Abstract
Objective
To investigate the therapeutic effect of neurologic music therapy (NMT) and speech language therapy (SLT) through improvement of the aphasia quotient (AQ) in post-stroke aphasic patients.
Methods
Twenty-one post-stroke, nonfluent aphasia patients who had ischemic/hemorrhagic stroke on radiologic evaluation were divided into the NMT and SLT groups. They received NMT and SLT for 1 month. Language function was assessed by Korean version-Western Aphasia Battery before and after therapy. NMT consisted of therapeutic singing and melodic intonation therapy, and SLT consisted of language-oriented therapy.
Results
Significant improvements were revealed in AQ, repetition, and naming after therapy in the NMT group and improvements in repetition in the SLT group of chronic stroke patients (p<0.05). There were significant improvements in language ability in the NMT group of subacute stroke patients. However, there was no significant improvement in the SLT group of subacute stroke patients.
Conclusion
We concluded that the two therapies are effective treatments in the chronic stage of stroke and NMT is effective in subacute post-stroke aphasic patients.
Keywords: Stroke, Aphasia, Music therapy, Speech therapy
INTRODUCTION
Language impairment in adults caused by injury to the central nervous system are on the increase due to improvements in stroke treatment and extension of life span made possible by the development of medical technologies [1]. Aphasia after stroke is reported to occur in 43 to 60 out of 100,000 people in Europe and United States, and the frequency is becoming higher as the number of elderly people is on the increase [1]. Aphasia is a common complication after stroke affecting the left middle cerebral artery, and is recognized as a major impairment by patients and their family members [2]. The types of aphasia can be roughly divided into fluent and nonfluent; fluent aphasia reduces understanding of language and nonfluent reduces expressive skills of language [3]. Broca's aphasia, as a representative type of nonfluent aphasia, shows favorable auditory understanding but difficulty in expression; patients speak in short sentences or mainly speak content words without using postpositions or function words [3]. Nonfluent aphasia is caused by injury to the left frontal lobe including Broca's area, and recently it was reported that injury to the subcortical area and the area around the inferior Rolandic area induced similar symptoms [3]. Some studies reported that nonfluent aphasia with severe left brain injury did not show a favorable course by natural healing and showed less response to traditional speech therapy [4].
Speech therapy has been used to treat aphasia [5], and it was reported that intensive language-action therapy as a speech therapy improved language performance of patients with chronic aphasia [4]. Language-oriented treatment is another component of speech therapy, and consists of training the patient to understand the contents of the program by using the auditory sense, expression training via using spoken language, and training of expression using pictures of texts. Melodic intonation therapy (MIT) has been used for severe aphasiac patients with rare voluntary speaking as a method of inducing speech using musical tones or rhythm that stimulate functions of the nondominant hemisphere [6]. Visual action therapy is effective in global aphasia [7], and word retrieval therapy is a method of therapy in which semantic and phonemic cues are presented. Some researchers reported that repetitive transcranial magnetic stimulation [8], cholinergic agents, and N-methyl-D-aspartate (NMDA) might be helpful in speech therapy [9].
Neurologic music therapy (NMT) is a method of music therapy for improving the cognitive, sensory, and motor functions impaired by neurological diseases, and some researchers reported that the therapy involved the patients understanding the music through stimulation of their cognitive, emotional, and sensorimotor functions [10]. The NMT applied in this study consisted of therapeutic singing and MIT. MIT is a type of reorganization language rehabilitation using uninjured non-verbal functions (melody, tones, etc.) of the brain. The patients are encouraged to say words, sentences or short phrases by using unfamiliar melody patterns, and the length of the target utterance is gradually extended by inducing speech as a form of a song in which the melodies are combined [11].
There are reports comparing MIT and simple language therapy for nonfluent aphasia caused by brain lesions, but the results of these studies are limited because of the small size of the therapy group [12]. In this context, the authors compared and analyzed changes in aphasia indicators in the group of patients with nonfluent aphasia who received therapeutic singing and MIT and in the group of patients who received language-oriented treatment, to investigate the neurologic effects between the two language therapies.
MATERIALS AND METHODS
Subjects
The subjects of this study were patients with stroke who were hospitalized in two university hospitals between January 2007 and May 2011. Among the patients with bleeding and infarction in the cerebral hemisphere on magnetic resonance imaging (MRI) and computed tomography, 21 of them who were diagnosed as having nonfluent aphasia using the Korean version-Western Aphasia Battery (K-WAB) [13], and these patients were selected to be the subjects of this study. Patients with a history of language impairment before the cerebral hemorrhage, and those who had neurological disorders other than stroke of the cerebral hemisphere, and those who had oral apraxia were excluded.
