Abstract
Objective
To investigate the effect on pain reduction and strengthening of the whole body vibration (WBV) in chronic knee osteoarthritis (OA).
Methods
Patients were randomly divided into two groups: the study group (WBV with home based exercise) and control group (home based exercise only). They performed exercise and training for 8 weeks. Eleven patients in each group completed the study. Pain intensity was measured with the Numeric Rating Scale (NRS), functional scales were measured with Korean Western Ontario McMaster score (KWOMAC) and Lysholm Scoring Scale (LSS), quadriceps strength was measured with isokinetic torque and isometric torque and dynamic balance was measured with the Biodex Stability System. These measurements were performed before training, at 1 month after training and at 2 months after training.
Results
NRS was significantly decreased in each group, and change of pain intensity was significantly larger in the study group than in the control group after treatment. Functional improvements in KWOMAC and LSS were found in both groups, but no significant differences between the groups after treatment. Dynamic balance, isokinetic strength of right quadriceps and isometric strengths of both quadriceps muscles improved in both groups, but no significant differences between the groups after treatment. Isokinetic strength of left quadriceps did not improve in both groups after treatment.
Conclusion
In chronic knee OA patients, WBV reduced pain intensity and increased strength of the right quadriceps and dynamic balance performance. In comparison with the home based exercise program, WBV was superior only in pain reduction and similarly effective in strengthening of the quadriceps muscle and balance improvement.
Keywords: Knee, Muscle strength, Osteoarthritis, Pain, Vibration
INTRODUCTION
Knee osteoarthritis (OA) is the most common type of OA, with an estimated 12.1% of adults in the United States suffering from pain and functional limitations [1]. Knee OA is commonly defined as a degenerative, noninfectious disease of the knee joint. The main symptoms of OA are stiffness, loss of mobility, swelling, and pain.
No curative agent has been known in treatment of OA. The primary goals for OA therapy are pain relief, maintenance of joint integrity, improvement in functional status, as well as lessening deformity and instability [2]. The American College of Rheumatology (ACR) guidelines recommend a combination of non-pharmacological and pharmacologic treatments for symptomatic knee OA and conservative management plans must be individualized and adjusted according to the responses of patients [3]. Non-pharmacological treatments, such as active modalities and physical agents effectiveness in reducing pain and disability, as well as improving quality of life without side effects in chronic knee OA patients [3,4]. In addition, physical agents, such as short-wave diathermy, transcutaneous electrical nerve stimulation (TENS), ultrasound, and hot packs are passive; non-invasive and safe modalities commonly used to control both acute and chronic pain [7].
The muscles around the knee, especially quadriceps and hamstring, are known to act as dynamic stabilizer and also as stabilization of the posture and even distribution of shock and the stress during the physical motion [5]. Quadriceps muscle weakness is a common clinical sign associated with tibiofemoral OA [6], and is considered to be a critical determinant of disability [7]. Loss of hyaline articular cartilage and impairment of bony remodeling can even result in capsular damage and muscle weakness [8], and impairment of knee proprioception has consistently been related to individuals with knee OA [9]. ACR guideline recommends strengthening exercise of the quadriceps [3]. Weakness of knee flexor and extensor muscles could lead to a decreased joint stability and be combined with the associated decreased biomechanical efficiency. Thus, we need an effective modality for pain relief and also muscle strengthening.
The whole body vibration (WBV) machinery and tools has recently been paid attention to because it seems to be easy and safe to perform. Ultrasound makes the platform to vibrate precisely vertically, which induces involuntary muscle contractions of the whole body. Various studies regarding application of WBV reported improvement of muscle strength, power, joint proprioception, balance, and flexibility [10-13]. Some studies reported its effects of especially quadriceps strengthening [10-13]. Improvements are thought to be due to reflex activation of the a-motor neuron, via muscle spindle activation [14]. The WBV exercise is a time-saving and safe method for rehabilitation of women with knee OA [15]. WBV could be thought as a useful modality in the patients who are unable to participate in active modalities because of severe disability according to advancing age and progression of knee OA.
This study was conducted to investigate the therapeutic effects, such as pain reduction and strengthening, and safety of WBV in chronic knee OA.
MATERIALS AND METHODS
Subjects and study design
Forty-four female ambulatory community-based patients were recruited with a diagnosis of chronic knee OA. Inclusion criteria of subjects were age at least or above 50 years, diagnosed as symptomatic knee OA for at least 6 months according to the clinical criteria of the ACR [3], and radiographic findings compatible with knee OA and Kellgren-Lawrence grades II and III in simple X-ray [16]. Further, patients had no previous history of serious knee trauma, surgery and arthroplasty, or intra-articular injection of hyaluronic acid or steroid in the last 6 months. Exclusion criteria were acute symptomatic OA, comorbidities such as any peripheral or central neurologic disorders, and previous surgery of knee during the last 6 months, and radiologic findings of Kellgren-Lawrence grade IV. Informed consents were obtained from all patients. Forty-four patients were randomized into two groups using the blocked randomization method. Eight patients (study group, 5; control group, 3) were excluded at screening due to severe OA on radiologic findings. Patients in the study group (n=17; mean age, 60.0±5.7 years) received WBV (20 minutes, 3 times every week) with home based exercise (HBE) and those in the control group (n=19; mean age, 62.5±6.2 years) performed only HBE after education for 8 weeks. During the training period, fourteen patients dropped out (study group, 8; control group, 6) because of personal business and tiresomeness, herpes zoster, low back pain, and knee pain aggravation. Finally, eleven patients finished training for 2 months in each group.
