Abstract
The aetiology of hallux valgus with regard to stability of the first metatarsocuneiform joint has historically been subject to much debate. Associations between the magnitude of the intermetatarsal angle and the hallux valgus angle have previously been established. Metatarsocuneiform joint coronal plane mobility is necessary for a concomitant increase in both of these angles. Although metatarsocuneiform joint hypermobility has been implicated in the development of a hallux valgus deformity, isolated sagittal plane instability has thus far not been proven to be a definitive cause.
Keywords: Hallux valgus, Metatarsocuneiform joint, Hallux valgus angle, Intermetatarsal angle
Introduction
The function of the first metatarsocuneiform joint has long been the subject of debate and controversy. The typical axis of motion of the first metatarsocuneiform joint is in a plantar–lateral and dorsal–medial plane (Fig. 1). Early reports focused on metatarsocuneiform joint mobility as a primary cause of hallux valgus deformities [1–3]. Little objective evidence has been published to support these theories, and recent reports present findings that may refute some of these claims [4–9]. While coronal plane mobility of the first metatarsocuneiform joint may allow a more substantial hallux valgus deformity to develop, sagittal plane mobility, we believe, is likely the result rather than the cause of this deformity. Morton [10–12] first suggested that first ray hypermobility is a pathologic entity contributing to a multitude of foot disorders; however, he never associated hypermobility with a hallux valgus deformity. Lapidus, in separate publications [1–3], was the first to propose that increased first ray mobility and hallux valgus deformity were associated. He suggested that coronal plane deviation and the development of hallux valgus deformity developed secondarily after a pathologic increase in first ray sagittal mobility. A component of his surgical treatment for hallux valgus deformity included arthrodesis of the first metatarsocuneiform joint for stabilization of the first ray.
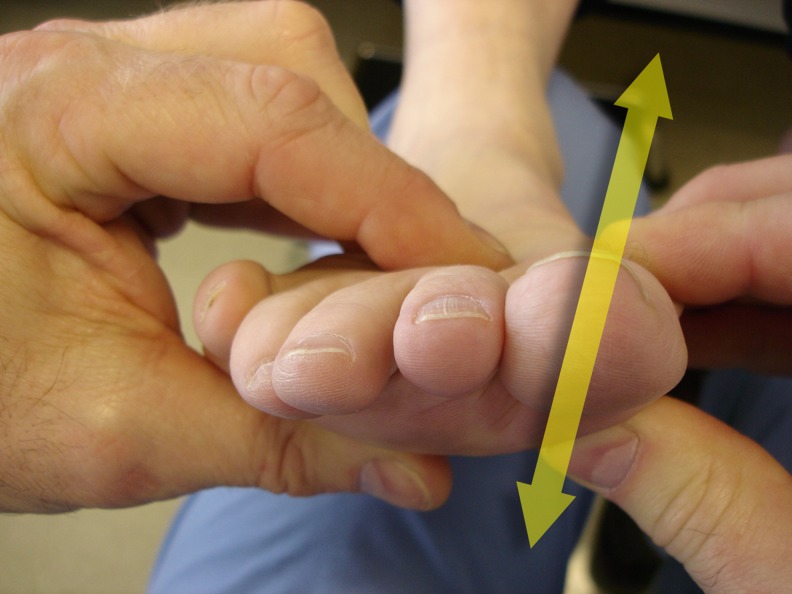
Fig. 1.
Axis of first ray motion and mobility. Axis of motion of the first metatarsocuneiform joint is in a plantar medial to dorsal lateral plane (used with permission, Surgery of the Foot and Ankle, 8th edition, Elsevier, Inc., Philadelphia, PA)
Morton and Lapidus had multiple reports supporting these theories, and their work still influences the surgical applications and clinical recommendations for many foot and ankle surgeons today [1–3, 10–12]. These early reports used subjective clinical examinations rather than strict objective criteria, and data quantifying the magnitude of pre-surgical and post-surgical first ray hypermobility was not included. Other authors have supported the theories of Morton and Lapidus, but have not objectively quantified the degree of first ray mobility or demonstrated that this mobility is the actual cause of hallux valgus [13–17]. Furthermore, the notion that this pathologic hypermobility is isolated to the first metatarsocuneiform joint has been hypothetical without evidence quantifying the location or magnitude of this mobility. More recently, some studies have presented compelling evidence to refute Morton’s original theories of hypermobility and its effects on hallux valgus [4–9, 18]. The purpose of this review was to summarize recent publications relating to first ray joint mobility and its role in the development of a hallux valgus deformity.
Laboratory testing
It is important to define whether first ray hypermobility is truly a pathologic entity [10, 12]. Furthermore, it would be helpful to determine whether this increased mobility occurs at the first metatarsocuneiform joint, or at other first ray joints, or in combination (first metatarsocuneiform, naviculocuneiform, talonavicular joints). Whitaker et al. [19], in an analysis of the kinematics of six nonpathologic cadaveric feet, reported that the talonavicular, naviculocuneiform, and metatarsocuneiform joints provided more sagittal plane mobility (27.4°) than the tibiotalar joint alone (23.2°). Faber et al. [20] presented their results of a cadaveric study evaluating the contribution of the metatarsocuneiform joint to first ray mobility in the transverse and sagittal planes. They found that the metatarsocuneiform joint contributed 82 % of medial mobility and 57 % of dorsal mobility when compared to the talonavicular and naviculocuneiform joints [20].