Therapy
The patients in the department of rehabilitation medicine of one university hospital had one-on-one therapy from the speech therapists of the hospital and neurologic music therapy consisting of therapeutic singing and MIT, as the NMT group. The patients in the department of rehabilitation medicine of the other university hospital had one-on-one therapy from the speech therapists of the hospital and language-oriented treatment, as the speech language therapy (SLT) group.
The NMT group received treatment consisting of therapeutic singing and MIT, which consisted of melody intonation and rhythmic left-hand slapping. Therapeutic singing included respiratory training, voice training, and automated singing via familiar songs, and automated speech training. The patients underwent respiratory training by doing exercises involving abdominal breathing, using a wind instrument, and whistling, and voice training to say 'ah.' The therapists sang a familiar song first and then the patients sang it after them, and the patients had training in saying sentences of the 'noun+verb' type by using melody. As for the MIT, the therapists determined a target word and phrase with the patients and induced speech from the patients by defining tones of specific syllables or word-phrases and by setting up melodies. The patients were asked to beat time with the uninjured hand and then to follow the beat by presenting rhythm patterns with drums or pictures.
The SLT group underwent language-oriented treatment consisting of understanding the contents of the program via the visual and auditory senses, expression training via spoken language, and training of expression via pictures of texts. The therapists presented the stimulation and then the patients responded to it, and without repeating the same stimulation until a correct response was given, different stimulations were presented to induce a response. The patients underwent automated spoken expression training in which automated or mechanically used words were induced for expression training via the spoken language, pictures or texts, articulation training using various types of consonants, vowels, syllables, and words, and then they were asked to follow three consecutive words presented by the therapists. The patients underwent training in which they read sentences aloud that corresponded to pictures shown by the therapists, produced words by using phonemic stimulations, made sentences from presented pictures, or talked about what they did the previous day. Both groups were given treatment for 60 minutes a day two times a week for a month.
Method
The K-WAB published by the Paradise Welfare Foundation was used to assess aphasia. The K-WAB is roughly divided into three domains: the first part is oral language, consisting of four sub-tests such as spontaneous speaking, understanding, repetition, and naming; the second part is written language including a reading and writing test; the third part covers other cognitive functions consisting of action, construct, visual space, and calculation tests. We assessed oral language in this study; spontaneous speaking contained a total of 20 points of content delivery and fluency. Understanding contained a total of 200 points of a yes/no test, auditory word recognition, and execution of orders. Repetition was a total of 100 points, and naming contained a total of 100 points and comprised the naming of objects, reminding of control words, completing sentences, and sentence answering. The aphasia quotient (AQ) reflecting the four items was a total of 100 points.
The K-WAB was applied before and after each session of speech therapy. The AQ and improvement in detailed items were compared in order to compare and analyze the therapeutic effects of each group.
Statistics
After one month of therapy, we evaluated changes in the AQ and scores of spontaneous speaking, understanding, repetition, and naming of each group for comparing and analyzing. The changed values of the K-WAB of the two groups were analyzed by using the Mann-Whitney U test, and the Wilcoxon signed-rank test was used in order to evaluate improvements in the K-WAB items within a group. The SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis, and p<0.05 was considered statistically significant.
RESULTS
A total of 21 patients participated in this study; 12 of them were in the NMT group and 9 were in the SLT group. Because there were differences in the period from stroke to treatment within the two groups, the subjects whose period between stroke and treatment was three months or less were placed in the subacute group and those with at least 180 days between stroke and treatment were put in the chronic group, making a total of four groups in this study. As for the chronic patients, there were no significant differences in ages and the period until treatment between the NMT and the SLT groups. In the NMT-chronic group, four had brain hemorrhage, two had cerebral infarction, three had right cerebral injury, and three had left cerebral injury. In the SLT-chronic group, all five patients had left cerebral hemorrhage (Table 1). As for the subacute patients, there were no significant differences in ages and the period until treatment between the NMT and the SLT groups. In the NMT-subacute group, five had brain hemorrhage, one had cerebral infarction, two had right cerebral injury, and four had left cerebral injury. In the SLT-subacute group, all four patients had left cerebral hemorrhage (Table 1).
Table 1.