Out of 22 patients of the control group, only one patient was on aspirin (Astrix 100 mg/day) due to underlying heart disease. Other patients were not on analgesic drugs, such as non-steroidal anti-inflammatory drugs, and during the study, such medication was not given. Also, during the study period, no other treatments, such as physical modalities (e.g., short-wave diathermy, TENS, ultrasound, and hot packs, etc.) nor injection technique was done to the patients, except for the HBE and WBV. Various measurements were performed before training, at 1 month after training, and at 2 months after training. Pain intensity was measured with the Numeric Rating Scale (NRS), functional scores of pain with Korean Western Ontario McMaster score (KWOMAC) and Lysholm Scoring Scale (LSS). The strength of the quadriceps muscle was measured with isokinetic peak torque (at 60°/sec), isometric torque and dynamic balance were measured. Information of clinical characteristics, such as age, height, body weight, Kellgren-Lawrence system, and body mass index were collected.
All study designs were approved by the Institutional Review Board of our institution.
Intervention
Whole body vibration training
WBV training was performed with TurboSonic (TS Korea Co., Ltd, Seoul, Korea). The patients were asked to stand barefoot on the platform with a slight knee flexion during training. To prevent the feeling of uncomfort and anxiety, the patient can hold a handle during training. The training of WBV was performed for 20 minutes and over three times a week for 8 weeks. During training of one set, patients were instructed to perform 2 training cycles of 10 minutes, and rest of 5 minutes between cycles. Vibration was delivered at a low frequency (12-14 Hz) with a vertical displacement of 2.5-5 mm (Fig. 1).
Fig. 1.

A woman stands on the vibrating platform of whole body vibration (TurboSonic) with a slight flexion of both knees.
Home based exercise
HBE consists of five exercise programs. The exercise protocol consisted of active range-of-motion exercises, muscle strengthening, and muscle stretching. The protocol was based on increasing muscle strength, and facilitation techniques are used for improving the proprioceptive, flexibility, and range of motion. The first session included a lecture that provided information about knee OA, its risk factors and information on the importance of regular exercise. The protocol for exercises was presented to patients for practice [17]. Most of the exercises prescribed can be incorporated into daily life; for example, while sitting on a chair, patients were instructed to slowly straighten their leg out in front of them for each leg. The patients were asked to perform each exercise up to 10 times each. Each patient received a detailed handout containing instructions and photographs of the exercises. Patients will attend HBE sessions over 3 times a week for eight weeks. Patients were instructed that pain should be avoided in all exercises.
Outcome measurements
Pain intensity
Pain intensity was measured with NRS.
Functional status
Functional status of patients with knee OA evaluated using KWOMAC and LSS. KWOMAC is a modified Korean version of WOMAC [18]. KWOMAC is a set of standardized questionnaires used by health professionals to evaluate the condition of patients with OA of the knee and hip. KWOMAC consists of 24 questionnaires, which compose 3 sub-concepts, such as pain, joint stiffness, and functional status. KWOMAC scores range from 0 to 96, with higher scores indicating severe OA.
LSS consists of 8 questionnaires with contents of pain, clinical symptom and functional status. LSS scores range from 0 to 100, with lower scores indicating severe OA.
Muscle strength
Maximal isokinetic torque: The maximal voluntary knee extensor strength was measured as isokinetic peak torque with an isokinetic dynamometer (model 900-240; Biodex Medical Systems, Shirley, NY, USA). The patient was tested in a seated position with the hip at 90° of flexion, and strapping was placed across the waist and chest to stabilize the torso. The axis of rotation of the dynamometer lever arm was aligned to the femoral lateral condyle, and the lever arm was secured to the tibia just proximal to the medial malleolus via an ankle cuff.
Following a warm-up comprising 1 submaximal and 1 maximal contraction, all of the patients performed 2 maximal trials for 5 seconds with a 1-minute rest interval. Patients were instructed to extend their knee as fast and forcefully as possible for at least 2 to 3 seconds. In each trial, the peak torque normalized to the patient's body mass was recorded, and the higher measurement of 2 valid trials was analyzed.
Maximal isometric torque
Following one submaximal trial contraction, two maximal isometric knee-extensions were performed at knee angles of 60°. Maximal contractions were interspersed by 90-second rest intervals. The highest isometric extension torque of the manually smoothed curves at each knee angle was selected as the maximal isometric torque.
Dynamic balance
Standing balance control scores were acquired from Biodex Stability System (Biodex Medical Systems). The platform is connected to computer software (ver. 3.1, Biodex Medical Systems) that enables the device to measure the balance objectively. Patients were instructed to stand barefoot on the platform with a slight knee flexion and attached to the feet on the platform. Before the start of the stability trials, the subjects were asked to maintain a quiet stance on the platform for seconds for initialization. During that time, center of pressure were assessed. Immediately after the quiet stance, 6 stability trials (3 trials per each state) were performed 30 seconds during opening of the eyes. The device measured and analyzed the medial-lateral (ML) index and anterior-posterior (AP) index as the mean±standard deviation. ML index represents the stability of the coronal plane and AP index represents the stability of the sagittal plane.