A key premise of Morton’s theory was that first ray instability led to increased weight-bearing of the second ray, and therefore, hypertrophy of the second metatarsal cortices [11]. This radiographic finding was listed as evidence of first ray hypermobility and listed as an indication for a first metatarsocuneiform joint arthrodesis during hallux valgus corrective surgery [21, 22]. Grebing et al. [8] studied the reliability of this radiographic sign and found no association between first ray mobility and cortical hypertrophy. They compared a control group with three other groups consisting of patients with interdigital neuromas, hallux valgus, and hallux rigidus, and reported no significant difference in the second metatarsal cortical thickness in any of the subgroups.
In the initial descriptions of first ray mobility [12], a subjective manual method was used to assess the degree of first ray mobility. The ankle is held in a neutral position and one hand is used to stabilize the lesser metatarsal heads, then the examiner grasps the first metatarsal with his index finger and thumb of the other hand and moves the first metatarsal head in a dorsal/plantar direction while estimating the amount of motion (Fig. 2a and b). Common terms used to describe the amount of mobility include a mild, moderate, substantial mobility, or hypermobile [1–3, 10–12, 16, 21, 23]. In Morton’s original work, in Lapidus’ publications, and in more recent publications on the results of the Lapidus procedure [1–3, 10–12, 14, 21, 23, 24], pre and postoperative first ray mobility were not quantified. Hypermobility was considered to be a preoperative condition and resolution following a metatarsocuneiform joint arthrodesis was felt to be a validation that the increased first ray mobility emanated from the first metatarsocuneiform joint [1–3, 23].
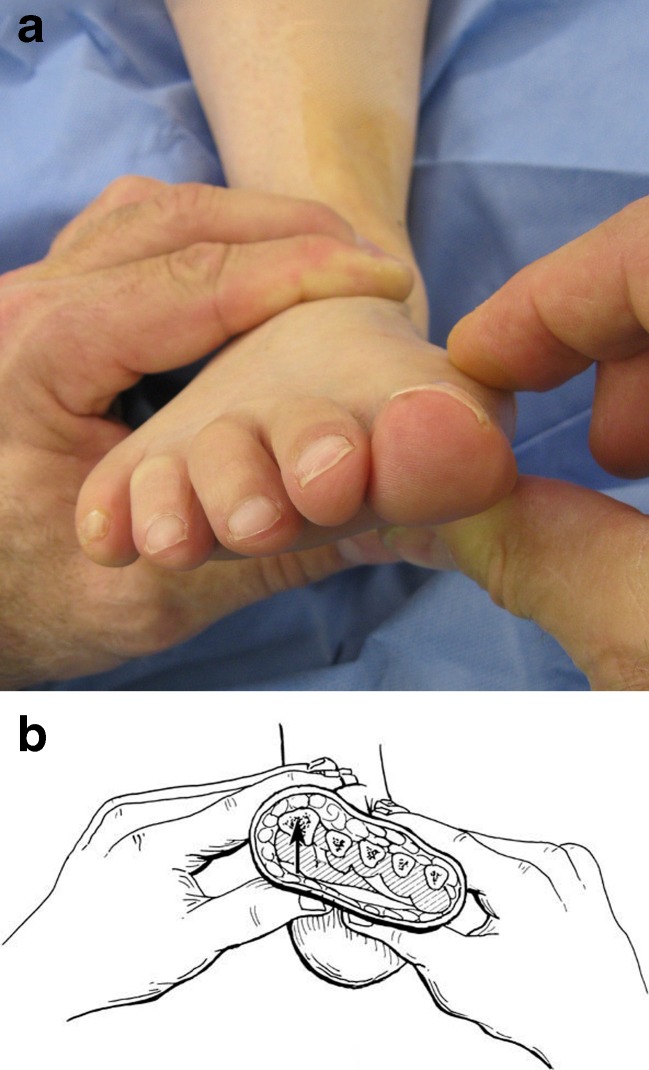
Fig. 2.
Morton’s manual exam of the first ray. a With the ankle in a neutral position and with one hand grasping the forefoot, the first ray is grasped and stabilized by the finger and thumb of the other hand. b The first ray is pushed in a dorsal position to assess the dorsal mobility of the first ray. It is pushed until a “soft endpoint” is reached (b used with permission, Surgery of the Foot and Ankle, 8th edition, Elsevier, Inc. Philadelphia, PA)
Glasoe [25] tested the reliability of Morton’s manual examination for first ray hypermobility with a group of three examiners assessing 15 volunteer subjects. The three examiners, including a surgeon and two physical therapists, compared intra-rater as well as inter-rater reliability. Intra-rater scores overall demonstrated agreement (kappa value of 0.73) from one session to the next when the same clinician examined the same subject on two separate occasions. Inter-rater scores demonstrated poor reliability with no consistency between exam findings when comparing the findings of all three clinicians (K < .0.16). There was no association (r = −0.21) between the physical examiner’s ability to grade dorsal mobility and the measure made by a well-validated mechanical device used to evaluate mobility. This led the authors to question the reliability and validity of manual estimates of first ray mobility and the variables of these manual examinations that may alter the parameters of the findings.