General characteristics of subjects
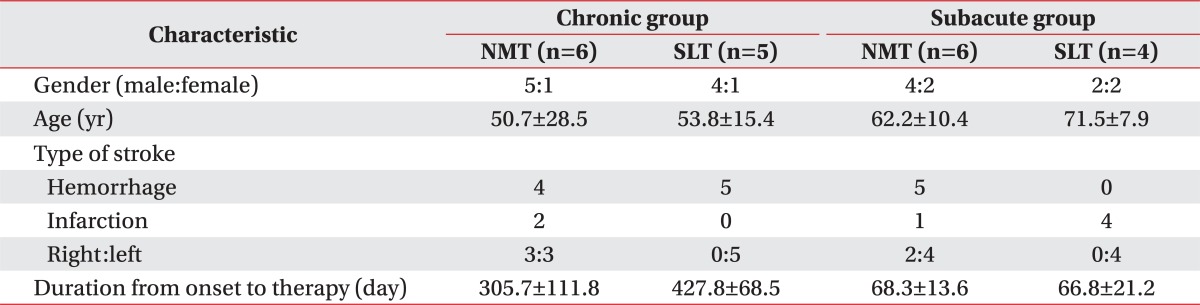
Values are presented as mean±standard deviation.
NMT, neurologic music therapy; SLT, speech language therapy.
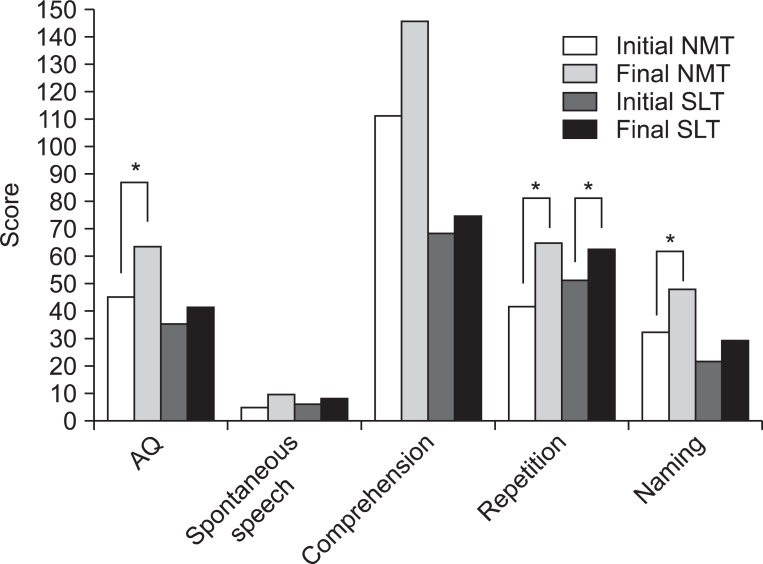
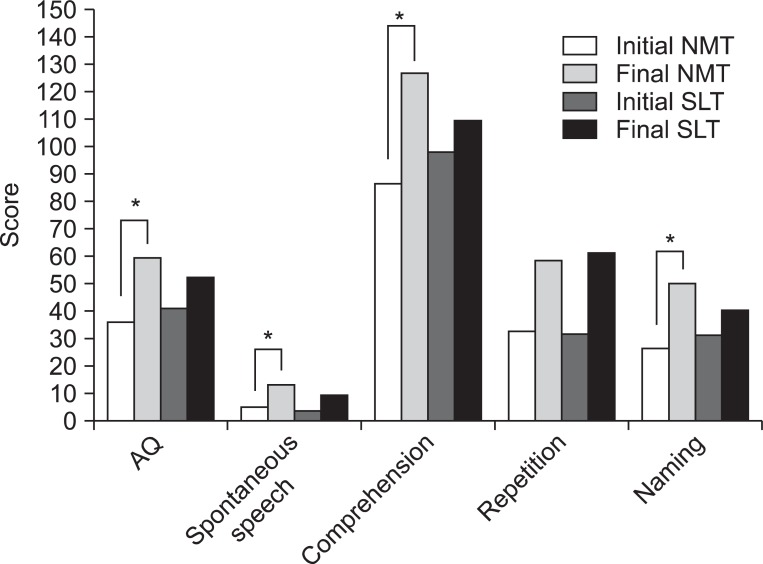
There was no significant difference between the NMT-chronic and the SLT-chronic groups when the changed values in which the initial values and the latter values of the K-WAB items in the chronic period were subtracted were compared between the two groups (Table 2). When the changed values of the two subacute groups were compared between the two groups, no significant difference was shown between the NMT-subacute and the SLT-subacute groups (Table 3). When the initial and the latter values within the NMT-chronic group were compared, significant improvements were shown in AQ, spontaneous speaking, repletion, and naming. In the SLT-chronic group, repletion showed significant improvement (Fig. 1). When the initial and the latter values within the NMT-subacute group were compared, significant improvements were shown in AQ, spontaneous speaking, understanding, and naming. In the SLT-subacute group, no significant improvement was shown in any detailed item (Fig. 2).