Data analysis and statistics
To investigate and compare the changes of each outcome at each period (baseline, 1 month after treatment, and 2 months after treatment) in each group, and to compare the changes between the study group and control group, analysis with repeated measures analysis of variance (RMANOVA) was performed. To test significant differences from the baseline at each time (1 month and 2 months) and to test the significance of the time effect for each group, linear contrasts were performed. The statistical significance level was determined as p-value <0.05. All outputs were produced using a statistical software package SAS ver. 9.3 (SAS Institute Inc., Cary, NC, USA).
RESULTS
The clinical characteristics of patients, such as age, height, body weight, Kellgren-Lawrence grade and body mass index are described and there were no statistical differences between the study group and control group at baseline (Table 1).
Table 1.
Clinical characteristics of the subjects
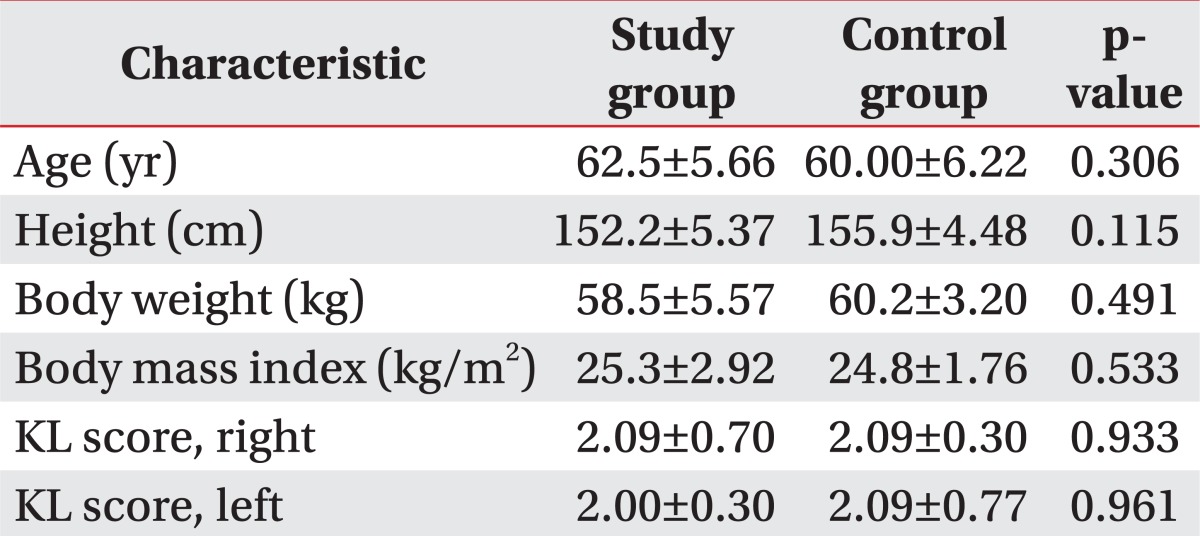
Values are presented as mean±standard deviation.
KL score, Kellgren-Lawrence system score.
Many parameters were measured and analyzed to investigate the change during training in each group and to compare the difference of change during training between the study group and control group.
Pain intensity (NRS) of knee pain significantly decreased after training in each group and the decrease of pain intensity was significantly more in the study group than the control group at 2 months after training (Table 2).
Table 2.
Pain intensity (Numeric Rating Scale) of knee
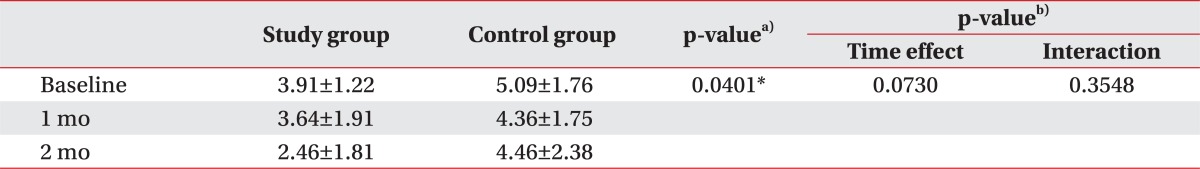
Values are presented as mean±standard deviation.
Time effect, the difference between subjects of each group according to the change of time; Interaction, for analytic significant interaction between time and group.
a)p-value between-subject effects from repeated measures analysis of variance (RMANOVA). b)p-value within-subject effects from RMANOVA. *p<0.05.
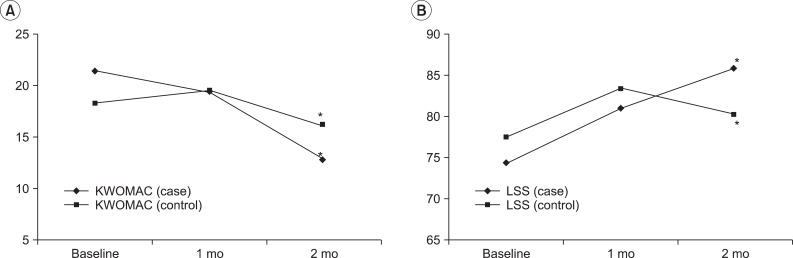
RMANOVA analysis revealed that the overall change of pain related physical functions, such as KWOMAC, and LSS after training were not significantly different between the study and control groups (Table 3). An analysis using linear contrast revealed that KWOMAC was significantly improved in both groups at 2 months in comparison with the baseline (p=0.035, from analysis using contrast for test between 2 months and the baseline), but there was no significant difference between the study group and control group during the training period. Further, LSS improved significantly from the baseline to 2 months (p=0.038, from analysis using contrast for test between 2 months and the baseline) and there was no statistical difference between the study group and control group (Fig. 2).