In 1994, Klaue et al. [15] developed a hand-held device that could be used to quantify first ray mobility. The device consists of an external caliper attached to an ankle-foot-orthosis. The caliper moves in a plantar and dorsal direction to measure sagittal plane motion [15] (Fig. 3a). In normal patients, the authors reported dorsal mobility to average 5 mm, while in those with hallux valgus, they observed mobility was greater than 8 mm of sagittal translation [14, 15, 17]. They defined that hypermobility of the first ray was present if there was greater than 8 mm of mobility. While Klaue et al. [15] quantified reproducible values with their device, the device did not selectively differentiate the measured mobility at the metatarsocuneiform joint from the other joints along the medial column. The Klaue device was subsequently validated by Jones et al. [9] using cadaveric limbs to compare stress radiographs with sagittal plane measurements. Glasoe et al. [26] later developed and validated another device which could be used to measure first ray mobility more precisely (Fig. 3b). This device applied a controlled force to the first ray which sought to eliminate some of the variables that occurred while using the Klaue device [27].
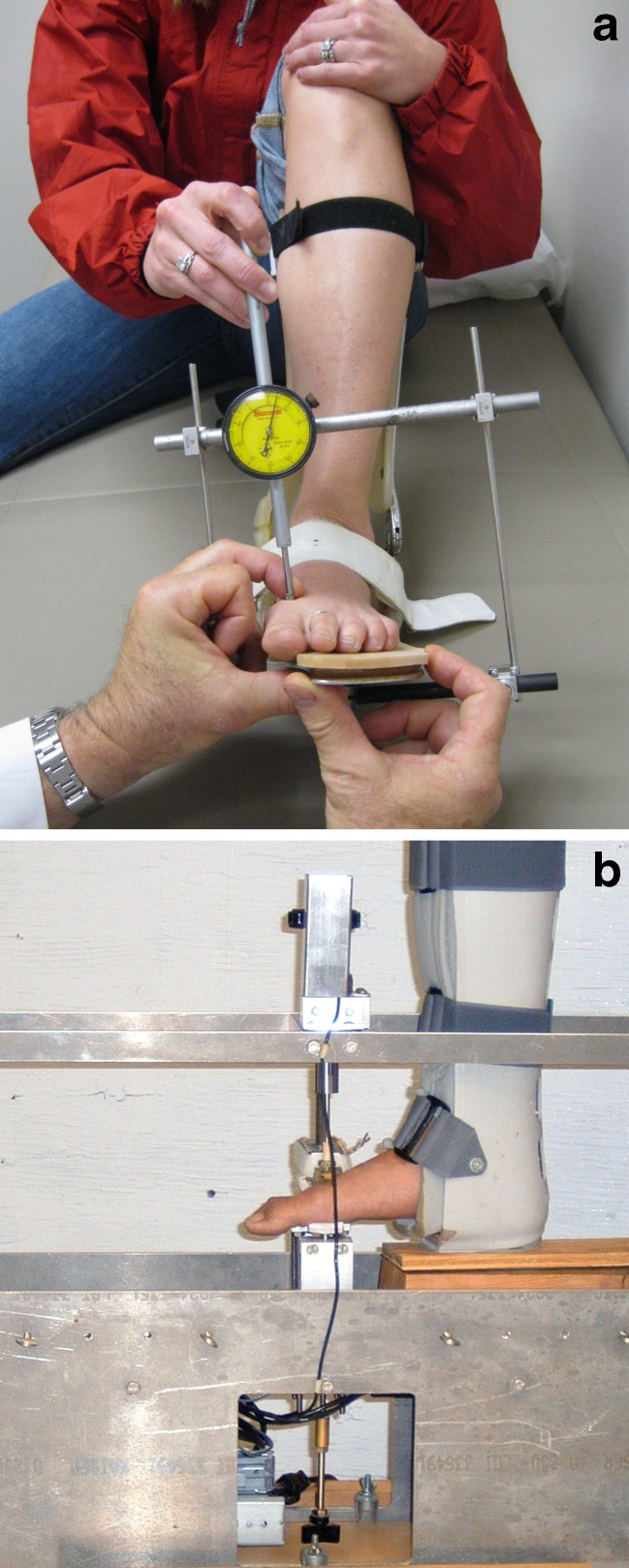
Fig. 3.
Devices used to measure first ray mobility. a The Klaue device, which uses manual pressure similar to the Morton manual exam. b Glasow device to measure first ray mobility using a measured force. (Courtesy of Ward Glasow, PhD)
Even with devices designed to quantify first ray mobility, studies have questioned the ability of an examiner to isolate first ray mobility to the metatarsocuneiform joint; upon careful review of these methods one can observe on radiographs that naviculocuneiform or talonavicular motion may also contribute to the overall first ray mobility [6, 9, 19, 20]. Klaue et al. [15] suggested an association between first ray hypermobility and hallux valgus, but a causal nature was not established. They hypothesized that first ray mobility stemmed from the first metatarsocuneiform joint and recommended a first metatarsocuneiform joint arthrodesis to correct the hallux valgus deformity and stabilize the first ray.