Table 2.
K-WAB score differences before and after NMT- or SLT-chronic group
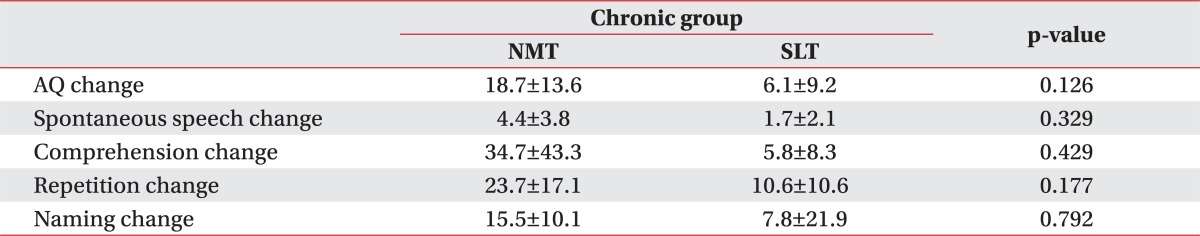
Values are presented as mean±standard deviation.
p<0.05 from the Mann-Whitney test.
K-WAB, Korean version-Western Aphasia Battery; NMT, neurologic music therapy; SLT, speech language therapy; AQ, aphasia quotient.
Table 3.
K-WAB score differences before and after NMT- or SLT-subacute group
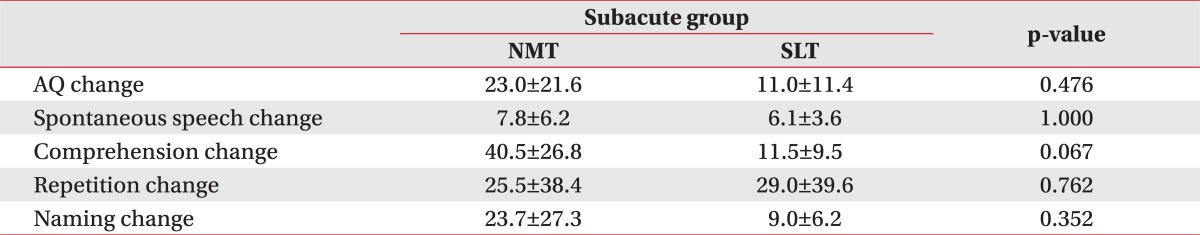
Values are presented as mean±standard deviation.
p<0.05 from the Mann-Whitney test.
K-WAB, Korean version-Western Aphasia Battery; NMT, neurologic music therapy; SLT, speech language therapy; AQ, aphasia quotient.
Fig. 1.
The Korean version-Western Aphasia Battery values within the neurologic music therapy (NMT)-chronic and speech language therapy (SLT)-chronic group. AQ, aphasia quotient. *p<0.05 (comparison of the initial vs. final values after NMT or SLT).
Fig. 2.
The Korean version-Western Aphasia Battery values within the neurologic music therapy (NMT)-subacute and speech language therapy (SLT)-subacute group. AQ, aphasia quotient. *p<0.05 (comparison of the initial vs. final values after NMT or SLT).
DISCUSSION
The authors compared and analyzed the therapeutic effects of NMT using expressive training, and the therapeutic effects of MIT with SLT using expressive training involving speech and pictures or texts for nonfluent aphasia caused by stroke to ascertain whether both methods were therapeutically effective for chronic nonfluent aphasia. NMT was effective in patients with subacute nonfluent aphasia.
The therapeutic mechanisms of NMT operate by stimulating the speaking pathway in the left cerebral hemisphere or the singing pathway in the right side of both cerebral hemispheres [14,15]. It has been reported that both cerebral hemispheres play a role in executing vocal cord production and controlling sensorimotor functions in both speaking and singing, and that the left hemisphere is used more in speaking [16,17]. Hypotheses explaining the effectiveness of music therapy for aphasia include the fact that words can be pronounced more slowly in singing than in speaking. Also, singing can present more opportunities for distinguishing phonemes that consist of words and phrases due to the length of syllables, and nonfluent aphasic patients may become more fluent by slow singing of connected segments. The rhythmic characteristics such as intonation, tones, and syllable accent may be helpful in speaking words and words as phrases, and chunking may activate the right cerebral hemisphere. Lastly, rhythmic tapping may activate the sensorimotor network of the cerebral hemisphere, promoting phrase generation [18]. Also, auditory motor function can be improved by sound generation from left-hand clapping due to shared nervous connections controlling both hand movements and movements of the mouth in pronunciation [19].