Table 3.
Change of physical functions
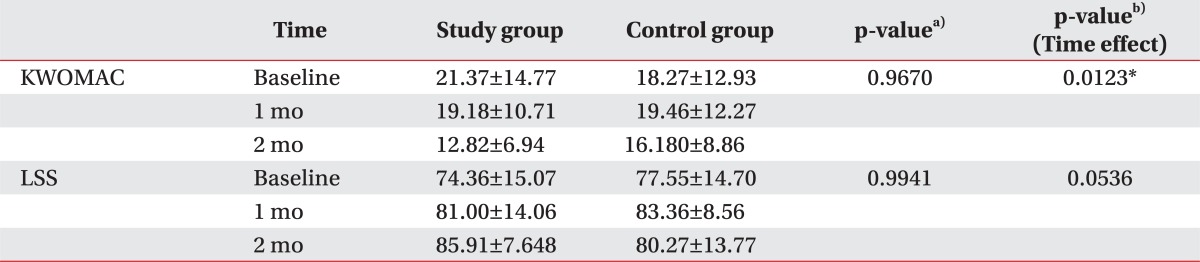
Values are presented as mean±standard deviation.
KWOMAC, Korean Western Ontario McMaster score; LSS, Lysholm Scoring Scale; Time effect, the difference between subjects of each group according to the change of time.
a)p-value between-subject effects from repeated measures analysis of variance (RMANOVA). b)p-value within-subject effects from RMANOVA (time effect). *p<0.05.
Fig. 2.
The graph shows changes in physical function over time. The changes of (A) Korean Western Ontario McMaster score (KWOMAC) and (B) Lysholm Scoring Scale (LSS) were significantly different between baseline and 2 months in both groups. But there was no significant differences study between study group and control group. Asterisk (*) indicates statistical significance between baseline and 2 months (p<0.05).
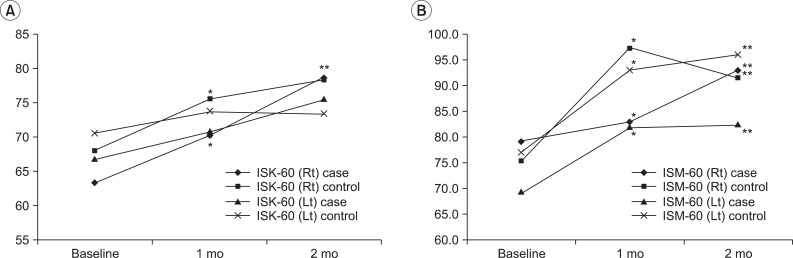
RMANOVA revealed that the overall change of isokinetic torque and isometric torque were not significantly different between WBV and HBE during 2 months (Table 4). The strengthening effect of WBV might be similar to HBE. An analysis using linear contrast revealed that isokinetic torque at 60°/sec of right knee extensor significantly improved in both groups during the training period (p=0.0175, from analysis using contrast for test between 1 month and the baseline; p<0.0001, from analysis using contrast for test between 2 months and the baseline), but there was no significant difference between the study group and control group. Isokinetic torque of left knee extensor improved, but not significant between each time and baseline in both groups. Isokinetic torque improved only in right knee extensor in both groups (Fig. 3A). Isometric torque of both knee extensors significantly increased at 1 month (p=0.0146 for right knee extensor and p=0.0039 for left knee extensor, from analysis using contrast for test between 1 month and the baseline) and at 2 months (p=0.0013 for right knee extensor and p=0.0001 for left knee extensor, from analysis using contrast for test between 2 months and the baseline), but there was no significant difference between the study group and control group (Fig. 3B).
Table 4.
Change in muscle strength
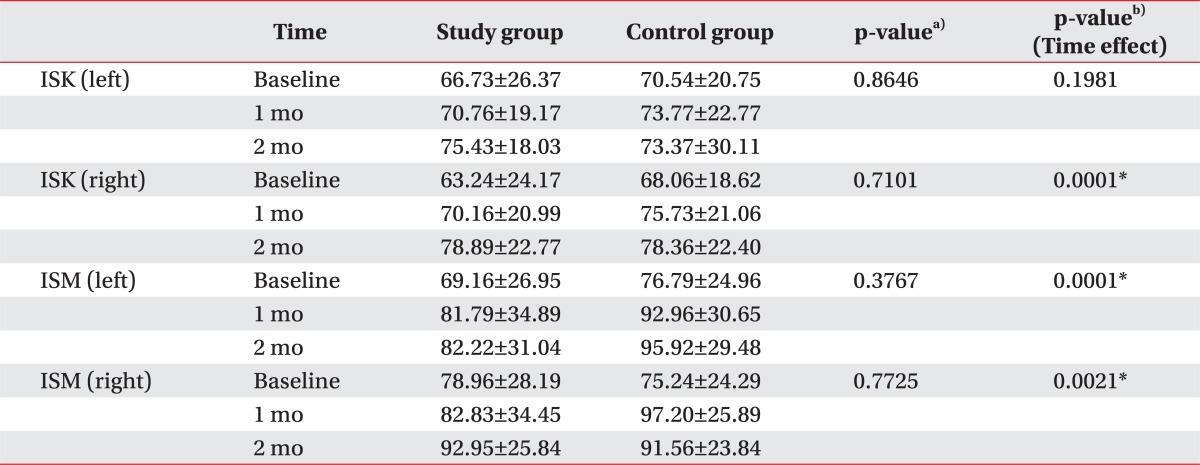
Values are presented as mean±standard deviation.