Clinical trials
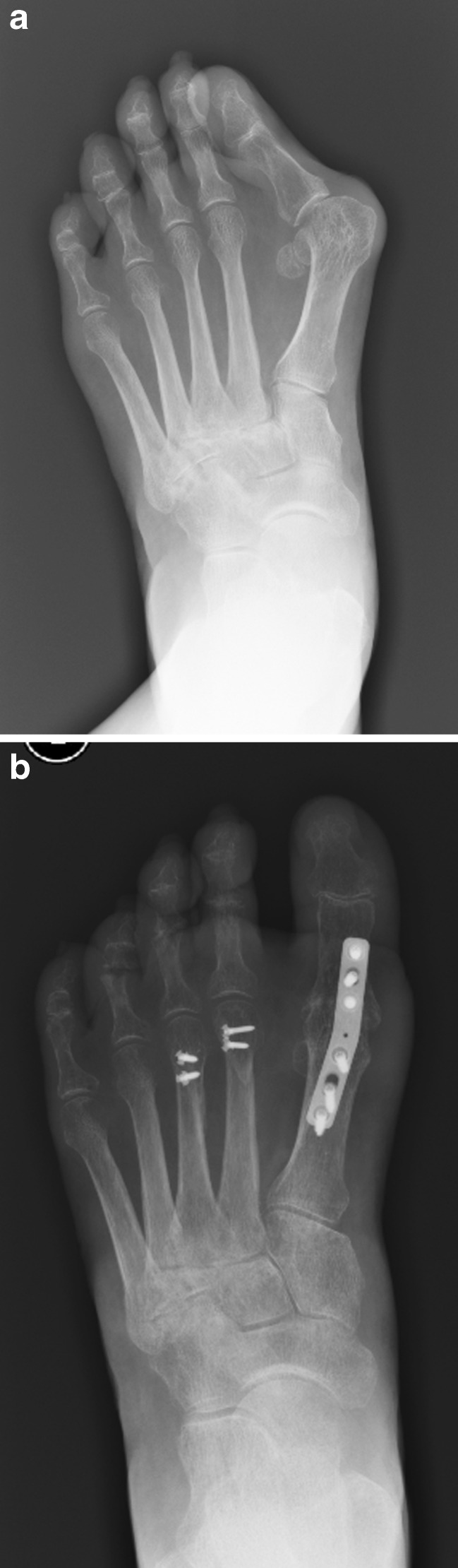
Multiple articles have attributed hallux valgus to increased mobility at the metatarsocuneiform joint without any objective data [14–16, 21, 23, 28, 29]. In those articles, the indication for a first metatarsocuneiform joint arthrodesis was a hallux valgus deformity with increased first ray mobility. Coughlin et al. [4] studied the effect of first metatarsophalangeal (MTP) joint arthrodesis for the treatment of severe idiopathic hallux valgus deformity. Sixteen patients (21 feet) were evaluated at an average of eight years of follow-up. The average correction of the 1–2 intermetatarsal angle was 6° (Fig. 4). Using the Klaue device, average postoperative sagittal translation measured 4 mm. No patients exhibited generalized ligamentous activity or increased first ray mobility. Two additional studies evaluating first MTP joint arthrodesis reported decreases of 8.2° and 5.6° in the 1–2 intermetatarsal angle while sparing the metatarsocuneiform joint from surgery [30–32]. Grimes and Coughlin [22] studied the effect of first MTP joint arthrodesis as a treatment of recurrent hallux valgus deformity. At an average follow-up of eight years, only two of 29 patients (7 %) demonstrated increased first ray mobility postoperatively. Both of these patients demonstrated generalized ligamentous laxity, but maintained excellent correction and reported high satisfaction scores at final follow-up.
Fig. 4.
Reduction of 1–2 intermetatarsal angle after first MTP joint arthrodesis. a Pre-operative radiograph demonstrating marked hallux valgus and widened 1–2 intermetatarsal (IM) angle. b Following metatarsophalangeal (MTP) joint arthrodesis, the IM angle has been diminished
Kim et al. [18] observed a significant postoperative decrease in first ray dorsiflexion mobility in hallux valgus patients treated with metatarsocuneiform joint sparing procedures. They evaluated 82 patients treated with a proximal metatarsal chevron osteotomy and distal soft tissue procedure and reported dorsoplantar mobility decreased from 6.8 mm to 3.2 mm at one year follow-up. Coughlin and Shurnas [7] investigated mobility of the first ray in men after a distal soft tissue procedure and proximal first metatarsal osteotomy, a procedure that spared the first metatarsocuneiform joint. The investigation began prior to the development of the Klaue device, and therefore, preoperative first ray mobility measurements were not recorded. Nevertheless, at six years follow-up, the mean first ray mobility was measured to be 4.9 mm, a value within the arbitrary-defined normal first ray mobility of less than 9 mm. Evaluation of mobility in the contralateral non-operative first ray demonstrated first ray mobility of 5.6 mm.
