAA can reliably improve a person’s quality of life. Nevertheless, the patient selection and education is essential. Cardiovascular and peripheral vascular disease, smoking, osteoporosis and overweight are risk factors for a worse survival rate. Pre-operative MRI and long-leg X-rays to evaluate any angular deformities of other joints are recommended. Additionally, angiography and neurological examination is recommended for selected patients.
Despite the fact that complication rates are still high, TAA offers a cost-effective alternative to ankle fusion. Further, total ankle replacement offers a better mobility, improved gait and reduces the subsequent subtalar joint arthritis. Improved operative technique, surgeon experience, as well as appropriate patient selection may lead to a decreasing complication rate and a favourable approach to arthrodesis.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Stephanie Noelle and Claus C. Egidy contributed to this work equally.
Contributor Information
Stephanie Noelle, Email: StephanieNoelle@gmx.de.
Claus C. Egidy, Email: claus.egidy@gmail.com
Michael B. Cross, Email: CrossM@HSS.EDU
Matthias Gebauer, Email: Matthias.gebauer@helios-kliniken.de.
Wolfgang Klauser, Phone: +49-40-31971233, Email: wolfgang.klauser@helios-kliniken.de.
References
- 1.Anderson T, Montgomery F, Carlsson A. Uncemented STAR total ankle prostheses. Three to eight-year follow-up of fifty-one consecutive ankles. J Bone Joint Surg Am. 2003;85-A(7):1321–1329. [PubMed] [Google Scholar]
- 2.Karantana A, Hobson S, Dhar S. The Scandinavian total ankle replacement: survivorship at 5 and 8 years comparable to other series. Clin Orthop Relat Res. 2010;468(4):951–957. doi: 10.1007/s11999-009-0971-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wood PL, Clough TM, Smith R. The present state of ankle arthroplasty. Foot Ankle Surg. 2008;14(3):115–119. doi: 10.1016/j.fas.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 4.Schuh R, Hofstaetter J, Krismer M, Bevoni R, Windhager R, Trnka HJ. Total ankle arthroplasty versus ankle arthrodesis. Comparison of sports, recreational activities and functional outcome. Int Orthop. 2012;36(6):1207–1214. doi: 10.1007/s00264-011-1455-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kwon DG, Chung CY, Park MS, Sung KH, Kim TW, Lee KM. Arthroplasty versus arthrodesis for end-stage ankle arthritis: decision analysis using Markov model. Int Orthop. 2011;35(11):1647–1653. doi: 10.1007/s00264-011-1336-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Easley ME, Adams SB, Jr, Hembree WC, DeOrio JK. Results of total ankle arthroplasty. J Bone Joint Surg Am. 2011;93(15):1455–1468. doi: 10.2106/JBJS.J.00126. [DOI] [PubMed] [Google Scholar]
- 7.Spirt AA, Assal M, Hansen ST., Jr Complications and failure after total ankle arthroplasty. J Bone Joint Surg Am. 2004;86-A(6):1172–1178. doi: 10.2106/00004623-200406000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Skytta ET, Koivu H, Eskelinen A, Ikavalko M, Paavolainen P, Remes V. Total ankle replacement: a population-based study of 515 cases from the Finnish Arthroplasty Register. Acta Orthop. 2010;81(1):114–118. doi: 10.3109/17453671003685459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Valderrabano V, Hintermann B, Dick W. Scandinavian total ankle replacement: a 3.7-year average followup of 65 patients. Clin Orthop Relat Res. 2004;424:47–56. doi: 10.1097/01.blo.0000132245.18548.09. [DOI] [PubMed] [Google Scholar]
- 10.Nunley JA, Caputo AM, Easley ME, Cook C. Intermediate to long-term outcomes of the STAR Total Ankle Replacement: the patient perspective. J Bone Joint Surg Am. 2012;94(1):43–48. doi: 10.2106/JBJS.J.01613. [DOI] [PubMed] [Google Scholar]