Time effect, the difference between subjects of each group according to the change of time; ISK, isokinetic torque of knee extensor (angular velocity, 60°); ISM, isometric torque of knee extensor.
a)p-value between-subject effects from repeated measures analysis of variance (RMANOVA). b)p-value within-subject effects from RMANOVA (time effect). *p<0.05.
Fig. 3.
The graph shows changes of knee extensor muscle strength: (A) isokinetic torque (60°/sec) and (B) isometric torque in both groups. (A) Isokinetic torques of right knee extensor increased significantly over time during training period in both groups and there were no significant differences between study group and control group. Isokinetic torques of left knee extensor was not significantly different during training period in each group and between groups. (B) Isometric torques of both knee extensors increased significantly over time during training period and there were no significant differences between groups during training period. Asterisk (*) indicates statistical significance between baseline and 1 month (p<0.05) and double asterisk (**) indicates statistical significance between baseline and 2 months. ISK, isokinetic; ISM, isometric; Rt, right; Lt, left.
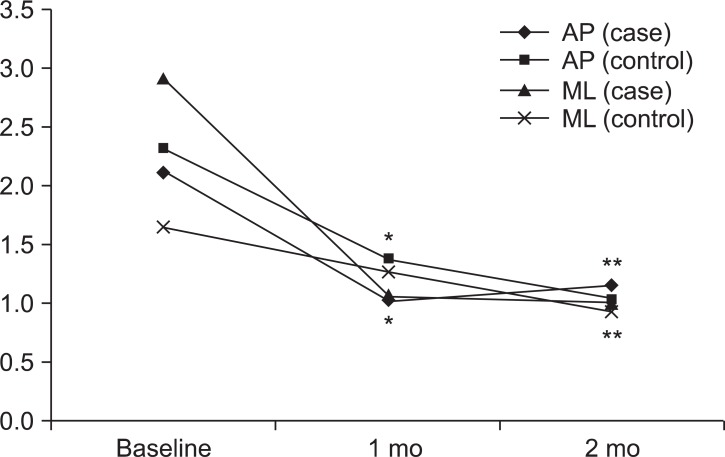
The effects on dynamic balance were not significantly different between the study group and control group (Table 5). AP index and ML index significantly improved at 1 month (p=0.0222 in AP index and p=0.0255 in ML index, from analysis using contrast for test between 1 month and the baseline) and at 2 months (p=0.0081 in AP index and p=0.0022 in ML index, from analysis using contrast for test between 2 months and the baseline) from the baseline in both groups, but there were no significant difference between 1 and 2 months in each group and no difference between the groups at each time. Dynamic balance after WBV significantly improved, but not significantly different with that after HBE (Fig. 4).
Table 5.
Change in dynamic balance
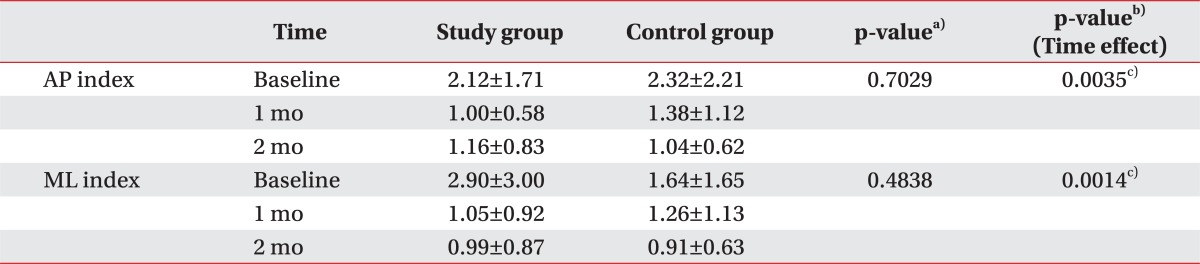
Values are presented as mean±standard deviation.
AP, anterior-posterior; ML, medial-lateral; Time effect, the difference between subjects of each group according to the change of time.
a)p-value between-subject effects from repeated measures analysis of variance (RMANOVA). b)p-value within-subject effects from RMANOVA (time effect). c)Significant differences (p<0.05) are identified. *p<0.05.
Fig. 4.
The graph shows changes in dynamic balance over time in both groups. Anterior-posterior (AP) index and medial-lateral (ML) index significantly improved at 1 month and 2 months, respectively, but there was no significant difference between study group and control group. Asterisk (*) indicates statistical significance between baseline and 1 month (p<0.05) and double asterisk (**) indicates statistical significance between baseline and 2 months (p<0.05).
DISCUSSION
WBV has been reported that low-amplitude, low frequency mechanical vibration is a safe and effective method to improve muscle strength [19-21]. Vibration exercise imposes hyper-gravity activity due to the high accelerations. While mechanical vibration applied to the muscle, fast and short changes occurred in the length of the muscle-tendon complex in skeletal muscles [22]. Vibrations elicit a response called "tonic vibration reflex". It was produced by mechanical activation of muscle spindles, mediation of the neural signals by Ia afferents, and activation of muscle fibers via large α-motor neurons [23]. Tonic vibration reflex is increased in recruitment of the motor units through activation of the muscle spindles and polysynaptic pathways [24]. WBV induced a more efficient use of the positive proprioceptive feedback loop [19-21,24]. This mechanism showed that the principle of the WBV-exercise regime increased muscle strength and proprioception.