Coughlin et al. [5] further studied the effects of a distal-soft tissue procedure with a proximal first metatarsal osteotomy and its effect on first ray mobility in a large group of adult patients (127 feet). In this prospective study with an average 27-month follow-up, they reported a reduction in first ray mobility from 7.2 to 4.5 mm. In concordance with other reports, there was an association between the magnitude of first ray sagittal plane mobility and coronal plane deformity. However, this mobility was consistently diminished to a normal level following re-alignment procedures sparing the first metatarsocuneiform joint. The authors acknowledged that coronal mobility of the first metatarsocuneiform joint is necessary for the development of a hallux valgus deformity, yet re-establishment of the first ray alignment dramatically diminished the increased sagittal mobility. This led them to conclude that increased sagittal mobility was the result rather than the cause of the deformity. The question that remained for the authors was whether the significantly reduced mobility of the first ray was decreased at the time of surgery or over the ensuing two-year period of time prior to the final evaluation. Using cadaver specimens [6], Coughlin et al. then performed the identical surgical procedure (originally performed in the clinical prospective study) and compared pre-surgical and immediate post-surgical mobility of the first ray using the Klaue device. They reported a decrease in sagittal plane motion from 11.0 mm to 5.2 mm and demonstrated a relationship between the magnitude of pre-operative hallux valgus deformity and first ray mobility. This supported the notion that this mobility could be diminished with a surgical procedure sparing the metatarsocuneiform joint by realignment of the first ray. The authors suggested that the increased mobility was secondary to the hallux valgus deformity rather than the cause of the deformity.
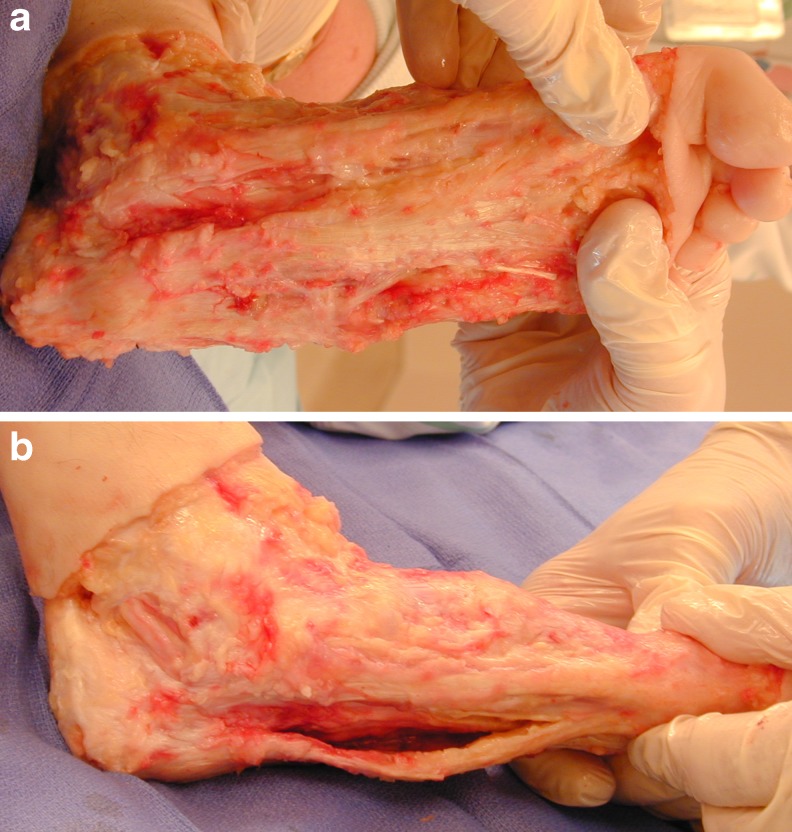
Soft tissue alignment
Rush et al. [33] used a metatarsal jig to evaluate the 1–2 intermetatarsal angle and first ray mobility. They demonstrated that increased first ray stability could be obtained by decreasing the 1–2 intermetatarsal angle. The authors attributed this to improved alignment of the hallux, sesamoids, and metatarsal, and therefore, more appropriate orientation of the plantar fascia and windlass mechanism. Sarrafian [34] also acknowledged the plantar aponeurosis as a critical component of first ray stability (Fig. 5a and b).
Fig. 5.