- 11.Slobogean GP, Younger A, Apostle KL, Marra CA, Wing K, Penner M, Daniels T, Glazebrook M. Preference-based quality of life of end-stage ankle arthritis treated with arthroplasty or arthrodesis. Foot Ankle Int. 2010;31(7):563–566. doi: 10.3113/FAI.2010.0563. [DOI] [PubMed] [Google Scholar]
- 12.Thomas R, Daniels TR, Parker K. Gait analysis and functional outcomes following ankle arthrodesis for isolated ankle arthritis. J Bone Joint Surg Am. 2006;88(3):526–535. doi: 10.2106/JBJS.E.00521. [DOI] [PubMed] [Google Scholar]
- 13.Krause FG, Windolf M, Bora B, Penner MJ, Wing KJ, Younger AS. Impact of complications in total ankle replacement and ankle arthrodesis analyzed with a validated outcome measurement. J Bone Joint Surg Am. 2011;93(9):830–839. doi: 10.2106/JBJS.J.00103. [DOI] [PubMed] [Google Scholar]
- 14.Mazur JM, Schwartz E, Simon SR. Ankle arthrodesis. Long-term follow-up with gait analysis. J Bone Joint Surg Am. 1979;61(7):964–975. [PubMed] [Google Scholar]
- 15.Haddad SL, Coetzee JC, Estok R, Fahrbach K, Banel D, Nalysnyk L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg Am. 2007;89(9):1899–1905. doi: 10.2106/JBJS.F.01149. [DOI] [PubMed] [Google Scholar]
- 16.Beyaert C, Sirveaux F, Paysant J, Mole D, Andre JM. The effect of tibio-talar arthrodesis on foot kinematics and ground reaction force progression during walking. Gait Posture. 2004;20(1):84–91. doi: 10.1016/j.gaitpost.2003.07.006. [DOI] [PubMed] [Google Scholar]
- 17.Esparragoza L, Vidal C, Vaquero J. Comparative study of the quality of life between arthrodesis and total arthroplasty substitution of the ankle. J Foot Ankle Surg. 2011;50(4):383–387. doi: 10.1053/j.jfas.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 18.SooHoo NF, Zingmond DS, Ko CY. Comparison of reoperation rates following ankle arthrodesis and total ankle arthroplasty. J Bone Joint Surg Am. 2007;89(10):2143–2149. doi: 10.2106/JBJS.F.01611. [DOI] [PubMed] [Google Scholar]
- 19.Saltzman CL, Kadoko RG, Suh JS. Treatment of isolated ankle osteoarthritis with arthrodesis or the total ankle replacement: a comparison of early outcomes. Clin Orthop Surg. 2010;2(1):1–7. doi: 10.4055/cios.2010.2.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Glazebrook MA, Arsenault K, Dunbar M. Evidence-based classification of complications in total ankle arthroplasty. Foot Ankle Int. 2009;30(10):945–949. doi: 10.3113/FAI.2009.0945. [DOI] [PubMed] [Google Scholar]
- 21.Haskell A, Mann RA. Perioperative complication rate of total ankle replacement is reduced by surgeon experience. Foot Ankle Int. 2004;25(5):283–289. doi: 10.1177/107110070402500502. [DOI] [PubMed] [Google Scholar]
- 22.Whalen JL, Spelsberg SC, Murray P. Wound breakdown after total ankle arthroplasty. Foot Ankle Int. 2010;31(4):301–305. doi: 10.3113/FAI.2010.0301. [DOI] [PubMed] [Google Scholar]
- 23.Myerson MS, Mroczek K. Perioperative complications of total ankle arthroplasty. Foot Ankle Int. 2003;24(1):17–21. doi: 10.1177/107110070302400102. [DOI] [PubMed] [Google Scholar]
- 24.Seth A. A review of the STAR prosthetic system and the biomechanical considerations in total ankle replacements. Foot Ankle Surg. 2011;17(2):64–67. doi: 10.1016/j.fas.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 25.Baker JF, Perera A, Lui DF, Stephens MM. The effect of body mass index on outcomes after total ankle replacement. Ir Med J. 2009;102(6):188–190. [PubMed] [Google Scholar]
- 26.Raikin SM, Kane J, Ciminiello ME. Risk factors for incision-healing complications following total ankle arthroplasty. J Bone Joint Surg Am. 2010;92(12):2150–2155. doi: 10.2106/JBJS.I.00870. [DOI] [PubMed] [Google Scholar]