Many studies were reported that WBV training improved neuromuscular performance in healthy people and along with other diseases [10-15]. Trans et al. [15] recently reported the effect of WBV exercise on muscle strength and proprioception in females with knee OA. This study compared WBV exercise with the control group who did not participate in any training. It showed that the WBV-exercise regime increased muscle strength and proprioception.
TurboSonic WBV used in this study produces vibration from an ultrasound, which can deliver an extremely low frequency vibration to the whole body. This advantage means that vibration is effectively propagated to the knee joint in standing position. In addition, the intensity of vibration can be adjusted to each individual patient to minimize discomforts and hazards. The target of the device could be the improvements proprioception of the knee joints and strengthening of knee extensor, as well as optimization of neuronal reactivation of the muscles and thereby, improved joint stability. We supposed that the TurboSonic WBV can be a safe and effective treatment intervention for strengthening of knee extensor and improvement of dynamic balance in patients with knee OA.
This study investigated the effects of WBV training on pain, dynamic balance, muscle strength and functional capacity for 2 months in mild to moderate knee OA patients. The analyses showed that the effects of WBV on pain reduction and improvement of pain related functions and also on strengthening of knee extensor and improvement of dynamic balance control as expected. However statistical analysis revealed these effects of WBV was not superior to those of the HBE except pain reduction.
The results of this study show that therapeutic effect of WBV was similar to the HBE except pain reduction, which was only superior in the WBV group. Pain reduction is essential to the functional disability in knee OA. However, the mechanism of pain reduction is not clear. We supposed that the WBV could influence slowly adapting receptors (Meissner corpuscles) [25,26]. The reductions of pain may result from a desensitization of Meissner corpuscles and Merkel cell that occurs after low frequency vibration [27]. Locally applied skin vibration can result in a reversible decrement in vibro-tactile afferent sensitivity, and it is thought that the threshold sensitivity of these afferents increases with frequency and amplitude [28,29]. Further, we suggested that repeated WBV stimulation increasing influence of the afferent threshold sensitivity. To our knowledge this is the first study to investigate the impact of WBV on decreased pain in females with knee OA.
The change of KWOMAC and LSS representing physical disability was not significantly different between WBV and HBEs. KWOMAC showed no significant change over 1 month in both groups, and after 2 months KWOMAC was similarly significantly improved in both groups. We did not analyze the difference in the items, such as pain, stiffness, and physical function. The change of LSS seemed to be different to KWOMAC. Though there were no statistical difference between WBV and HBE, the mean values of LSS in the WBV group improved consistently from the baseline to 2 months and those in the control group improved only over first 1 month. LSS is composed of 8 different entries and sub-concepts of pain, clinical symptoms, and functional status. Whereas KWOMAC is composed of 24 entries without clinical symptom sub-concept, but has joint stiffness entry in which LSS does not have.
Dynamic balance significantly improved only over the first 1 month in both groups and no statistical difference between the WBV and HBE. Isometric torque of knee extensor and knee flexor improved more than isokinetic torque in each group; therefore, both WBV and HBE might be helpful to improve isometric torque of quadriceps and hamstring, and also improved dynamic balance. If we analyzed the correlation between isometric torque and dynamic balance, we could suggest a more detailed association of these outcomes. Strengthening of quadriceps is important and we could find the strengthening effect of WBV and HBE. The quadriceps muscle acts as a dynamic stabilizer of the knee joint and might have some association with balance. We suggest the possibility that WBV could be helpful to dynamic balance through improvement of isometric torque of the quadriceps muscle.
In this study, both the study group and control group showed improvements of isometric torque of both knee extensors. However, as for the isokinetic torque of knee extensors, both groups showed improvements only in the right side. This result could be due to many different factors. Because most of strengthening exercise of HBE is composed of isometric exercise, the components of HBE could be the cause of significant improvement of isometric torque compared to isokinetic torque. In addition, because of joint stiffness and pain of chronic knee OA patients, the measurement may have not been precise.
The limb dominance may be the cause of improvement of isokinetic torque only in the right side. Limb dominance has been defined as one limb demonstrating increased dynamic control as a result of an imbalance in muscular strength and recruitment patterns [30-32]. In this study, except for 1 patient in the study group, all the other patients were right limb dominance and this could have affected the isokinetic strengthening. However, no study was done about the relationship between the limb dominance and strengthening effect, and further researches are needed.
We set the therapeutic intervention of HBE in the control group. Because of ethical problems, we thought this was the least intervention to patients with knee OA. This was the difference from another study [15], which designed the control group with no therapeutic intervention. If we set the control group with no intervention like the other study, results of this study might have changed to be advantageous over the control group with various measurements.
HBE composed of light strengthening exercise has been known as a good intervention for patients with knee OA. It was reported to be superior to no exercise group over the two years [33], and as effective as the standard physical therapy [34] and hyaluronate injection [35]. Recent ACR guideline strongly recommends that all patients with symptomatic knee have been enrolled in an exercise program commensurate with their ability to perform these activities [3]. Therefore, we suggest that WBV might be valuable therapeutic intervention in knee OA because therapeutic effect of WBV seems to be as effective as HBE, which is proved as effective.