Language-oriented therapy programs are constructed on the assumption that the aphasiac patient is injured not only in the pathway that gives access to the language system but in the language system itself. In other words, the programs take into consideration that the aphasiac patient is impaired in at least one aspect of language (phonologic, semantic, and phrasal) and give treatment that improves efficiency in verbal information processing.
Because the language system of the patient is impaired, therapies should target the impaired language mode and maintain the proper difficulty level based on the degrees of the injury. The mechanisms should enhance efficiency of verbal processing to increase the functions of language therapy to the maximum, reorganize tissues, and stimulate the brain areas corresponding to the injured areas so that these parts conduct the functions that were performed by the injured areas [20].
The group of chronic patients with nonfluent aphasia treated by NMT showed significant increase in the latter K-WAB values when compared to the initial values, and their AQ, repetition, and understanding were significantly enhanced. The chronic group treated by SLT showed a significant increase in repetition only. The subacute group treated by NMT showed significant improvements in AQ, spontaneous speaking, understanding, and naming (in the latter values rather than in the initial values). The subacute group treated by SLT showed no improvement in any detained item. The results of this study may indicate that both therapies are effective in chronic nonfluent aphasia and that NMT improves language functions of patients with subacute nonfluent aphasia.
Koelsch et al. [21] reported that the expression of sensory factors in music and language are separate functions or conducted by other areas. Schlaug et al. [12] observed that the right cerebrum including the right posterior middle premotor cortex, the right inferior frontal gyrus, and the posterior superior temporal gyrus were activated on functional MRI after Broca's aphasia patients were given therapy with MIT. After therapy with SLT, it was reported that the right premotor/motor areas of brain and temporal lobe and left posterior perisylvian region were activated [12]. Such results may indicate that there are other pathways involved in speaking and singing, and that both therapies may be effective in the treatment of aphasia by activating the cerebrum via different pathways.
This study may be limited in that the number of subjects was small, the ages of the subjects were uneven, and the number of educational years before the onset of stroke and difference in cognitive functions before therapy were not considered. Also, because the K-WAB scores were applied to selected nonfluent aphasic patients, the NMT group had patients with both right and left cerebral lesions but the SLT group had only left cerebral lesions, a fact that might affect the results of this study. There are some more limitations: the therapies were applied in two university hospitals and were not conducted by one therapist; the treatment period was short (one month); and the catamnesis of language therapy was not considered. Further studies to compensate for such limitations may be needed.
In conclusion, the purpose of this study was to compare and analyze the therapeutic effects of NMT and SLT on nonfluent aphasic stroke patients to assess the clinical values and to contribute to the planning of rehabilitation of aphasia patients. Both the NMT and SLT groups of chronic nonfluent aphasia showed significant therapeutic effects, and as for subacute nonfluent aphasia, the NMT group showed significant effects. NMT and the SLT were shown to have therapeutic effects on nonfluent aphasia, but no definite conclusions about the differences in the effects between the two can be made because of the limitations in this study. Future well-designed controlled studies are required.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Engelter ST, Gostynski M, Papa S, Frei M, Born C, Ajdacic-Gross V, et al. Epidemiology of aphasia attributable to first ischemic stroke: incidence, severity, fluency, etiology, and thrombolysis. Stroke. 2006;37:1379–1384. doi: 10.1161/01.STR.0000221815.64093.8c. [DOI] [PubMed] [Google Scholar]