The plantar fascia plays a key role in stabilization of the first ray. a In a neutral ankle position, the fascia is tight. b With plantar flexion of the ankle, the fascia is quite relaxed or loose, having no stabilizing control of the first ray
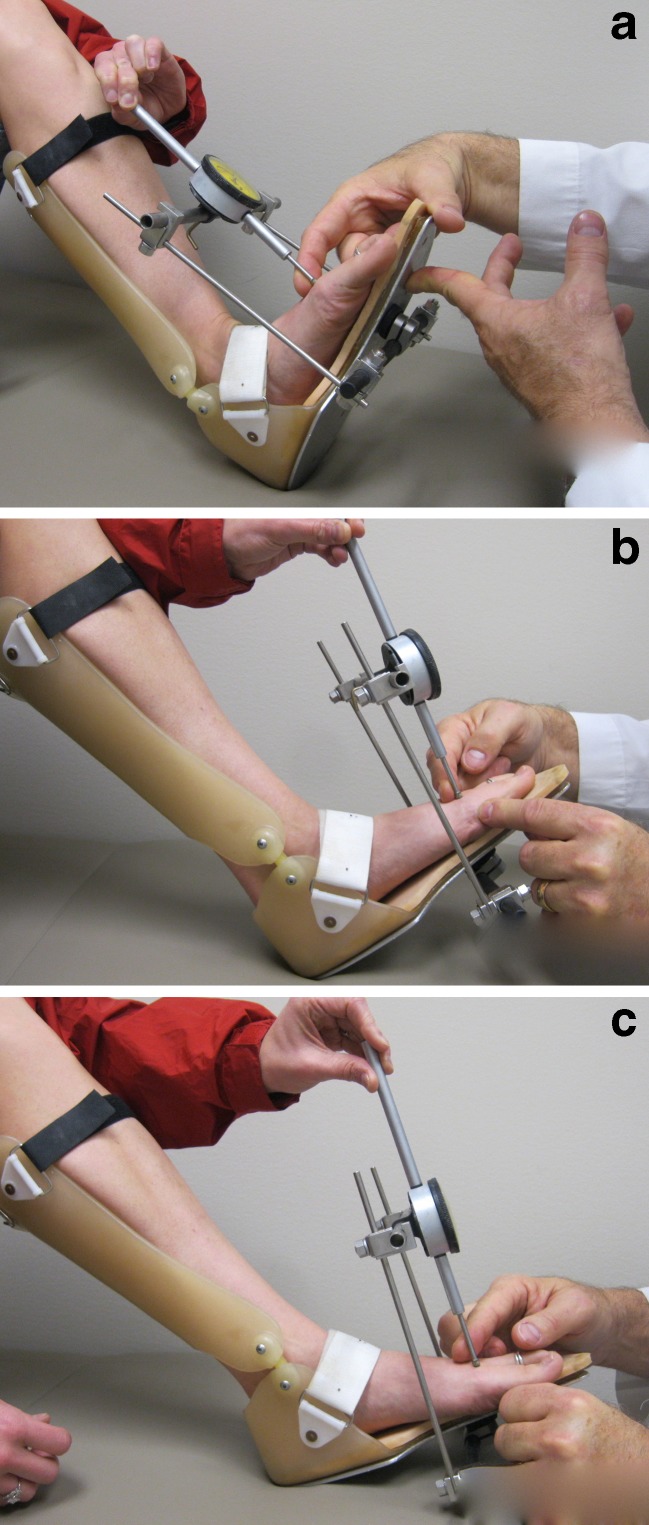
Grebing and Coughlin [35] evaluated the plantar fascia as it relates to first ray mobility and how first ray mobility is affected by ankle position. The authors demonstrated that sagittal plane mobility increased with ankle plantar flexion and decreased with ankle dorsiflexion. They used a modified Klaue device in which the position of the ankle joint was altered by placing the ankle in dorsiflexion, neutral position, or plantar flexion (Figs. 6a, b, and c). The authors quantified first ray motion in reference to variable ankle positions in a group of normal patients, a group of patients with untreated moderate to severe hallux valgus, a group who had undergone a successful metatarsophalangeal joint arthrodesis for hallux valgus, and a group of patients who had previously undergone a plantar fasciectomy for plantar fibromatosis. With the ankle in neutral position, the first ray motion averaged 4.9 mm for the control group, 7.0 mm for the hallux valgus group, 4.4 mm for the MTP fusion group, and 7.7 mm for the plantar fasciectomy group. There was a significant decrease in motion with ankle dorsiflexion in all four groups and a significant increase in motion with ankle plantar flexion in all groups except the fasciectomy group. The authors concluded that the plantar fascia is a key stabilizer of the first ray. Based on these observations, we believe that alignment confers stability, rather than instability leads to malalignment.
Fig. 6.
Device used to assess mobility with differing magnitude of ankle dorsiflexion. Modified Klaue device allowing different positions of the ankle while examining first ray mobility. a Dorsiflexion of ankle tightens the plantar fascia and reduces first ray mobility. b Neutral ankle position. c Plantar flexion of the ankle relaxes the plantar fascia leading to increased first ray mobility
Conclusion
The etiology of hallux valgus with regard to stability of the first metatarsocuneiform joint has historically been subject to much debate. Associations between the magnitude of the intermetatarsal angle and the hallux valgus angle have previously been established [5, 36]. We believe that metatarsocuneiform joint coronal plane mobility is necessary for a concomitant increase in both of these angles. Although metatarsocuneiform joint hypermobility has been implicated in the development of a hallux valgus deformity, isolated sagittal plane instability has thus far not been proven to be a definitive cause. Likewise, it has not been proven that first ray “hypermobility” is itself a pathologic entity. Van Beek and Greisberg [37] recently noted that we must first define the measures of mobility and then apply them to large populations before the notion of hypermobility is properly defined.
Multiple reports confirm that distal realignment procedures sparing the metatarsocuneiform joint will lead to a reduction of first ray mobility [4–7, 18]. The mobility of the first ray relies on more than just static restraints, and soft tissue alignment plays an important role. As a hallux valgus deformity develops, the dynamic restraints, including the plantar aponeurosis, sesamoids, and intrinsic musculature become compromised and malaligned [33, 34]. While the metatarsocuneiform joint is critical to the development of hallux valgus, it is for different reasons than those envisioned by Lapidus [1–3] and others [15, 21, 28, 38]. These historical theories were based on unreliable methods by which to quantify mobility. Metatarsocuneiform joint mobility may be necessary for a hallux valgus deformity to develop; however, “hypermobility” may not be the cause but rather the result of a hallux valgus deformity.