This study has several limitations to the generalization of the results. The sample size was small. The small sample sizes used probably decreased statistical power. The other limitation is long-term measurement of efficacy, and the lack of the control group did not participate in any training and only the WBV treatment group. Lastly, both the study group and control group showed improvements of isokinetic torque of knee extensors only in the right side. To support these results, many probable causes are explained above, but the evidence is yet scarce. Therefore, this point should further be evaluated.
Many studies reported that long-term occupational exposure to intense WBV seems to be associated with an increased risk of low back pain [36-38]. Because the long-term exposure to WBV can lead to muscle fatigue and pathological change of musculoskeletal system [36]. However, short term exposure to WBV has been reported to increase muscle power by improved muscle activation [39]. In our study, adverse events, such as low back pain and aggravation of knee pain, occurred only in one patient in the study group, which is smaller than in the control group. Therefore, we can suggest TurboSonic which seems to be a safe WBV exercise device. However, vesicles on the buttock in one patient, which was diagnosed as herpes zoster, might be not be related to the whole body vibrator due to no reports of herpes zoster after WBV.
In chronic knee OA patients, WBV reduced pain intensity and increased strength of the right quadriceps and performance of dynamic balance. In comparison with HBE program, WBV was superior only in pain reduction and similarly effective in strengthening of the quadriceps muscle and improvement of dynamic balance.
ACKNOWLEDGMENTS
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A090084).
Special thanks to biostatistician (Chi-Yeon Lim, PhD) of the Department of Data Management and Statistics Institute, Dongguk University.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991-94. J Rheumatol. 2006;33:2271–2279. [PubMed] [Google Scholar]
- 2.Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012;64:465–474. doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
- 3.Iwamoto J, Takeda T, Sato Y. Effect of muscle strengthening exercises on the muscle strength in patients with osteoarthritis of the knee. Knee. 2007;14:224–230. doi: 10.1016/j.knee.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Devos-Comby L, Cronan T, Roesch SC. Do exercise and self-management interventions benefit patients with osteoarthritis of the knee? A metaanalytic review. J Rheumatol. 2006;33:744–756. [PubMed] [Google Scholar]
- 5.Tan J, Balci N, Sepici V, Gener FA. Isokinetic and isometric strength in osteoarthrosis of the knee: a comparative study with healthy women. Am J Phys Med Rehabil. 1995;74:364–369. [PubMed] [Google Scholar]
- 6.Hootman JM, FitzGerald SJ, Macera CA, Blair SN. Lower extremity muscle strength and risk of self-reported hip or knee osteoarthritis. J Phys Act Health. 2004;1:321–330. [Google Scholar]
- 7.McAlindon TE, Cooper C, Kirwan JR, Dieppe PA. Determinants of disability in osteoarthritis of the knee. Ann Rheum Dis. 1993;52:258–262. doi: 10.1136/ard.52.4.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kirkley A, Webster-Bogaert S, Litchfield R, Amendola A, MacDonald S, McCalden R, et al. The effect of bracing on varus gonarthrosis. J Bone Joint Surg Am. 1999;81:539–548. doi: 10.2106/00004623-199904000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Barrett DS, Cobb AG, Bentley G. Joint proprioception in normal, osteoarthritic and replaced knees. J Bone Joint Surg Br. 1991;73:53–56. doi: 10.1302/0301-620X.73B1.1991775. [DOI] [PubMed] [Google Scholar]
- 10.Cochrane DJ, Stannard SR. Acute whole body vibration training increases vertical jump and flexibility performance in elite female field hockey players. Br J Sports Med. 2005;39:860–865. doi: 10.1136/bjsm.2005.019950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bogaerts A, Verschueren S, Delecluse C, Claessens AL, Boonen S. Effects of whole body vibration training on postural control in older individuals: a 1 year randomized controlled trial. Gait Posture. 2007;26:309–316. doi: 10.1016/j.gaitpost.2006.09.078. [DOI] [PubMed] [Google Scholar]
- 12.Fagnani F, Giombini A, Di Cesare A, Pigozzi F, Di Salvo V. The effects of a whole-body vibration program on muscle performance and flexibility in female athletes. Am J Phys Med Rehabil. 2006;85:956–962. doi: 10.1097/01.phm.0000247652.94486.92. [DOI] [PubMed] [Google Scholar]
- 13.Cardinale M, Bosco C. The use of vibration as an exercise intervention. Exerc Sport Sci Rev. 2003;31:3–7. doi: 10.1097/00003677-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Cardinale M, Lim J. The acute effects of two different whole body vibration frequencies on vertical jump performance. Med Sport. 2003;56:287–292. [Google Scholar]