- 2.Wade DT, Wood VA, Hewer RL. Recovery after stroke: the first 3 months. J Neurol Neurosurg Psychiatry. 1985;48:7–13. doi: 10.1136/jnnp.48.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walker-Batson D, Avent JR. Adult neurogenic communication disorders. In: Braddom RL, editor. Physical medicine and rehabilitation. 3rd ed. Philadelphia: Saunders; 2007. pp. 49–62. [Google Scholar]
- 4.Berthier ML, Pulvermuller F. Neuroscience insights improve neurorehabilitation of poststroke aphasia. Nat Rev Neurol. 2011;7:86–97. doi: 10.1038/nrneurol.2010.201. [DOI] [PubMed] [Google Scholar]
- 5.Berthier ML. Poststroke aphasia: epidemiology, pathophysiology and treatment. Drugs Aging. 2005;22:163–182. doi: 10.2165/00002512-200522020-00006. [DOI] [PubMed] [Google Scholar]
- 6.Sparks RW, Holland AL. Method: melodic intonation therapy for aphasia. J Speech Hear Disord. 1976;41:287–297. doi: 10.1044/jshd.4103.287. [DOI] [PubMed] [Google Scholar]
- 7.Helm-Estabrooks N, Fitzpatrick PM, Barresi B. Visual action therapy for global aphasia. J Speech Hear Disord. 1982;47:385–389. doi: 10.1044/jshd.4704.385. [DOI] [PubMed] [Google Scholar]
- 8.Lee JH, Yoo WK, Jung KI, Kim DH, Park DS, Im HJ. The therapeutic effect of inhibitory repetitive transcranial magnetic stimulation on right inferior frontal gyrus in subcortical aphasia. J Korean Acad Rehabil Med. 2007;31:70–77. [Google Scholar]
- 9.Berthier ML, Hinojosa J, Martin Mdel C, Fernandez I. Open-label study of donepezil in chronic poststroke aphasia. Neurology. 2003;60:1218–1219. doi: 10.1212/01.wnl.0000055871.82308.41. [DOI] [PubMed] [Google Scholar]
- 10.Thaut MH, Gardiner JC, Holmberg D, Horwitz J, Kent L, Andrews G, et al. Neurologic music therapy improves executive function and emotional adjustment in traumatic brain injury rehabilitation. Ann N Y Acad Sci. 2009;1169:406–416. doi: 10.1111/j.1749-6632.2009.04585.x. [DOI] [PubMed] [Google Scholar]
- 11.Belin P, Van Eeckhout P, Zilbovicius M, Remy P, Francois C, Guillaume S, et al. Recovery from nonfluent aphasia after melodic intonation therapy: a PET study. Neurology. 1996;47:1504–1511. doi: 10.1212/wnl.47.6.1504. [DOI] [PubMed] [Google Scholar]
- 12.Schlaug G, Marchina S, Norton A. From singing to speaking: why singing may lead to recovery of expressive language function in patients with Broca's aphasia. Music Percept. 2008;25:315–323. doi: 10.1525/MP.2008.25.4.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim HH, Na DL. Paradise Korean version the Western Aphasia Battery. Seoul: Paradise Welfare Foundation; 2001. [Google Scholar]
- 14.Bohland JW, Guenther FH. An fMRI investigation of syllable sequence production. Neuroimage. 2006;32:821–841. doi: 10.1016/j.neuroimage.2006.04.173. [DOI] [PubMed] [Google Scholar]
- 15.Brown S, Martinez MJ, Hodges DA, Fox PT, Parsons LM. The song system of the human brain. Brain Res Cogn Brain Res. 2004;20:363–375. doi: 10.1016/j.cogbrainres.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 16.Guenther FH, Hampson M, Johnson D. A theoretical investigation of reference frames for the planning of speech movements. Psychol Rev. 1998;105:611–633. doi: 10.1037/0033-295x.105.4.611-633. [DOI] [PubMed] [Google Scholar]
- 17.Jeffries KJ, Fritz JB, Braun AR. Words in melody: an H(2)15O PET study of brain activation during singing and speaking. Neuroreport. 2003;14:749–754. doi: 10.1097/00001756-200304150-00018. [DOI] [PubMed] [Google Scholar]
- 18.Thaut MH, Kenyon GP, Schauer ML, McIntosh GC. The connection between rhythmicity and brain function. IEEE Eng Med Biol Mag. 1999;18:101–108. doi: 10.1109/51.752991. [DOI] [PubMed] [Google Scholar]
- 19.Lahav A, Saltzman E, Schlaug G. Action representation of sound: audiomotor recognition network while listening to newly acquired actions. J Neurosci. 2007;27:308–314. doi: 10.1523/JNEUROSCI.4822-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kelly H, Brady MC, Enderby P. Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev. 2010;(5):CD000425. doi: 10.1002/14651858.CD000425.pub2. [DOI] [PubMed] [Google Scholar]
- 21.Koelsch S, Gunter TC, von Cramon DY, Zysset S, Lohmann G, Friederici AD. Bach speaks: a cortical "language-network" serves the processing of music. Neuroimage. 2002;17:956–966. [PubMed] [Google Scholar]