Acknowledgments
Conflict of interest
The authors declare they have no conflict of interest.
Contributor Information
Jesse F. Doty, Phone: +1-901-4821848, FAX: +1-423-7785994, Email: jessd90@hotmail.com
Michael J. Coughlin, Phone: +1-208-3673330, FAX: +1-208-3673331, Email: thefootmd@gmail.com
References
- 1.Lapidus PW. Operative correction of metatarsus varus primus in hallux valgus. Surg Gynecol Obstet. 1934;58:183–191. [Google Scholar]
- 2.Lapidus PW. A quarter of a century of experience with the operative correction of the metatarsus varus primus in hallux valgus. Bull Hosp Joint Dis. 1956;17(2):404–421. [PubMed] [Google Scholar]
- 3.Lapidus PW. The author’s bunion operation from 1931 to 1959. Clin Orthop. 1960;16:119–135. [PubMed] [Google Scholar]
- 4.Coughlin MJ, Grebing BR, Jones CP. Arthrodesis of the first metatarsophalangeal joint for idiopathic hallux valgus: intermediate results. Foot Ankle Int. 2005;26(10):783–792. doi: 10.1177/107110070502601001. [DOI] [PubMed] [Google Scholar]
- 5.Coughlin MJ, Jones CP. Hallux valgus and first ray mobility. A prospective study. J Bone Joint Surg Am. 2007;89(9):1887–1898. doi: 10.2106/JBJS.F.01139. [DOI] [PubMed] [Google Scholar]
- 6.Coughlin MJ, Jones CP, Viladot R, Glano P, Grebing BR, Kennedy MJ, Shurnas PS, Alvarez F. Hallux valgus and first ray mobility: a cadaveric study. Foot Ankle Int. 2004;25(8):537–544. doi: 10.1177/107110070402500805. [DOI] [PubMed] [Google Scholar]
- 7.Coughlin MJ, Shurnas PS. Hallux valgus in men. Part II: first ray mobility after bunionectomy and factors associated with hallux valgus deformity. Foot Ankle Int. 2003;24(1):73–78. doi: 10.1177/107110070302400112. [DOI] [PubMed] [Google Scholar]
- 8.Grebing BR, Coughlin MJ. Evaluation of Morton’s theory of second metatarsal hypertrophy. J Bone Joint Surg Am. 2004;86-A(7):1375–1386. doi: 10.2106/00004623-200407000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Jones CP, Coughlin MJ, Pierce-Villadot R, Golano P, Kennedy MP, Shurnas PS, Grebing BR, Teachout L. The validity and reliability of the Klaue device. Foot Ankle Int. 2005;26(11):951–956. doi: 10.1177/107110070502601110. [DOI] [PubMed] [Google Scholar]
- 10.Morton D (1935) The human foot. Columbia University Press, New York
- 11.Morton D. Significant characteristics of the Neanderthal foot. Nat History. 1926;26:310–314. [Google Scholar]
- 12.Morton DJ. Hypermobility of the first metatarsal bone: the interlinking factor between matarsalgia and longitudinal arch strains. J Bone Joint Surg. 1928;10:187–196. [Google Scholar]
- 13.Barnicot NA, Hardy RH. The position of the hallux in West Africans. J Anat. 1955;89(3):355–361. [PMC free article] [PubMed] [Google Scholar]
- 14.Faber FW, Mulder PG, Verhaar JA. Role of first ray hypermobility in the outcome of the Hohmann and the Lapidus procedure. A prospective, randomized trial involving one hundred and one feet. J Bone Joint Surg Am. 2004;86-A(3):486–495. doi: 10.2106/00004623-200403000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Klaue K, Hansen ST, Masquelet AC. Clinical, quantitative assessment of first tarsometatarsal mobility in the sagittal plane and its relation to hallux valgus deformity. Foot Ankle Int. 1994;15(1):9–13. doi: 10.1177/107110079401500103. [DOI] [PubMed] [Google Scholar]
- 16.Lee KT, Young K. Measurement of first-ray mobility in normal vs. hallux valgus patients. Foot Ankle Int. 2001;22(12):960–964. doi: 10.1177/107110070102201206. [DOI] [PubMed] [Google Scholar]
- 17.Voellmicke KV, Deland JT. Manual examination technique to assess dorsal instability of the first ray. Foot Ankle Int. 2002;23(11):1040–1041. doi: 10.1177/107110070202301113. [DOI] [PubMed] [Google Scholar]
- 18.Kim JY, Park JS, Hwang SK, Young KW, Sung IH. Mobility changes of the first ray after hallux valgus surgery: clinical results after proximal metatarsal chevron osteotomy and distal soft tissue procedure. Foot Ankle Int. 2008;29(5):468–472. doi: 10.3113/FAI.2008.0468. [DOI] [PubMed] [Google Scholar]