- 15.Trans T, Aaboe J, Henriksen M, Christensen R, Bliddal H, Lund H. Effect of whole body vibration exercise on muscle strength and proprioception in females with knee osteoarthritis. Knee. 2009;16:256–261. doi: 10.1016/j.knee.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 16.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fitzgerald GK, Oatis C. Role of physical therapy in management of knee osteoarthritis. Curr Opin Rheumatol. 2004;16:143–147. doi: 10.1097/00002281-200403000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Bae SC, Lee HS, Yun HR, Kim TH, Yoo DH, Kim SY. Cross-cultural adaptation and validation of Korean Western Ontario and McMaster Universities (WOMAC) and Lequesne osteoarthritis indices for clinical research. Osteoarthritis Cartilage. 2001;9:746–750. doi: 10.1053/joca.2001.0471. [DOI] [PubMed] [Google Scholar]
- 19.Bosco C, Cardinale M, Tsarpela O, Colli R, Tihanyi J, von Duvillard SP, et al. The influence of whole body vibration on jumping ability. Biol Sport. 1998;15:157–164. [Google Scholar]
- 20.Bosco C, Colli R, Introini E, Cardinale M, Tsarpela O, Madella A, et al. Adaptive responses of human skeletal muscle to vibration exposure. Clin Physiol. 1999;19:183–187. doi: 10.1046/j.1365-2281.1999.00155.x. [DOI] [PubMed] [Google Scholar]
- 21.Torvinen S, Kannu P, Sievanen H, Jarvinen TA, Pasanen M, Kontulainen S, et al. Effect of a vibration exposure on muscular performance and body balance: randomized cross-over study. Clin Physiol Funct Imaging. 2002;22:145–152. doi: 10.1046/j.1365-2281.2002.00410.x. [DOI] [PubMed] [Google Scholar]
- 22.Nigg BM. Impact forces in running. Curr Opin Orthop. 1997;8:43–47. [Google Scholar]
- 23.De Gail P, Lance JW, Neilson PD. Differential effects on tonic and phasic reflex mechanisms produced by vibration of muscles in man. J Neurol Neurosurg Psychiatry. 1966;29:1–11. doi: 10.1136/jnnp.29.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Issurin VB, Liebermann DG, Tenenbaum G. Effect of vibratory stimulation training on maximal force and flexibility. J Sports Sci. 1994;12:561–566. doi: 10.1080/02640419408732206. [DOI] [PubMed] [Google Scholar]
- 25.Lundstrom RJ. Responses of mechanoreceptive afferent units in the glabrous skin of the human hand to vibration. Scand J Work Environ Health. 1986;12(4 Spec No):413–416. [PubMed] [Google Scholar]
- 26.Talbot WH, Darian-Smith I, Kornhuber HH, Mountcastle VB. The sense of flutter-vibration: comparison of the human capacity with response patterns of mechanoreceptive afferents from the monkey hand. J Neurophysiol. 1968;31:301–334. doi: 10.1152/jn.1968.31.2.301. [DOI] [PubMed] [Google Scholar]
- 27.Bensmaia SJ, Leung YY, Hsiao SS, Johnson KO. Vibratory adaptation of cutaneous mechanoreceptive afferents. J Neurophysiol. 2005;94:3023–3036. doi: 10.1152/jn.00002.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leung YY, Bensmaia SJ, Hsiao SS, Johnson KO. Time-course of vibratory adaptation and recovery in cutaneous mechanoreceptive afferents. J Neurophysiol. 2005;94:3037–3045. doi: 10.1152/jn.00001.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hollins M, Roy EA. Perceived intensity of vibrotactile stimuli: the role of mechanoreceptive channels. Somatosens Mot Res. 1996;13:273–286. doi: 10.3109/08990229609052583. [DOI] [PubMed] [Google Scholar]
- 30.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35:1745–1750. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 31.Hewett TE, Myer GD, Ford KR. Prevention of anterior cruciate ligament injuries. Curr Womens Health Rep. 2001;1:218–224. [PubMed] [Google Scholar]
- 32.Knapik JJ, Bauman CL, Jones BH, Harris JM, Vaughan L. Preseason strength and flexibility imbalances associated with athletic injuries in female collegiate athletes. Am J Sports Med. 1991;19:76–81. doi: 10.1177/036354659101900113. [DOI] [PubMed] [Google Scholar]
- 33.Thomas KS, Muir KR, Doherty M, Jones AC, O'Reilly SC, Bassey EJ. Home based exercise programme for knee pain and knee osteoarthritis: randomised controlled trial. BMJ. 2002;325:752. doi: 10.1136/bmj.325.7367.752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ben Salah Frih Z, Fendri Y, Jellad A, Boudoukhane S, Rejeb N. Efficacy and treatment compliance of a home-based rehabilitation programme for chronic low back pain: a randomized, controlled study. Ann Phys Rehabil Med. 2009;52:485–496. doi: 10.1016/j.rehab.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 35.Kawasaki T, Kurosawa H, Ikeda H, Takazawa Y, Ishijima M, Kubota M, et al. Therapeutic home exercise versus intraarticular hyaluronate injection for osteoarthritis of the knee: 6-month prospective randomized open-labeled trial. J Orthop Sci. 2009;14:182–191. doi: 10.1007/s00776-008-1312-9. [DOI] [PubMed] [Google Scholar]
- 36.Seidel H, Heide R. Long-term effects of whole-body vibration: a critical survey of the literature. Int Arch Occup Environ Health. 1986;58:1–26. doi: 10.1007/BF00378536. [DOI] [PubMed] [Google Scholar]
- 37.Dupuis H, Zerlett G. Whole-body vibration and disorders of the spine. Int Arch Occup Environ Health. 1987;59:323–336. doi: 10.1007/BF00405276. [DOI] [PubMed] [Google Scholar]
- 38.Hulshof C, van Zanten BV. Whole-body vibration and low-back pain: a review of epidemiologic studies. Int Arch Occup Environ Health. 1987;59:205–220. doi: 10.1007/BF00377733. [DOI] [PubMed] [Google Scholar]
- 39.Cochrane DJ, Legg SJ, Hooker MJ. The short-term effect of whole-body vibration training on vertical jump, sprint, and agility performance. J Strength Cond Res. 2004;18:828–832. doi: 10.1519/14213.1. [DOI] [PubMed] [Google Scholar]