- 19.Whittaker EC, Aubin PM, Ledoux WR. Foot bone kinematics as measured in a cadaveric robotic gait simulator. Gait Posture. 2011;33(4):645–650. doi: 10.1016/j.gaitpost.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 20.Faber FW, Kleinrensink GJ, Verhoog MW, Vijn AH, Snijders CJ, Mulder PG, Verhaar JA. Mobility of the first tarsometatarsal joint in relation to hallux valgus deformity: anatomical and biomechanical aspects. Foot Ankle Int. 1999;20(10):651–656. doi: 10.1177/107110079902001007. [DOI] [PubMed] [Google Scholar]
- 21.Sangeorzan BJ, Hansen ST., Jr Modified Lapidus procedure for hallux valgus. Foot Ankle. 1989;9(6):262–266. doi: 10.1177/107110078900900602. [DOI] [PubMed] [Google Scholar]
- 22.Grimes JS, Coughlin MJ. First metatarsophalangeal joint arthrodesis as a treatment for failed hallux valgus surgery. Foot Ankle Int. 2006;27(11):887–893. doi: 10.1177/107110070602701104. [DOI] [PubMed] [Google Scholar]
- 23.Hansen ST., Jr Hallux valgus surgery. Morton and Lapidus were right! Clin Podiatr Med Surg. 1996;13(3):347–354. [PubMed] [Google Scholar]
- 24.Coetzee JC, Resig SG, Kuskowski M, Saleh KJ. The Lapidus procedure as salvage after failed surgical treatment of hallux valgus: a prospective cohort study. J Bone Joint Surg Am. 2003;85-A(1):60–65. doi: 10.2106/00004623-200301000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Glasoe WM, Allen MK, Saltzman CL, Ludewig PM, Sublett SH. Comparison of two methods used to assess first-ray mobility. Foot Ankle Int. 2002;23(3):248–252. doi: 10.1177/107110070202300310. [DOI] [PubMed] [Google Scholar]
- 26.Glasoe WM, Yack HJ, Saltzman CL. Measuring first ray mobility with a new device. Arch Phys Med Rehabil. 1999;80(1):122–124. doi: 10.1016/S0003-9993(99)90320-9. [DOI] [PubMed] [Google Scholar]
- 27.Glasoe WM, Grebing BR, Beck S, Coughlin MJ, Saltzman CL. A comparison of device measures of dorsal first ray mobility. Foot Ankle Int. 2005;26(11):957–961. doi: 10.1177/107110070502601111. [DOI] [PubMed] [Google Scholar]
- 28.Bednarz PA, Manoli A., 2nd Modified lapidus procedure for the treatment of hypermobile hallux valgus. Foot Ankle Int. 2000;21(10):816–821. doi: 10.1177/107110070002101004. [DOI] [PubMed] [Google Scholar]
- 29.Clark HR, Veith RG, Hansen ST., Jr Adolescent bunions treated by the modified Lapidus procedure. Bull Hosp Jt Dis Orthop Inst. 1987;47(2):109–122. [PubMed] [Google Scholar]
- 30.Cronin JJ, Limbers JP, Kutty S, Stephens MM. Intermetatarsal angle after first metatarsophalangeal joint arthrodesis for hallux valgus. Foot Ankle Int. 2006;27(2):104–109. doi: 10.1177/107110070602700206. [DOI] [PubMed] [Google Scholar]
- 31.Humbert JL, Bourbonniere C, Laurin CA. Metatarsophalangeal fusion for hallux valgus: indications and effect on the first metatarsal ray. Can Med Assoc J. 1979;120(8):937–941. [PMC free article] [PubMed] [Google Scholar]
- 32.Mann RA, Katcherian DA. Relationship of metatarsophalangeal joint fusion on the intermetatarsal angle. Foot Ankle. 1989;10(1):8–11. doi: 10.1177/107110078901000102. [DOI] [PubMed] [Google Scholar]
- 33.Rush SM, Christensen JC, Johnson CH. Biomechanics of the first ray. Part II: metatarsus primus varus as a cause of hypermobility. A three-dimensional kinematic analysis in a cadaver model. J Foot Ankle Surg. 2000;39(2):68–77. doi: 10.1016/S1067-2516(00)80030-7. [DOI] [PubMed] [Google Scholar]
- 34.Sarrafian SK. Functional characteristics of the foot and plantar aponeurosis under tibiotalar loading. Foot Ankle. 1987;8(1):4–18. doi: 10.1177/107110078700800103. [DOI] [PubMed] [Google Scholar]
- 35.Grebing BR, Coughlin MJ. The effect of ankle position on the exam for first ray mobility. Foot Ankle Int. 2004;25(7):467–475. doi: 10.1177/107110070402500705. [DOI] [PubMed] [Google Scholar]
- 36.Hardy RH, Clapham JC. Observations on hallux valgus; based on a controlled series. J Bone Joint Surg Br. 1951;33-B(3):376–391. doi: 10.1302/0301-620X.33B3.376. [DOI] [PubMed] [Google Scholar]
- 37.Van Beek C, Greisberg J. Mobility of the first ray: review article. Foot Ankle Int. 2011;32(9):917–922. doi: 10.3113/FAI.2011.0917. [DOI] [PubMed] [Google Scholar]
- 38.Harris RI, Beath T. Hypermobile flat-foot with short tendo achillis. J Bone Joint Surg Am. 1948;30A(1):116–140. [PubMed] [Google Scholar]